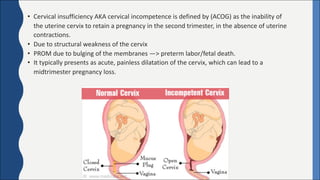
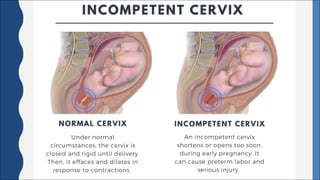
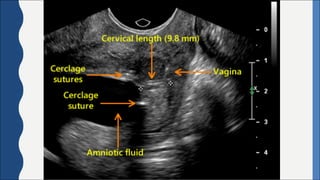
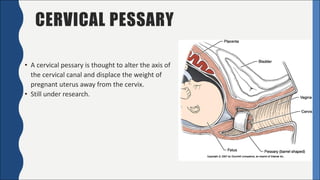
Cervical incompetence, also known as cervical insufficiency, is a condition characterized by the inability of the cervix to retain a pregnancy in the second trimester due to structural weakness. It can result in painless cervical dilation and premature rupture of membranes, leading to midtrimester pregnancy loss or preterm birth. Risk factors include previous cervical trauma from procedures or injuries, and exposure to diethylstilbestrol in utero. Diagnosis involves assessing cervical length by ultrasound and testing for fetal fibronectin. Treatment options include cervical cerclage surgery to reinforce the cervix, a cervical pessary, and progesterone supplementation to reduce recurrent preterm birth risk.