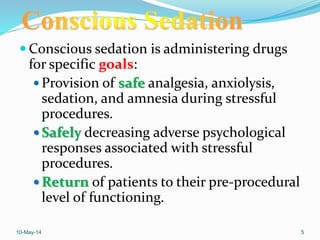
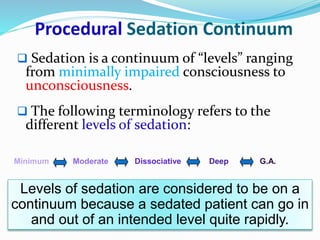
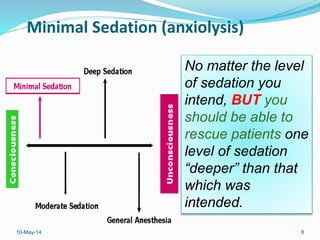
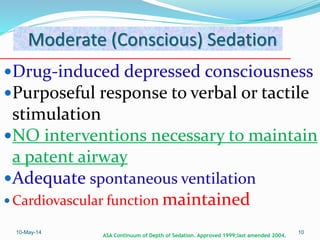
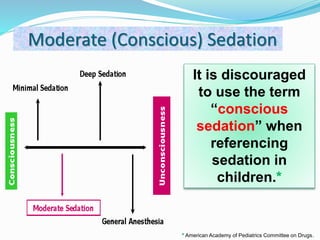
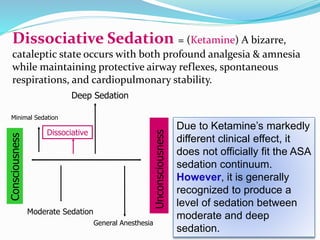
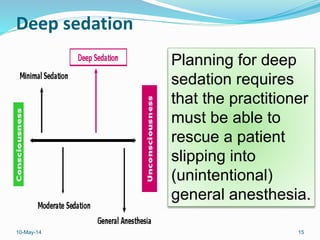
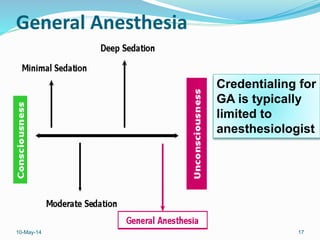
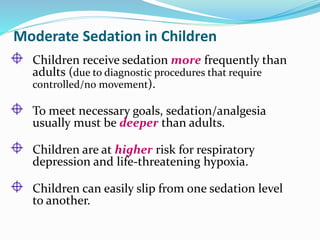
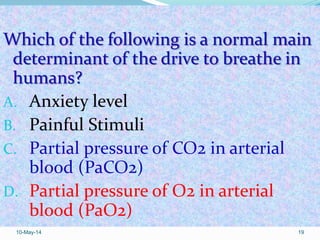
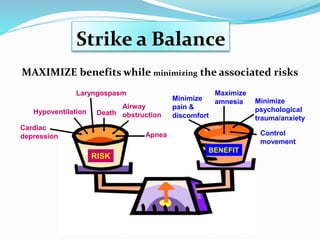
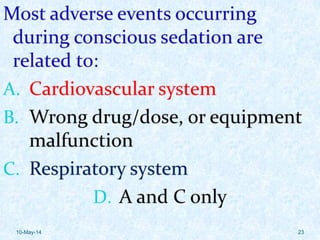
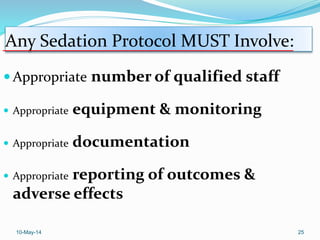
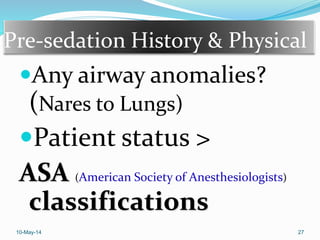
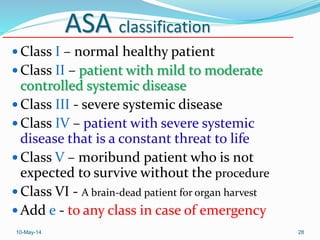
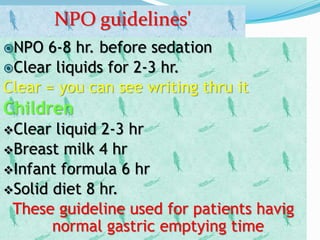
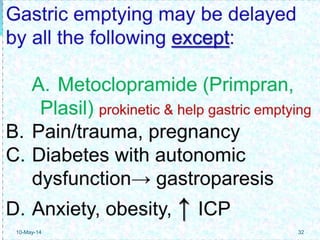
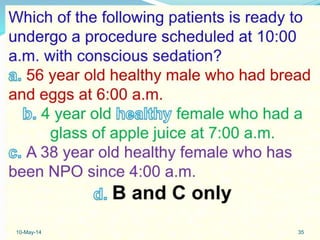
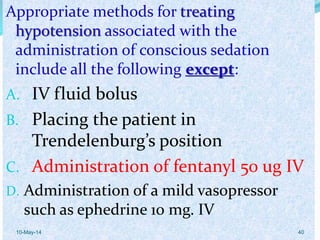
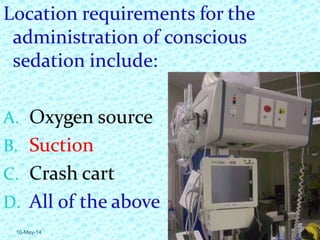
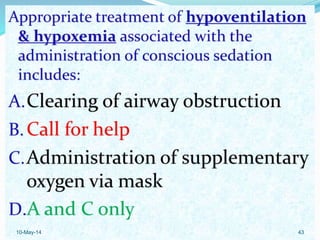
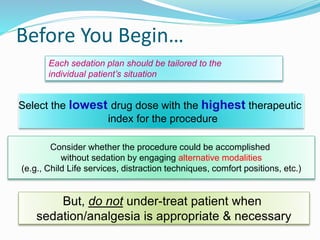
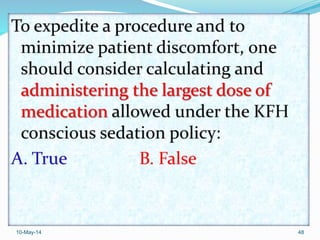
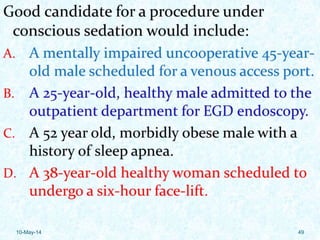
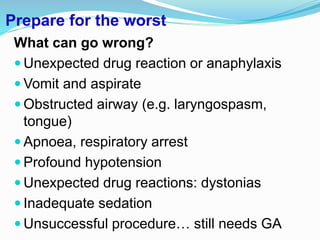
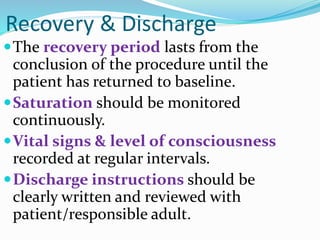
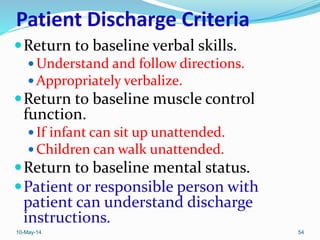
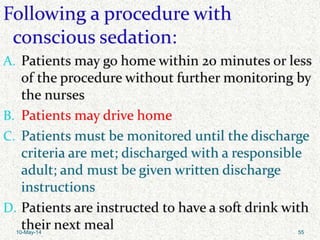
The document outlines a mandatory course on conscious sedation, focusing on its terminology, pharmacology, and patient management. It describes the continuum of sedation levels, indications for use, and guidelines for safe practice, particularly in children who require deeper sedation. Key components include appropriate documentation, monitoring, and recovery protocols to ensure patient safety and positive experiences.