Burn And Scald
•Download as PPT, PDF•
82 likes•38,726 views
Report
Share
Report
Share
More Related Content
What's hot
What's hot (20)
First aid for patients with Wound, Hemorrhage.pptx

First aid for patients with Wound, Hemorrhage.pptx
Viewers also liked
Viewers also liked (20)
Dr.senthil sailesh- Wound debridement,open fracture,evidence based,

Dr.senthil sailesh- Wound debridement,open fracture,evidence based,
ortho 01 management of open fracture-update by kk 31052010

ortho 01 management of open fracture-update by kk 31052010
Similar to Burn And Scald
Similar to Burn And Scald (20)
evaluation and management of patient presenting with Burn.pptx

evaluation and management of patient presenting with Burn.pptx
Recently uploaded
Models Call Girls In Hyderabad 9630942363 Hyderabad Call Girl & Hyderabad Esc...

Models Call Girls In Hyderabad 9630942363 Hyderabad Call Girl & Hyderabad Esc...GENUINE ESCORT AGENCY
Pondicherry Call Girls Book Now 9630942363 Top Class Pondicherry Escort Servi...

Pondicherry Call Girls Book Now 9630942363 Top Class Pondicherry Escort Servi...GENUINE ESCORT AGENCY
Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7![Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
![Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X79953056974 Low Rate Call Girls In Saket, Delhi NCR
Recently uploaded (20)
Low Rate Call Girls Bangalore {7304373326} ❤️VVIP NISHA Call Girls in Bangalo...

Low Rate Call Girls Bangalore {7304373326} ❤️VVIP NISHA Call Girls in Bangalo...
Top Rated Hyderabad Call Girls Erragadda ⟟ 9332606886 ⟟ Call Me For Genuine ...

Top Rated Hyderabad Call Girls Erragadda ⟟ 9332606886 ⟟ Call Me For Genuine ...
9630942363 Genuine Call Girls In Ahmedabad Gujarat Call Girls Service

9630942363 Genuine Call Girls In Ahmedabad Gujarat Call Girls Service
Call Girls Service Jaipur {9521753030} ❤️VVIP RIDDHI Call Girl in Jaipur Raja...

Call Girls Service Jaipur {9521753030} ❤️VVIP RIDDHI Call Girl in Jaipur Raja...
Call Girls Hosur Just Call 9630942363 Top Class Call Girl Service Available

Call Girls Hosur Just Call 9630942363 Top Class Call Girl Service Available
Premium Bangalore Call Girls Jigani Dail 6378878445 Escort Service For Hot Ma...

Premium Bangalore Call Girls Jigani Dail 6378878445 Escort Service For Hot Ma...
Models Call Girls In Hyderabad 9630942363 Hyderabad Call Girl & Hyderabad Esc...

Models Call Girls In Hyderabad 9630942363 Hyderabad Call Girl & Hyderabad Esc...
Top Quality Call Girl Service Kalyanpur 6378878445 Available Call Girls Any Time

Top Quality Call Girl Service Kalyanpur 6378878445 Available Call Girls Any Time
Independent Call Girls In Jaipur { 8445551418 } ✔ ANIKA MEHTA ✔ Get High Prof...

Independent Call Girls In Jaipur { 8445551418 } ✔ ANIKA MEHTA ✔ Get High Prof...
Pondicherry Call Girls Book Now 9630942363 Top Class Pondicherry Escort Servi...

Pondicherry Call Girls Book Now 9630942363 Top Class Pondicherry Escort Servi...
(Low Rate RASHMI ) Rate Of Call Girls Jaipur ❣ 8445551418 ❣ Elite Models & Ce...

(Low Rate RASHMI ) Rate Of Call Girls Jaipur ❣ 8445551418 ❣ Elite Models & Ce...
Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7![Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
![Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7
Call Girl In Pune 👉 Just CALL ME: 9352988975 💋 Call Out Call Both With High p...

Call Girl In Pune 👉 Just CALL ME: 9352988975 💋 Call Out Call Both With High p...
Coimbatore Call Girls in Coimbatore 7427069034 genuine Escort Service Girl 10...

Coimbatore Call Girls in Coimbatore 7427069034 genuine Escort Service Girl 10...
Jogeshwari ! Call Girls Service Mumbai - 450+ Call Girl Cash Payment 90042684...

Jogeshwari ! Call Girls Service Mumbai - 450+ Call Girl Cash Payment 90042684...
Call Girls Madurai Just Call 9630942363 Top Class Call Girl Service Available

Call Girls Madurai Just Call 9630942363 Top Class Call Girl Service Available
Manyata Tech Park ( Call Girls ) Bangalore ✔ 6297143586 ✔ Hot Model With Sexy...

Manyata Tech Park ( Call Girls ) Bangalore ✔ 6297143586 ✔ Hot Model With Sexy...
Call Girls Service Jaipur {8445551418} ❤️VVIP BHAWNA Call Girl in Jaipur Raja...

Call Girls Service Jaipur {8445551418} ❤️VVIP BHAWNA Call Girl in Jaipur Raja...
Call Girls Jaipur Just Call 9521753030 Top Class Call Girl Service Available

Call Girls Jaipur Just Call 9521753030 Top Class Call Girl Service Available
8980367676 Call Girls In Ahmedabad Escort Service Available 24×7 In Ahmedabad

8980367676 Call Girls In Ahmedabad Escort Service Available 24×7 In Ahmedabad
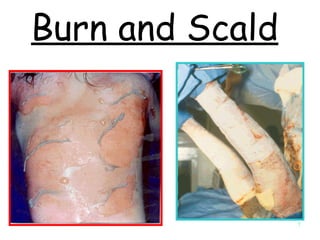
Burn And Scald
- 14. 1° burn 2° burn
- 15. Superficial burn (1° burn)
- 18. Blister may ↑size because continuous exudation and collection of tissue fluid
- 20. 3° burn
- 21. Eschar:composed of denatured protein
- 27. Zon of injury
- 28. Thermal injury Inflammation Vasodilatation & ↑blood flow Leukocyctes & nutrient promote healing Vasoactive substance
- 34. Burn Shock First 24 hours Burn Shock after 24 hours
- 35. Thermal injury Inflammation Histamine release Vasoconstriction ↑ blood pressure ↑ blood flow to injury ↑ capillary permeability Fluids leakage and Loss from injury Site (edema) ↓ intravascular fluid Hypovolemic shock ↑ Protein leakage Hypoproteinemia ↓ Plasma osmotic pressure
- 48. Myoglobinuria
- 53. Rule of nines
- 56. Lund and Browder chart 3½ 3¼ 3 2¾ 2½ 2½ C-1 leg (back or front) 4¾ 4½ 4¼ 4 3¼ 2¾ B-1 thigh (back or front) 3½ 4½ 5½ 6½ 8½ 9½ A-head (back or front) Adult 15 10 5 1 0 Age in years
- 66. ER Assessment History Physical examination Intravenous line Nasogastric tube Indwelling catheter Neurological assessment Vital signs
- 72. Pulse oximeter
- 75. Arterial blood gases *To assess acid-base balance due to a respiratory disorder, respiratory acidosis . 75-100mmHg PO 35-45 mmHg PCO2 ↑ 7.35-7.45 PH ↓
- 81. Diagnostic test Swabs for culture &sensitivity Daily urea , electrolytes Daily FBC ABGs PCV until stable Later Urinalysis ABGs Grouping & typing Carboxyhemoglobin Blood sugar ECG Urea & electrolytes CXR Full Blood Count Optional Essential Initial
- 93. Crystalloid Solutions 273 308 289 Osmolality (mosm/kg) 6.7 5.7 7.4 pH mEq/L Lactate (28) -- Bicarb. (26) Buffer mEq/L 3/0 -- 5/2 Ca/Mg mEq/L 4 -- 4-5 K mEq/L 109 154 103 Cl mEq/L 130 154 141 Na Ringer’s lactate 0.9% Saline Plasma
- 104. Burn victim
- 105. Endotracheal tube
- 106. Tracheostomy