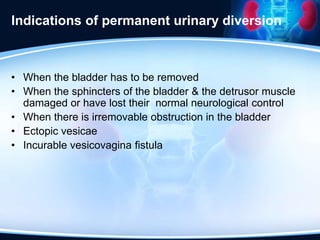
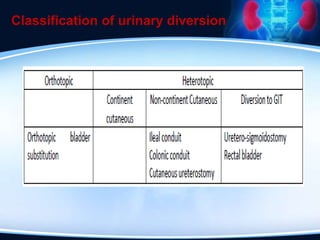
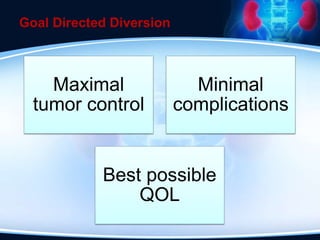
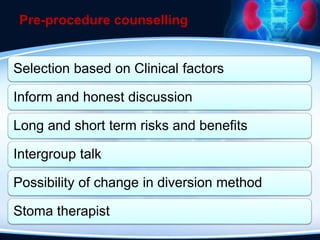
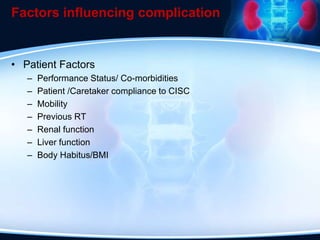
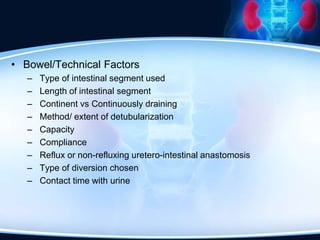
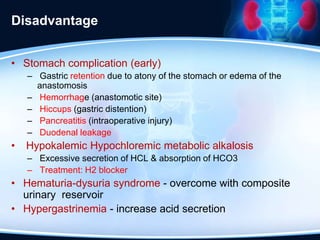
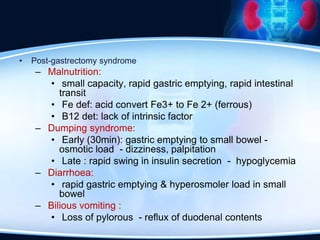
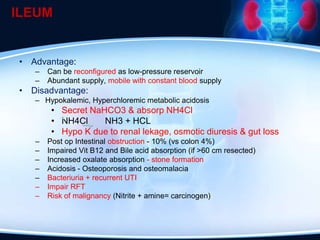
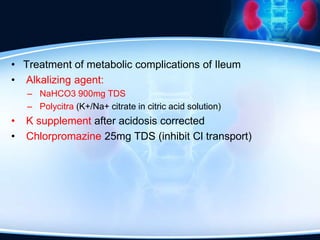
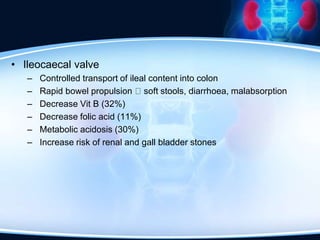
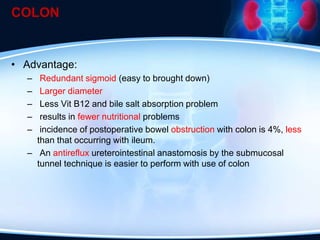
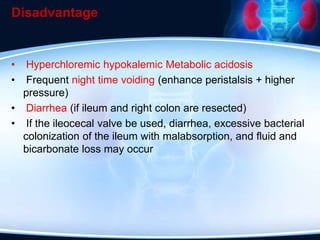
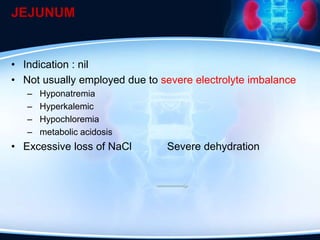
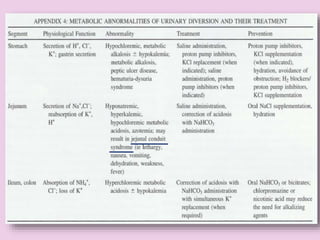
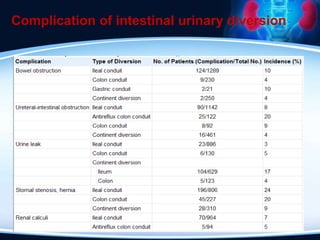
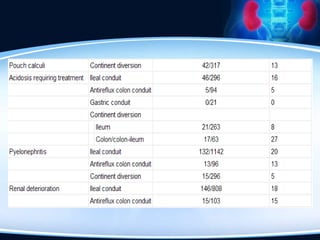
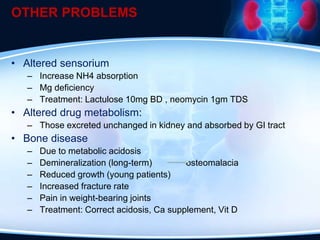
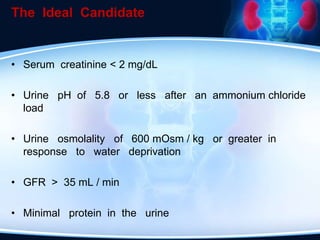
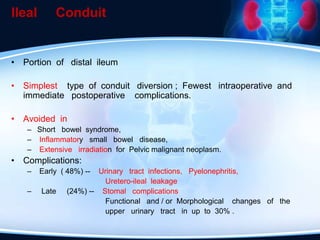
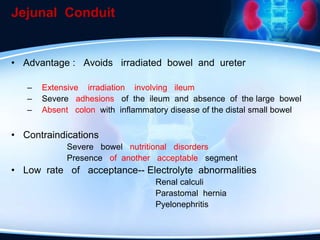
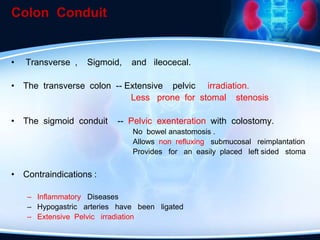
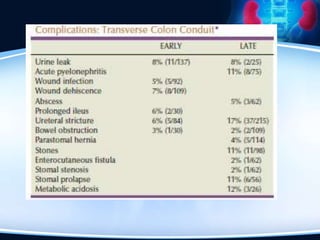
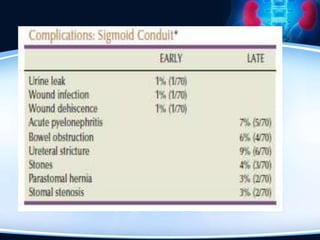
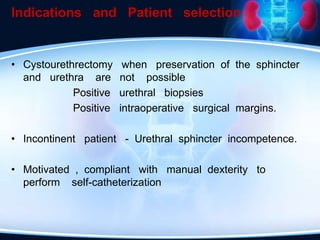
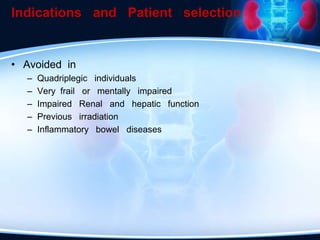
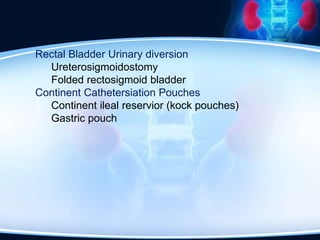
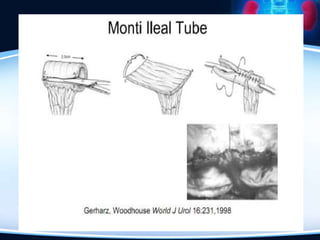
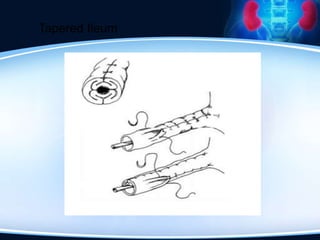
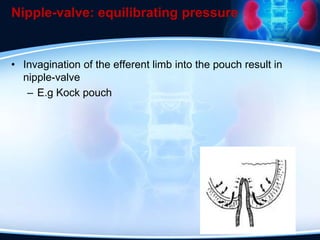
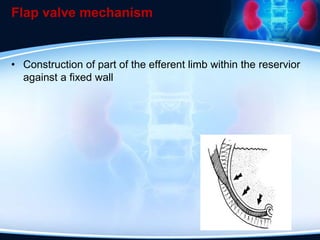
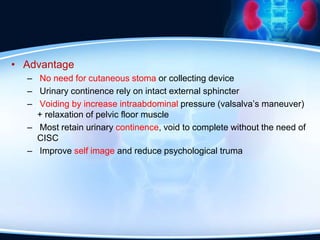
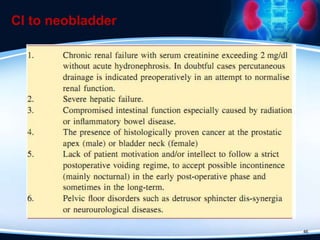
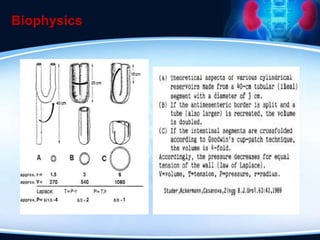
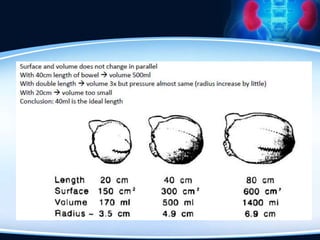
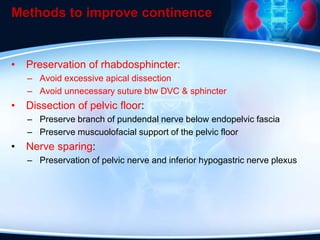
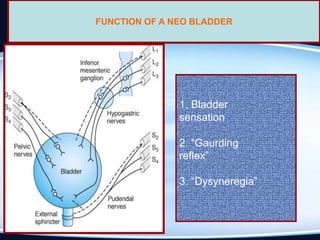
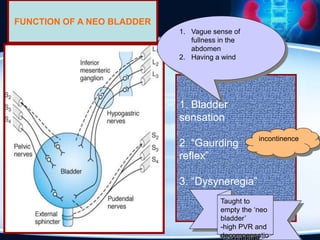
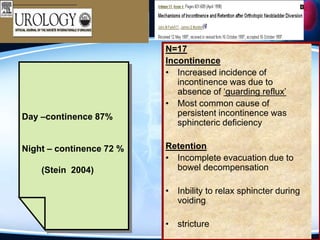
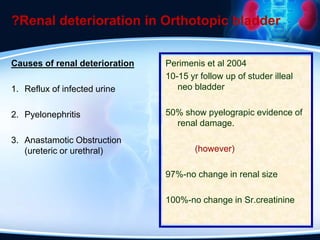
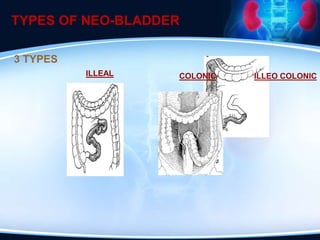
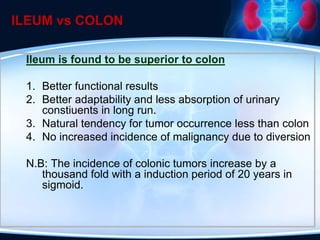
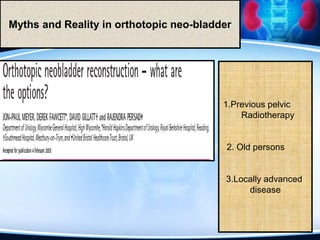
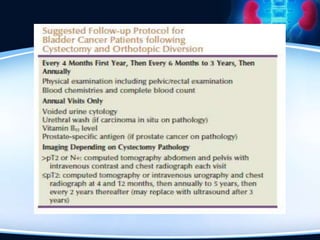
The document discusses indications, types, and complications associated with urinary diversion in urological surgery. It outlines various methods of urinary diversion, including ileal conduit, colon conduit, and orthotopic neobladder, along with their advantages and disadvantages, and emphasizes the importance of pre-procedure counselling. Factors influencing complications and patient selection criteria for specific diversion methods are also highlighted to optimize outcomes and quality of life.