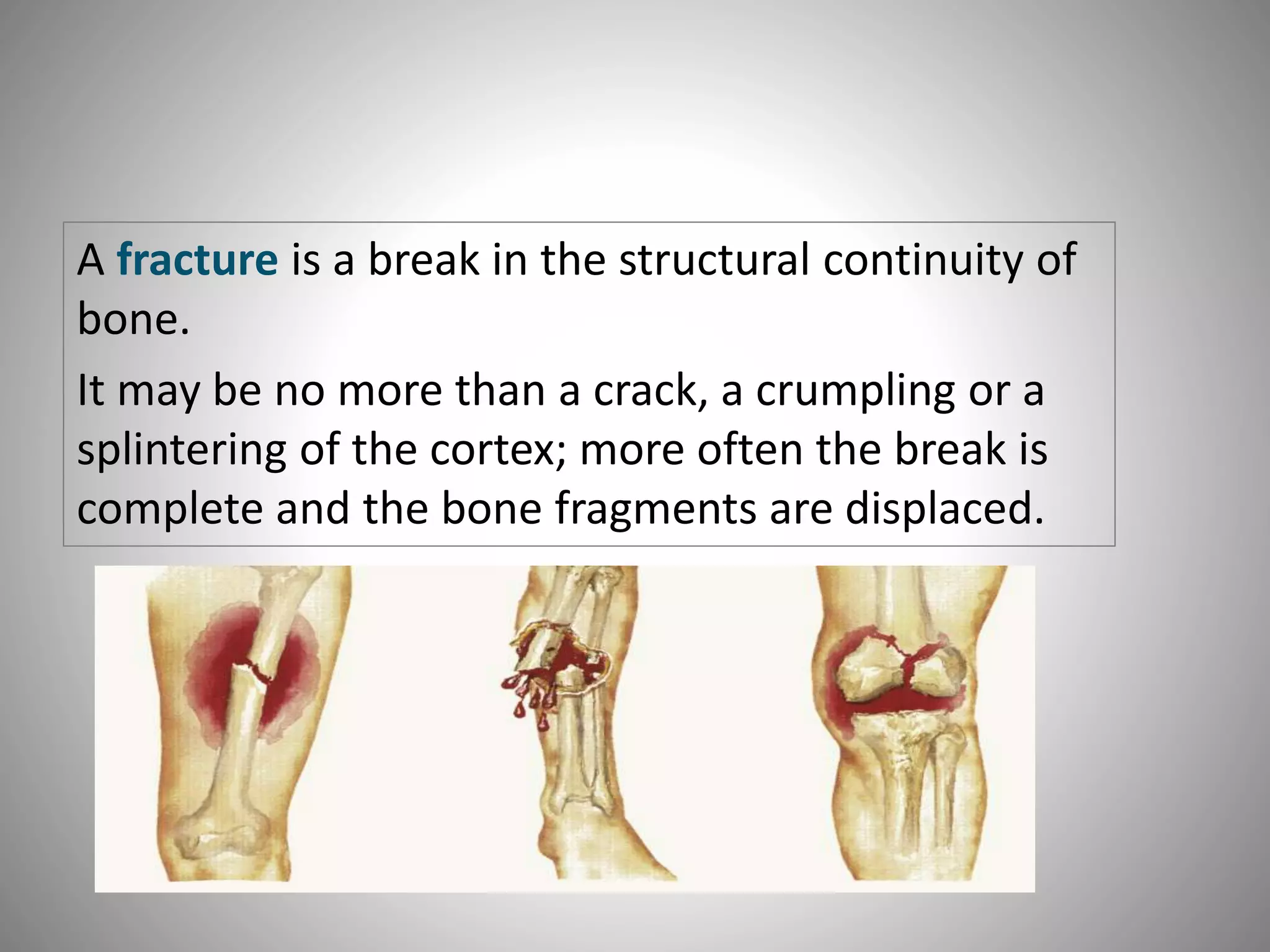
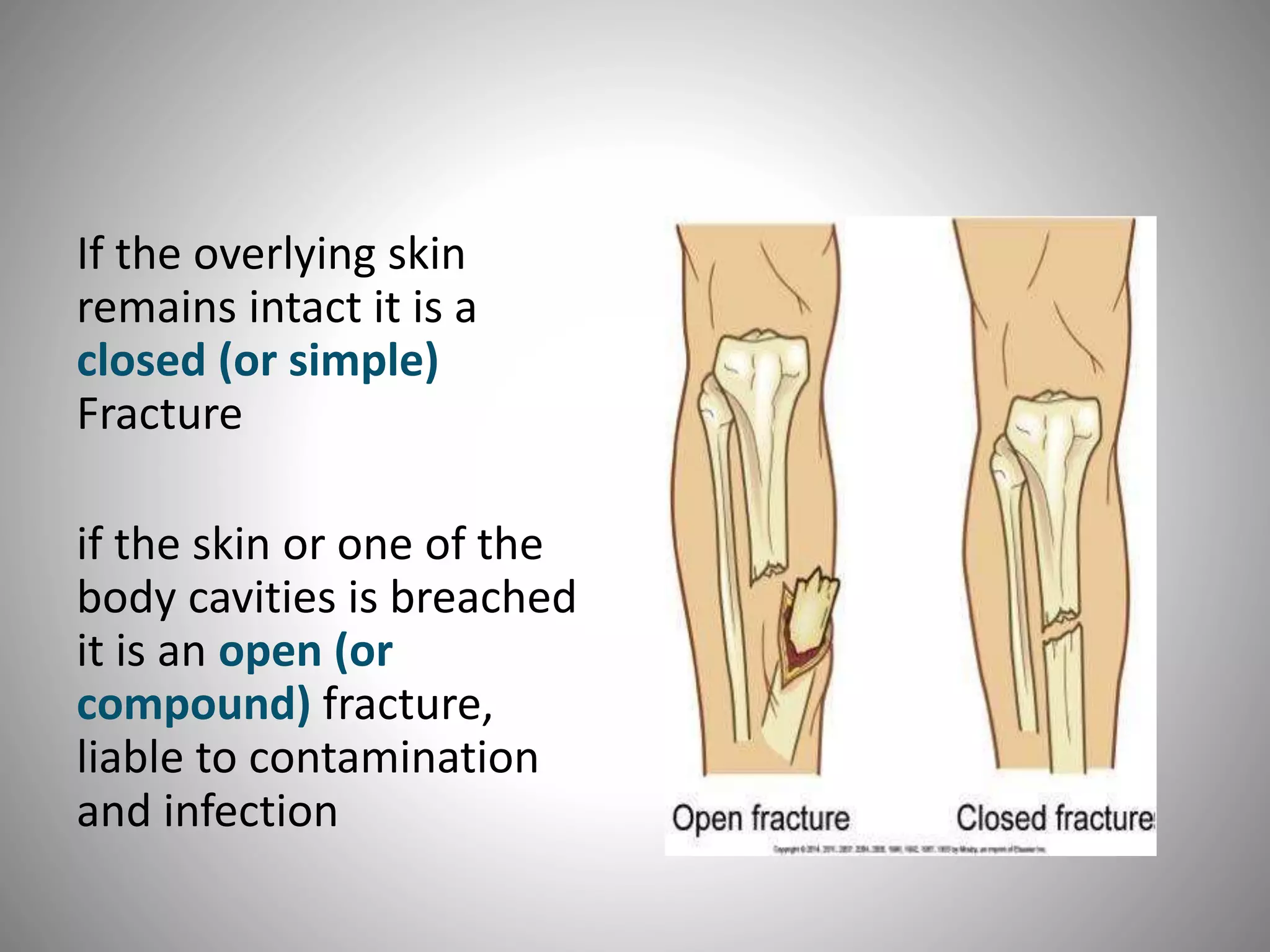
1) A fracture is a break in the bone that can range from a crack to a complete break with bone fragments displaced. Closed fractures involve an intact skin surface while open fractures breach the skin or a body cavity.
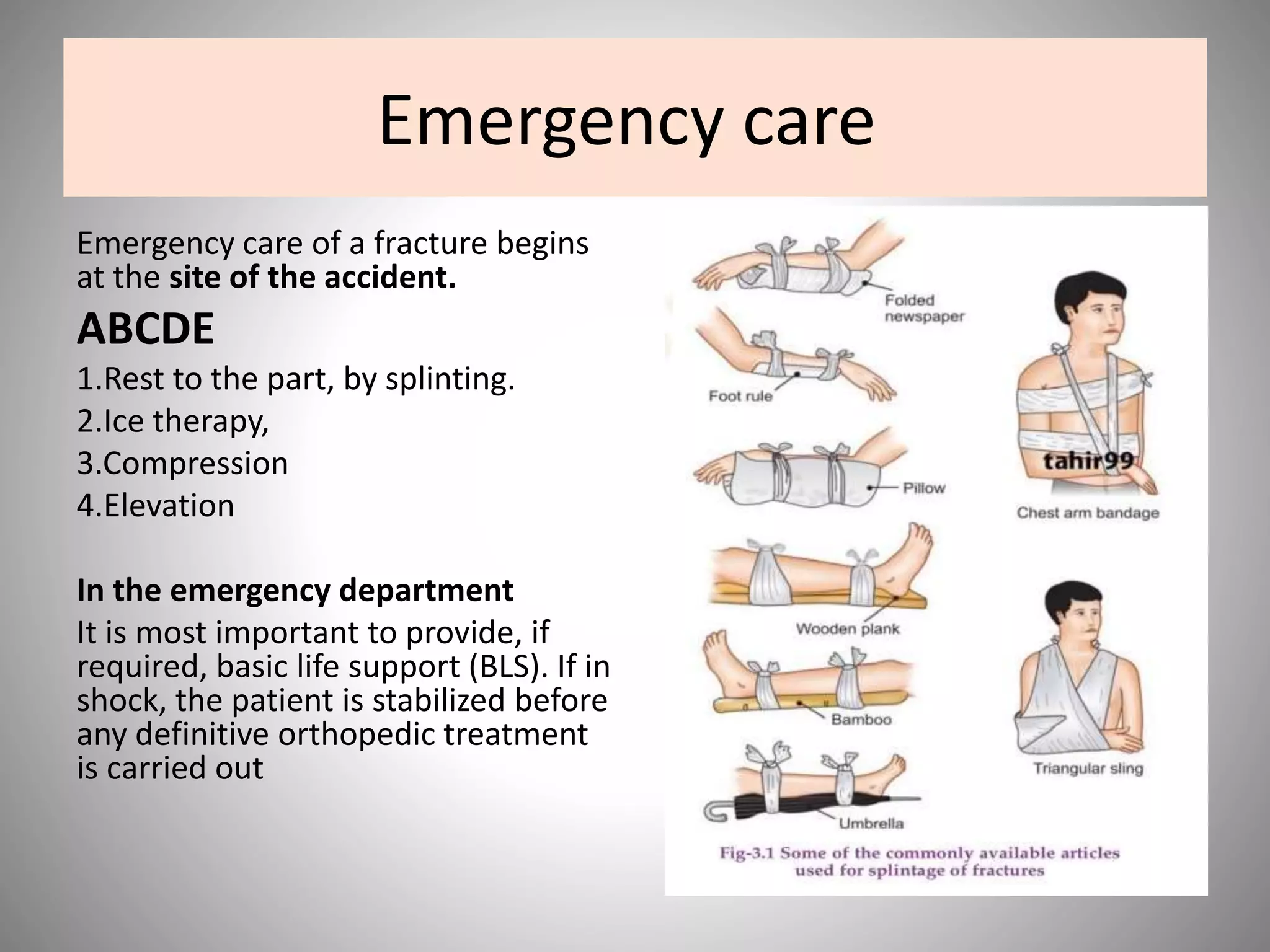
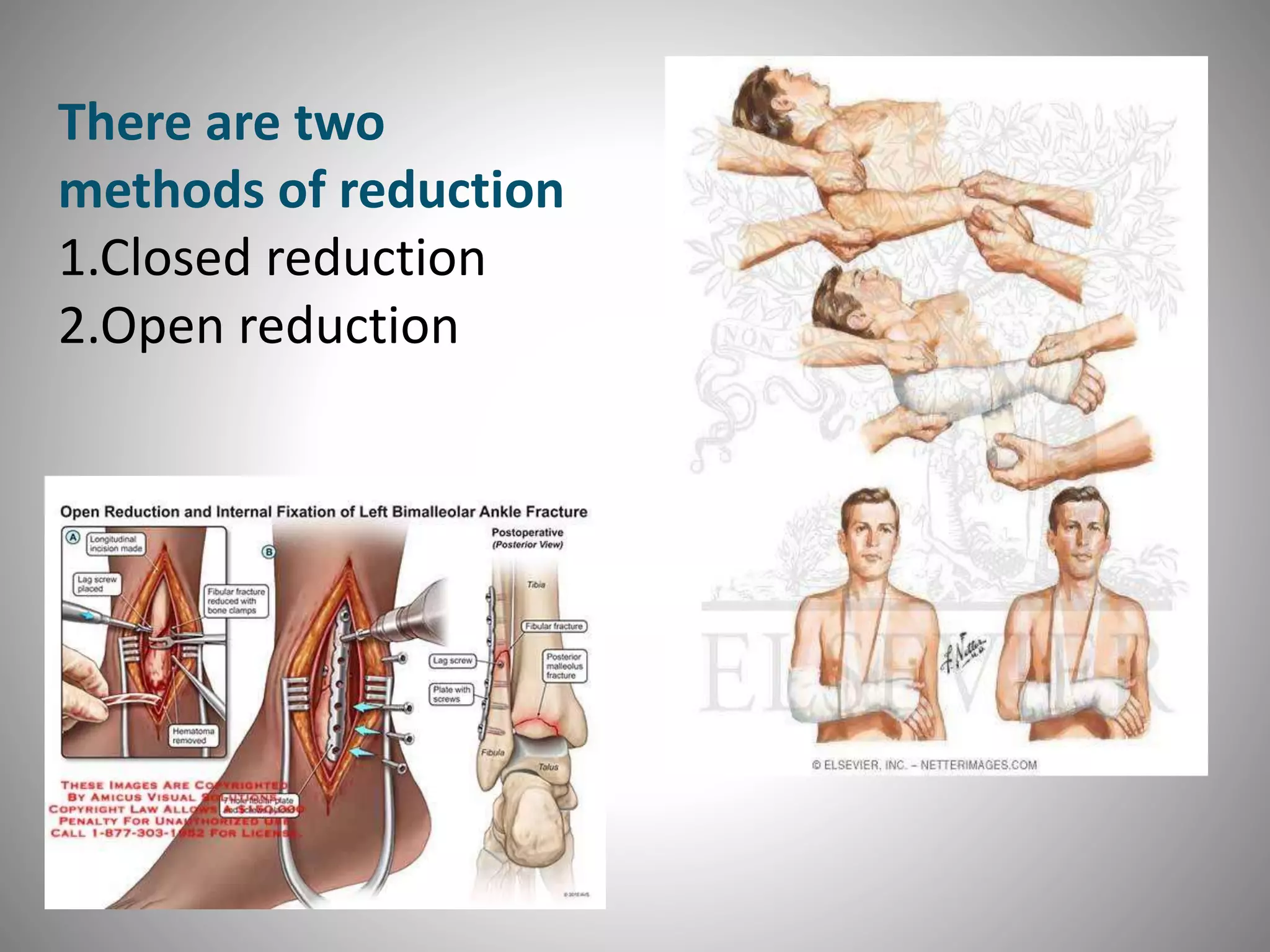
2) Treatment of fractures involves three phases - emergency care, definitive care, and rehabilitation. Emergency care focuses on splinting, RICE therapy, and stabilizing the patient. Definitive care includes reducing the fracture, using various methods to hold the reduction in place, and early mobilization.
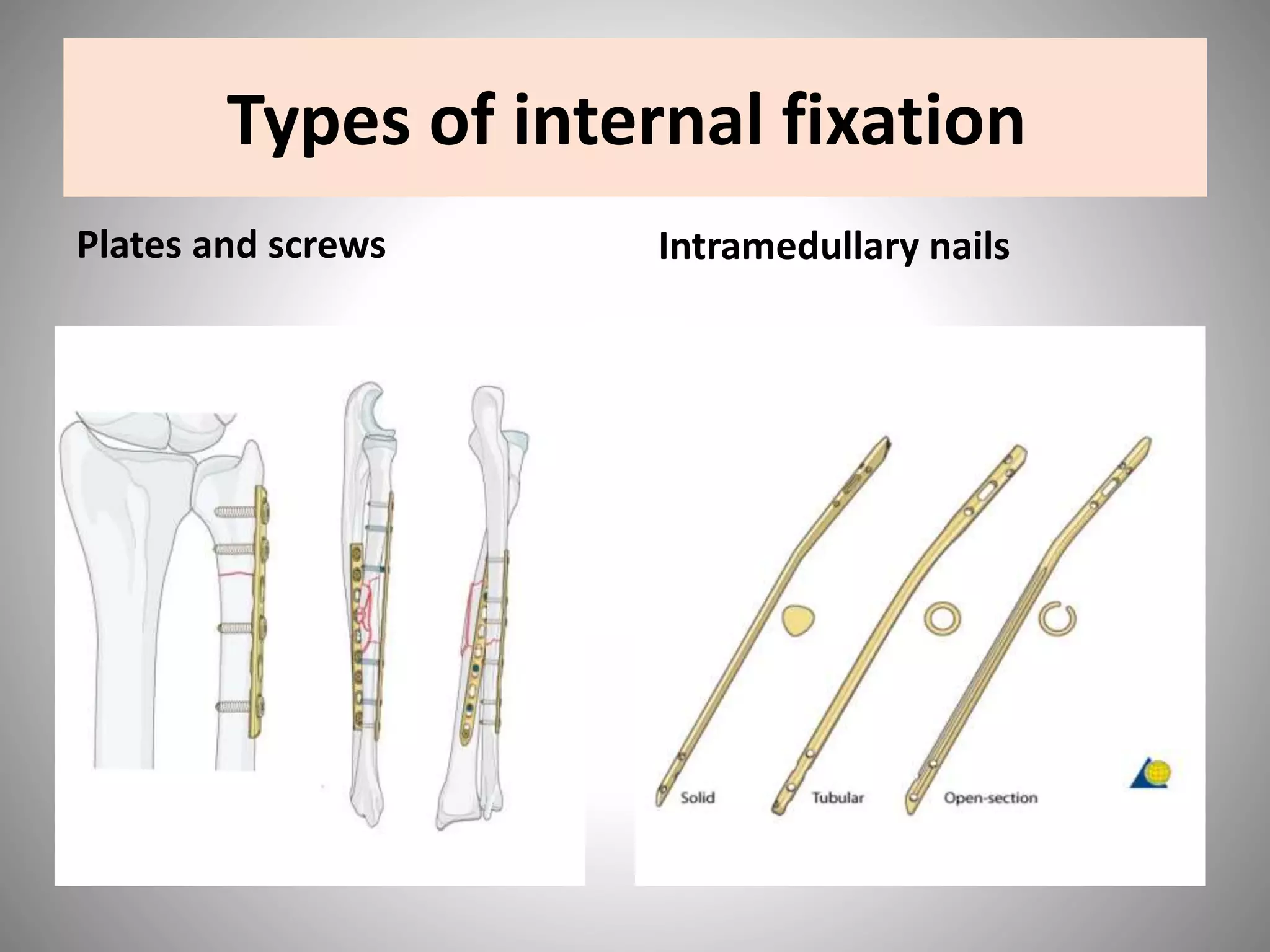
3) Management of closed fractures generally prioritizes the patient's general condition first before addressing the fracture. Methods to hold a closed fracture in place include casting, traction, internal fixation, external