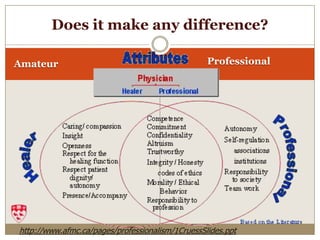
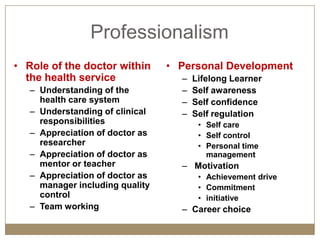
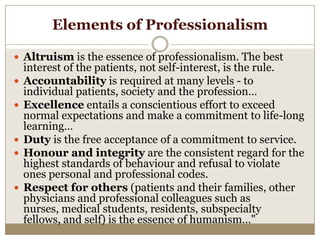
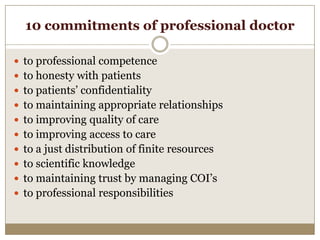
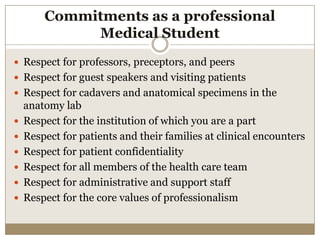
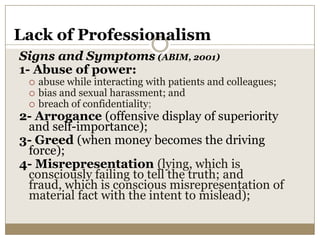
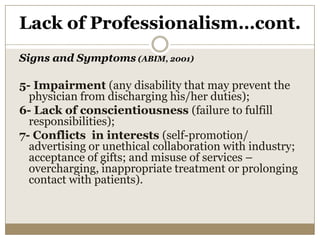
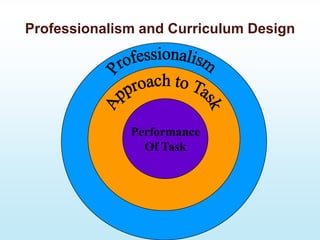
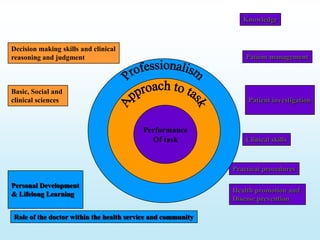
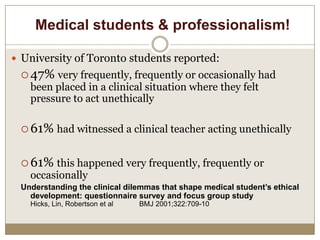
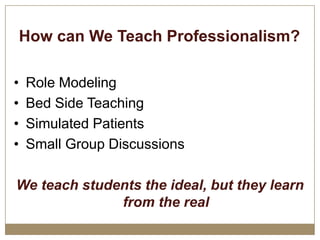
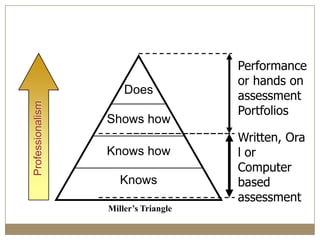
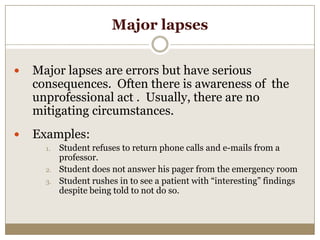
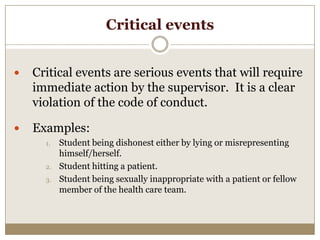
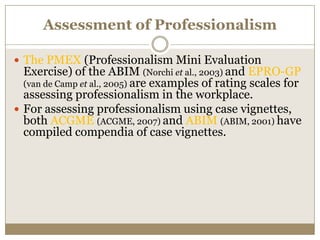
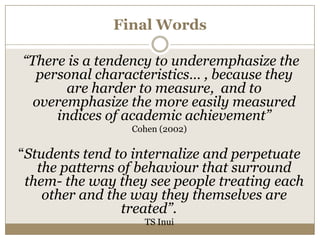
The document explores the concept of professionalism in medicine, emphasizing altruism, accountability, and integrity as fundamental elements. It discusses the importance of self-awareness, lifelong learning, and ethical behavior among medical professionals, along with the need for structured assessment methods to evaluate professionalism. The text also outlines the various commitments expected of medical professionals and the consequences of unprofessional behavior.