Calculus Disease
This document discusses calculus disease, including epidemiology, etiology, types of stones, clinical presentation, investigations, and treatment options. Some key points:
- Most patients are 30-60 years old and male. Stones are more common in Asians and whites.
- Risk factors include diet, climate, urine composition, infection, immobilization, and metabolic conditions.
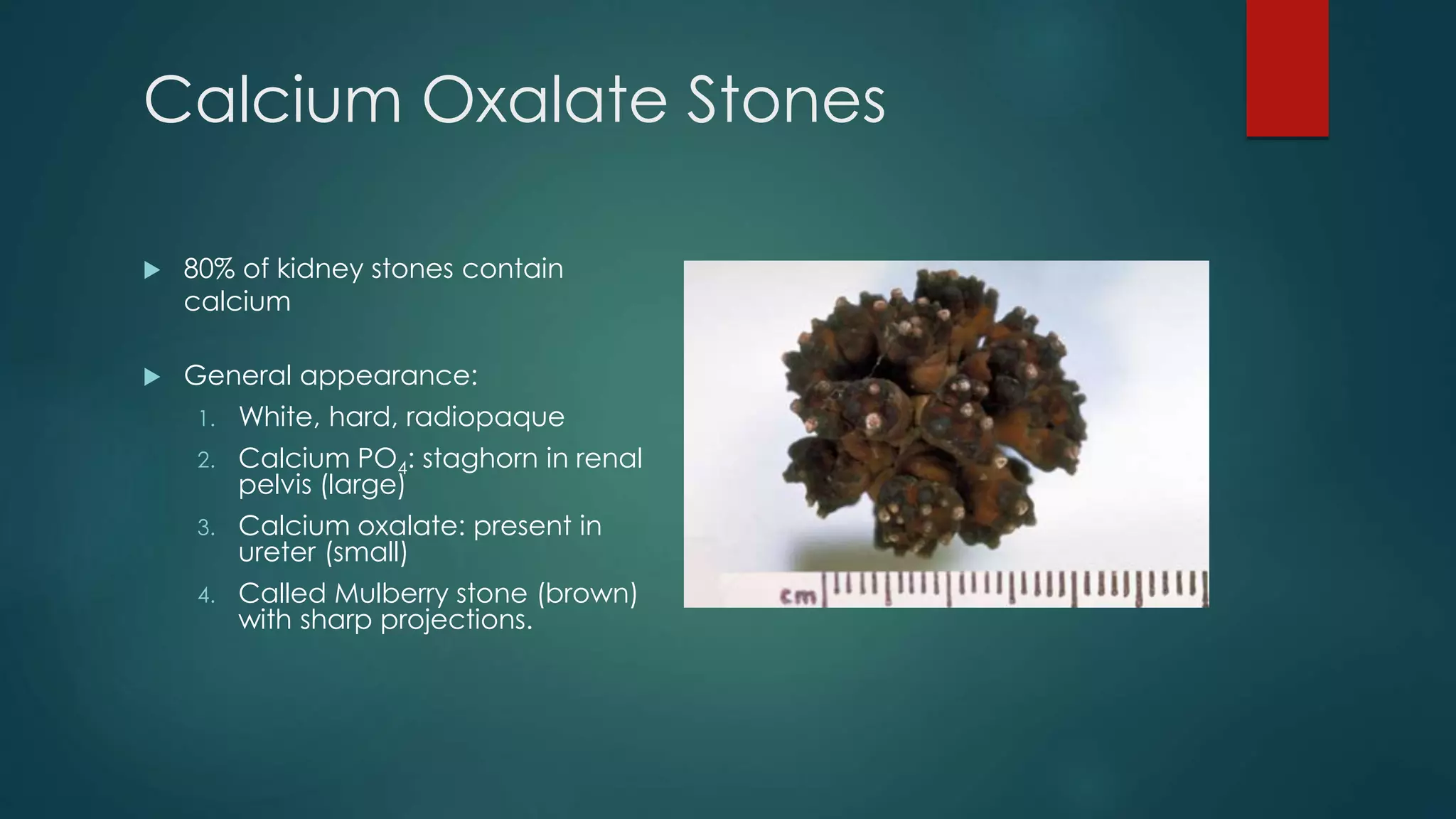
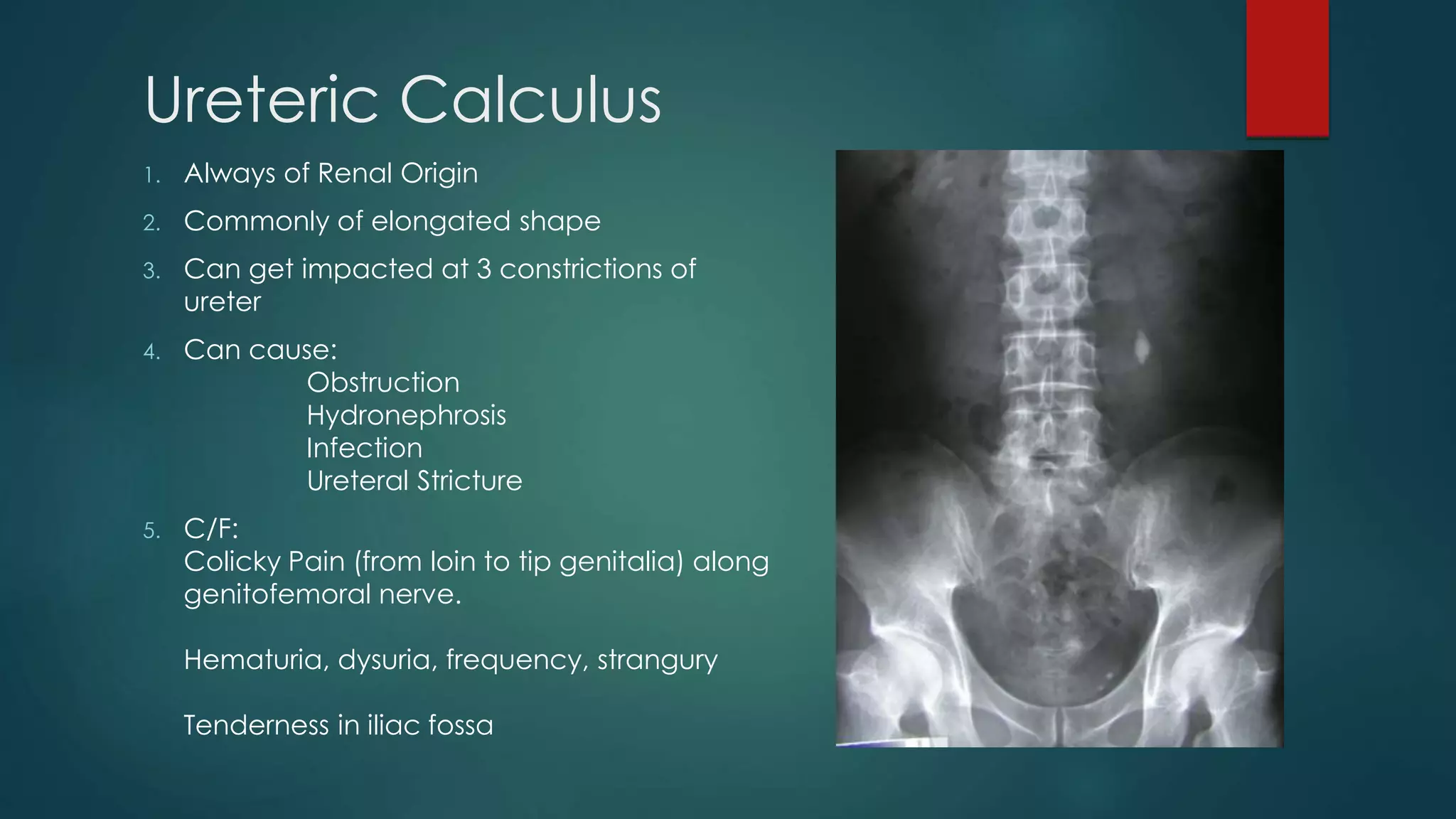
- Common stone types are calcium oxalate, phosphate, uric acid, cystine, xanthine, and struvite.
- Clinical presentation includes renal colic pain radiating from the flank to the groin, sometimes with hematuria. Investigations include blood tests, urine analysis, X-rays