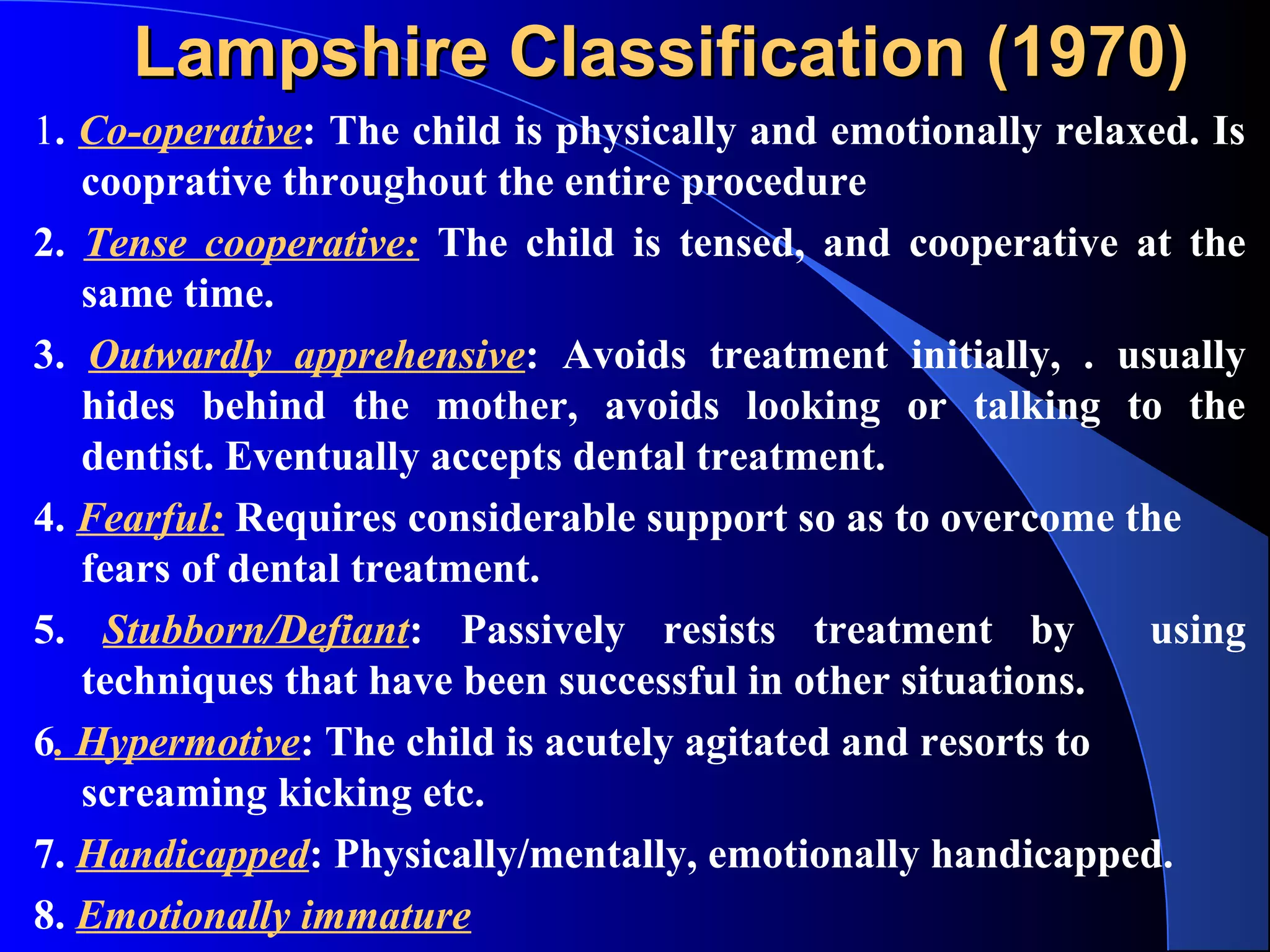
This document discusses child behavior and behavior management techniques in dentistry. It defines concepts like fear, anxiety, and emotions commonly seen in children. It also describes various classification systems used to assess child behavior and factors that can influence it like parental attitudes. The document outlines non-pharmacological behavior management techniques including communication, modeling, desensitization and contingency management. It discusses practical considerations for behavior management in a dental clinic.



















![Factors affecting ChildsFactors affecting Childs
behaviorbehavior
Under the control of dentist
Under the control of parents
– Maternal anxiety and attitudes [Overprotective,
Overindulgent, Under affectionate, Rejecting,
authoritarian]
Others [socioeconomic status, nutritional,past
dental experience]](https://image.slidesharecdn.com/child-behaviormanagement-140427150349-phpapp01/75/Child-behavior-management-TECHNIQUES-25-2048.jpg)



![CommunicationCommunication
Verbal [establishment of communication,
establishment of communicator ,message clarity,tone]
Nonverbal [Multi sensory Communication]
Problem Ownership –Use “I” messages,
Active Listening
Appropriate Responses to the situation](https://image.slidesharecdn.com/child-behaviormanagement-140427150349-phpapp01/75/Child-behavior-management-TECHNIQUES-29-2048.jpg)




![Tell-show-do[ Addelston]Tell-show-do[ Addelston]
The technique involves verbal explanations of
procedures in phrases appropriate to the
developmental level of the patient (tell);
demonstrations for the patient of the visual, auditory,
olfactory, and tactile aspects of the procedure in a
carefully defined, non threatening setting (show);
and then, without deviating from the explanation and
demonstration, completion of the procedure (do).
The tell-show-do technique is used with
communication skills (verbal and nonverbal) and
positive reinforcement.](https://image.slidesharecdn.com/child-behaviormanagement-140427150349-phpapp01/75/Child-behavior-management-TECHNIQUES-34-2048.jpg)




![ModelingModeling
Allowing the patient to
observe one or more
individuals [models]
Patient frequently
imitates the models](https://image.slidesharecdn.com/child-behaviormanagement-140427150349-phpapp01/75/Child-behavior-management-TECHNIQUES-39-2048.jpg)












































![ROUTES OF ADMINISTRATIONROUTES OF ADMINISTRATION
Inhalation
Enteral [ oral and rectal]
Parenteral [ IM, IV, IN, Submucosal, sub
cutaneous,]](https://image.slidesharecdn.com/child-behaviormanagement-140427150349-phpapp01/75/Child-behavior-management-TECHNIQUES-84-2048.jpg)

![Nitrous oxide and oxygenNitrous oxide and oxygen
sp gr 1.53,low solubility in blood, rapid onset , no
bio transformation,excreted by lungs
Adverse effects [ N2O Entraped in gas filled
spaces]](https://image.slidesharecdn.com/child-behaviormanagement-140427150349-phpapp01/75/Child-behavior-management-TECHNIQUES-86-2048.jpg)







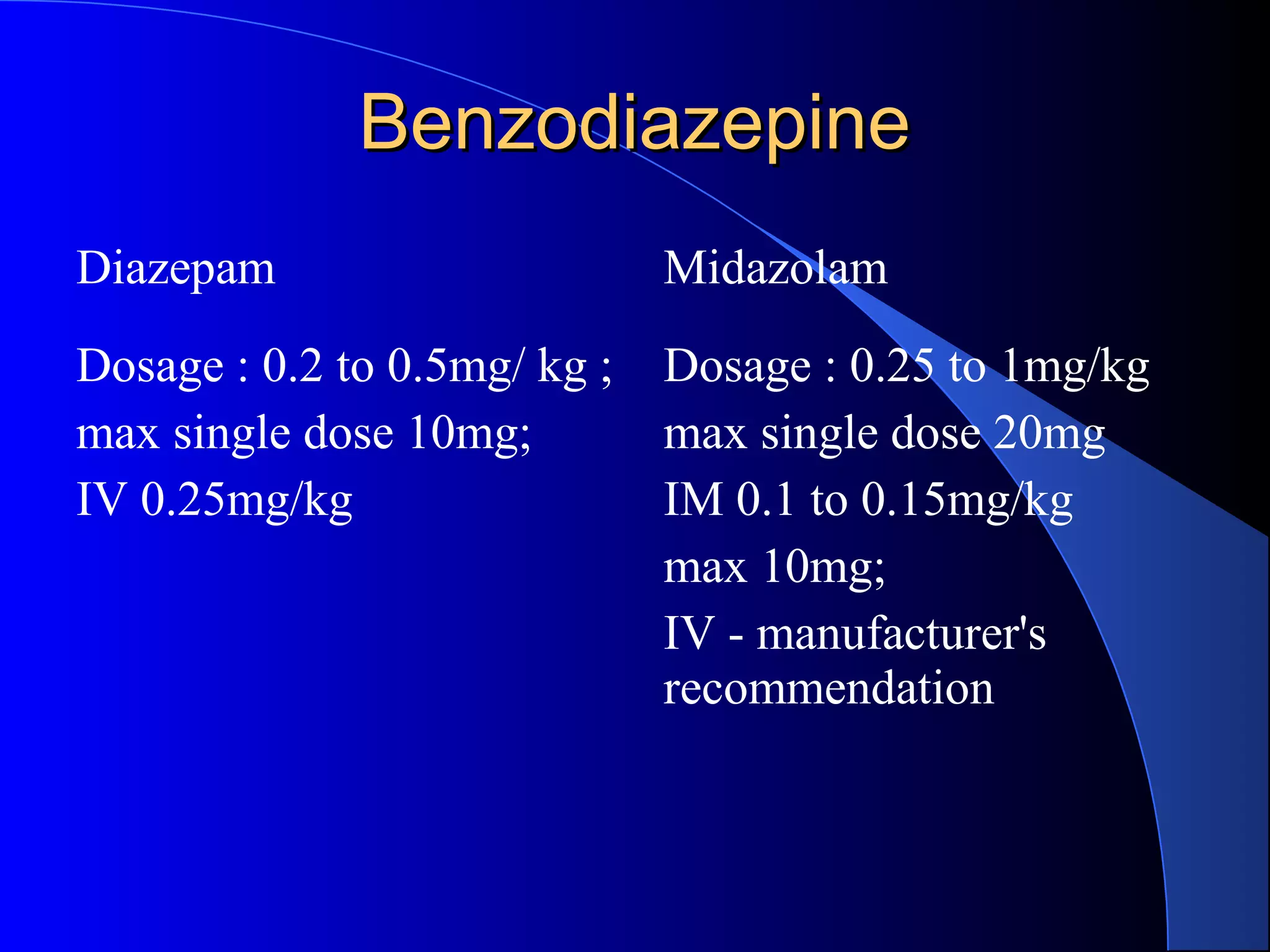
![Common agents used for sedationCommon agents used for sedation
Gases
Antihistamines
[Hydroxyzine ,Promethazine,Diphenhydramine]
Benzodiazepines
[Diazepam , Midazolam, lorazepam]
Benzodiazepines Antagonist [Flumazenil]
Sedative Hypnotics [Barbiturates ,Chloral Hydrate]
Narcotics [Meperidine ,Fentanyl]
Narcotic Antagonist [Naloxone]
Dissociative agent [Ketamine]
Others [Propofol]](https://image.slidesharecdn.com/child-behaviormanagement-140427150349-phpapp01/75/Child-behavior-management-TECHNIQUES-94-2048.jpg)




![Ketamine [ Dissociative agent]Ketamine [ Dissociative agent]
Derivative of the street drug phencyclidine.
This drug carries an increased risk of deep sedation
and should be used only by those with hospital
privileges in deep sedation.
Induces a functional dissociation between the
cortical & limbic systems to create a sensory
isolation and “trance-like” state.
A potent pain reliever as the drug prevents cortical
interpretation of noxious stimuli.](https://image.slidesharecdn.com/child-behaviormanagement-140427150349-phpapp01/75/Child-behavior-management-TECHNIQUES-100-2048.jpg)


