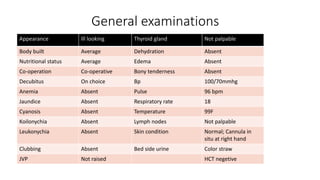
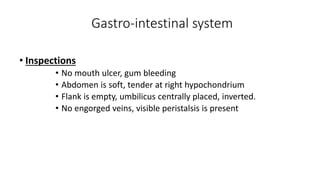
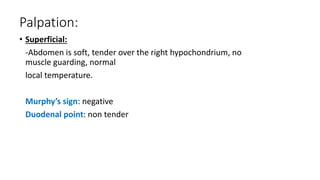
- Md. Dulal, a 42-year-old male shopkeeper, presented with 6 months of recurrent upper abdominal pain aggravated by fatty foods. Examination found right hypochondriac tenderness.
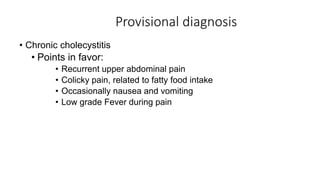
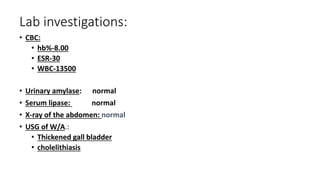
- Tests showed thickened gallbladder and cholelithiasis on ultrasound. Provisional diagnosis was chronic cholecystitis given recurrent pain related to fatty foods and tenderness in the right upper quadrant.
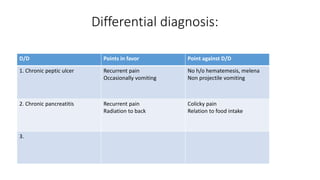
- Differential diagnoses considered were chronic peptic ulcer and pancreatitis but were less likely given absence of hematemesis, melena, or projectile vomiting. Management options discussed were open or laparoscopic cholecystectomy.