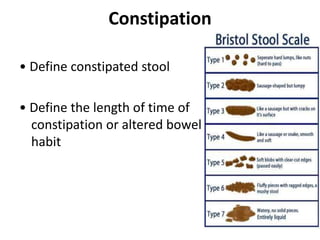
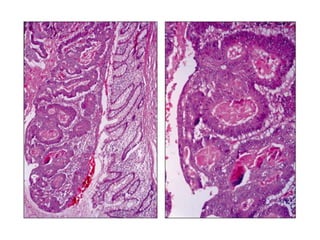
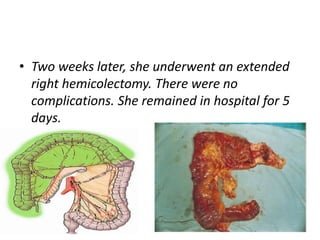
A 79-year-old woman presented with constipation, weight loss, and abdominal discomfort over the past year. Blood tests confirmed iron-deficiency anemia. CT colonography showed thickening in the ascending colon. Colonoscopy revealed a partial obstruction from a polypoid mass in the ascending colon. She underwent a right hemicolectomy, and pathology found a T3N0M0 moderately differentiated mucinous adenocarcinoma. She declined adjuvant chemotherapy due to risks. Surveillance colonoscopy is planned in one year.