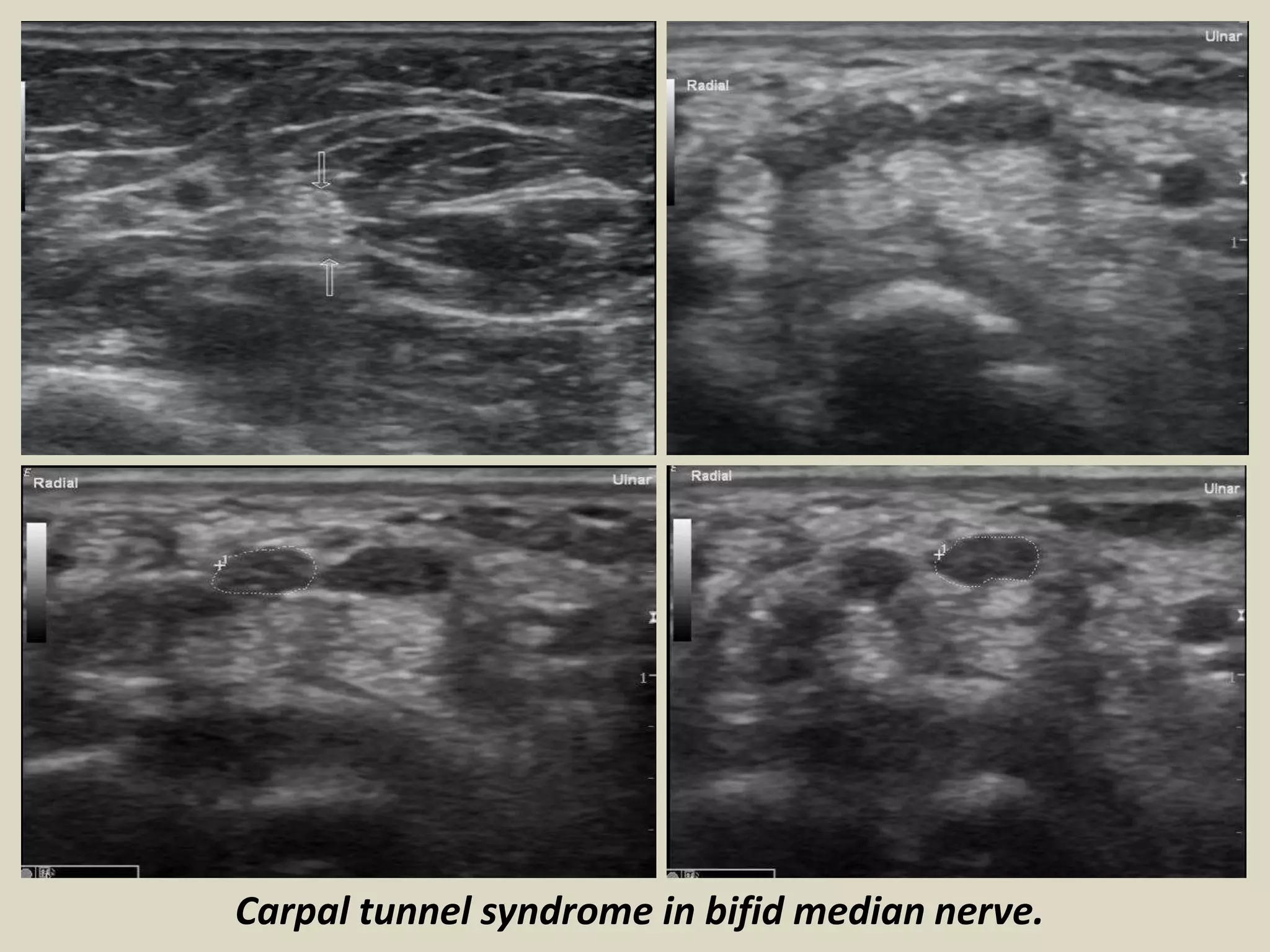
This document provides an ultrasound examination of the wrist joint, with descriptions of the anatomy and pathology that can be visualized. It examines the wrist in detail through 6 compartments on the dorsal side and structures on the volar side such as the carpal tunnel and Guyon's canal. Common conditions discussed include carpal tunnel syndrome, ganglion cysts, scapholunate ligament tears, tendon abnormalities, joint effusions, and other soft tissue lesions. The role of ultrasound in evaluating muscular, tendinous, ligamentous, vascular and other pathology of the wrist is outlined.