Parkinsonism syndromes with differential diagnosis
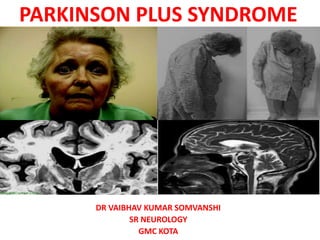
- 1. PARKINSON PLUS SYNDROME DR VAIBHAV KUMAR SOMVANSHI SR NEUROLOGY GMC KOTA
- 2. OUTLINE • Classification • Red flag signs • Diagnostic criteria • Phenotypic spectrum • Investigations • Novel biomarkers • Treatment • Future trends
- 3. INTRODUCTION • Common problem in neurology OPD • Wide variety of sporadic / heredodegenerative syndromes • 80-85% -IPD • Differentiation from other syndromes • Important in prognostication and management
- 5. PARKINSONISM PLUS • Progressive Supranuclear Palsy • Multiple System Atrophy [(Shy-Dragger syn.), SND (MSA P), OPCA (MSA C)] • Corticobasal Degeneration • Dementia with Lewy Body Disease
- 7. PROGRESSIVE SUPRANUCLEAR PALSY • Steele et al—1964 • 5% of parkinsonian pts • Male-to-female ratio is 1.5:1 • Commonly misdiagnosed as PD • Diagnosis is purely clinical • Always sporadic, few familial cases
- 8. • The usual interval from initial symptom occurrence to the need for a cane or a walker is 3.1 years, • Confinement to a chair or bed is 8.2 years. • Median disease duration of 9.7 years
- 9. • Postural Instability & EP Features : • Falls—backward • Rigidity –axial • Hypophonic • Widely based ataxic • Frontal release signs • Pseudobulbar palsy • L-DOPA UNRESPONSIVENESS
- 10. • Early signs- Slow vertical saccades and square wave jerks • Reduced blink rate and apraxia of eyelid opening • On doll’s eye maneuver, there is improved range • Subcortical-type dementia • Typical facies- “surprised look” • Advanced PSP - Complete ophthalmoparesis
- 12. NINDS PSP DIAGNOSTIC CRITERIA • Possible PSP(highly sensitive) • Mandatory inclusion criteria: • Gradually progressive disorder • Onset age 40 or later • Either vertical supranuclear palsy or both slowing of vertical saccades • Postural instability with falls within a year of disease onset • No evidence of other diseases that could explain the foregoing features, as Indicated by exclusion criteria
- 13. • Mandatory exclusion criteria: • Recent history of encephalitis • Alien limb syndrome • Cortical sensory deficits • Focal frontal or temporoparietal atrophy • Hallucinations or delusions unrelated to dopaminergic therapy • Cortical dementia of Alzheimer type • Prominent, early cerebellar symptoms • Unexplained dysautonomia
- 14. • Supportive features: • Symmetrical akinesia or rigidity • Proximal more than distal • Abnormal neck posture especially retrocollis • Poor or absent response of parkinsonism to levodopa • Early dysphagia and dysarthria • Early onset of cognitive impairment including two or more of: apathy, Impairment in abstract thought, decreased verbal fluency, utilisation or Imitation behaviour , or frontal release signs
- 15. • Probable PSP(highly specific) • Mandatory inclusion criteria • Gradually progressive disorder • Onset age 40 or later • Vertical supranuclear palsy • Prominent postural instability with falls within a year of disease onset • No evidence of other diseases that could explain the foregoing features, • As indicated by exclusion criteria
- 16. • Definite PSP • Mandatory inclusion criteria: • Clinically probable or possible PSP and • Histopathological evidence of typical PSP
- 18. INVESTIGATIONS • Clinical diagnosis • MRI midbrain atrophy (appearance of a flat or concave profile -68% sensitivity and an 89% Specificity • Superior cerebellar peduncle atrophy. • “Morning Glory Flower Sign” and the “Hummingbird Sign” – Highly specific(100%) low Sensitivity (50% and 68.4%) • Magnetic resonance parkinsonism index (MRPI) - sensitivity of 100% and specificity of 99·2–100·0% for PSP-RS. • Pons : Midbrain ratio
- 19. MAGNETIC RESONANCE PARKINSONISM INDEX (MRPI) P = area of pons in midsagittal plane MCP = width of middle cerebellar peduncle (P / M) x (MCP / SCP) M = area of midbrain in midsagittal plane SCP = width of superior cerebellar peduncle value more than 13.55 abnormal , strongly suggests will develop PSP.
- 20. • PET – lowered glucose metabolism in the midbrain ,caudate, thalamus of PSP • MIBG is abnormal in PD because of postganglionic sympathetic denervation, but is typically normal in PSP . • IBZM SPECT assessing the postsynaptic receptors is abnormal in PSP and normal in PD • IBZM SPECT is abnormal in all APS • DAT scan is abnormal in PD and all AP syndromes
- 23. PATHOLOGY • Spares the cortex and involves the basal ganglia,dentate, pontine, and oculomotor nuclei. • Abnormal tau hyperphosphorylation and deposition. Tau is encoded by MAPT and normally functions to stabilize microtubules. • Neurofibrillary tangles are present in reticular formation and ocular motor nuclei. • Tufted astrocytes -feature of PSP that differentiates other tauopathies such as CBD (astrocytic plaques,colloid bodies)
- 25. NOVEL DIAGNOSTIC APPROACH AND BIOMARKERS • CSF tau protein- CSF phospho-tau and total tau concentrations lower than AD • 2–5 times increased neurofilament light chain concentrations in PSP
- 26. TREATMENT • No effective symptomatic or neuroprotective treatments • A trial of levodopa (up to 1 g/d) and amantadine (up to 450 mg/d) • Botulinum toxin injections can be used to treat levator inhibition,rigidity , dystonia • Serotonin reuptake inhibitors (SSRIs) may be used for apathy with no clear benefit. • Supportive measures such as physiotherapy, walking aids, speech therapy and PEG
- 27. • A small study with Coenzyme Q10- no RCT study • Recent large, double-blind studies with (glycogen synthase kinase)GSK-3b inhibitors (Tideglusib,Davunetide) ,prevent hyperphosphorylation of tau- failed. • Tideglusib reduced the rate of brain atrophy in one study.
- 28. MULTIPLE SYSTEM ATROPHY • Sporadic neurodegenerative disorder clinically any combination of parkinsonian, autonomic, cerebellar, or pyramidal signs. • MSA is an alpha-synucleinopathy. • Usually a sporadic disease; however, rarely, familial cases - mutations in COQ2 gene. • Prevalence of MSA - ranged from 1·9 to 4·9 cases per 100 000 people
- 29. CLINICAL PRESENTATION : • Affects both men and women • Sixth decade of life • Mean survival of 6–9 years.(Upto 15yrs) Main features • Autonomic failure • Parkinsonism • Cerebellar ataxia • Pyramidal signs in any combination
- 30. TWO MAJOR MOTOR MANIFESTATIONS Distinguished clinically– • 1. Parkinsonian features predominate in 80% of patients (MSA-P subtype), • 2. Cerebellar ataxia is the main motor feature in 20% of patients (MSA-C subtype). • Both similar survival times. • MSA-P - more rapid functional deterioration
- 31. MSA-P • Progressive akinesia and rigidity • Jerky postural tremor and tremor at rest. • Orofacial or craniocervical dystonia • Recurrent falls at disease onset are unusual . • 90% of the MSA-P pts- unresponsive to levodopa in the long term.
- 32. MSA-C • Gait ataxia • Scanning dysarthria • Cerebellar oculomotor disturbances. • May be indistinguishable from other patients with idiopathic late onset cerebellar Ataxia
- 33. • Dysautonomia • Urogenital and orthostatic dysfunction. • Early erectile dysfunction is nearly universal in men with MSA • Female- genital insensitivity • Urinary incontinence or retention are common
- 34. CONSENSUS STATEMENT FOR CLINICAL DIAGNOSIS OF MSA • Autonomic and urinary dysfunction • Features • 1. Orthostatic hypotension(68% of patients) • 2. Urinary incontinence or incomplete bladder emptying • Criteria • Reduction of least 30mmhg or in diastolic blood pressure by at least 15 mm hg after 3 min of standing • Urinary incontinence (persistent, involuntary partial or total bladder emptying, • Accompanied by erectile dysfunction in men or both
- 35. • Parkinsonism : initial feature in 46% of patients with MSA-P • A. Features • 1. Bradykinesia • 2. Rigidity • 3. Postural instability (not caused by primary visual, vestibular, cerebellar, or proprioceptive dysfunction) • 4. Tremor (postural, resting or both) • B. Criteria • Bradykinesia plus at least one of features 2–4
- 36. • Cerebellar dysfunction :initial feature in 5% • A. Features • 1. Gait ataxia • 2. Ataxic dysarthria • 3. Limb ataxia • 4. Sustained gaze-evoked nystagmus • Criteria • Gait ataxia plus at least one of features 2–4
- 37. • Corticospinal tract dysfunction • A. Features • 1. Extensor plantar responses with hyper-reflexia • Criteria • No corticospinal tract features are used in defining the diagnosis of MSA • Prominent and severe spasticity should raise suspicion for an alternative diagnosis
- 38. • Exclusion criteria: • Symptomatic onset <30 years/>75YRS of age • Family history of a similar disorder • Systemic disease or other identifiable causes • Hallucinations unrelated to medication • Dementia
- 39. • Exclusion criteria: • Prominent slowing of vertical saccades or vertical supranuclear gaze palsy • Evidence of focal cortical dysfunction • Laboratory investigation- metabolic, molecular genetic and imaging evidence of an alternative cause of features
- 40. • Possible MSA • A sporadic, progressive, adult (>30y) with onset disease characterized by the following: • Parkinsonism or cerebellar syndrome • At least 1 feature of autonomic or urogenital dysfunction • At least 1 additional feature
- 41. • Probable MSA • A sporadic, progressive, adult (>30y) with onset disease characterized by the following: • Autonomic failure involving urinary dysfunction • Poorly levodopa-responsive parkinsonism or cerebellar dysfunction
- 42. Definitive MSA • A sporadic, progressive, adult (>30y) with onset disease pathologically confirmed by Presence of high density GCIS in association with degenerative changes in Striatonigral and olivopontocerebellar pathways
- 43. MSA ADDITIONAL FEATURES • Pyramidal signs • Orofacial dystonia or dyskinesias • Dyskinesia mainly affecting orofacial muscles • Axial dystonia -PISA syndrome (subacute axial dystonia with a severe tonic lateral flexion of the trunk, head, and neck) early severe camptocormia
- 44. • Jerky tremor • Dysarthria- Atypical, irregular and severely hypophonic • Dysphagia within 5 years of motor onset • Neuropsychiatric features – Depression (41%) , Hallucinations (5·5%),Dementia (4·5%) , Insomnia (19%) ,Daytime sleepiness (17%) , Restless legs (10%)
- 46. Investigations • Autonomic function tests (table tilt,24 hr ambulatory bp,heart rate monitoring,baroreflex sensitivity,qsart,gastric emptying study,psg) • Cardiovascular function • Standard urine analysis will exclude infection. • The residual volume –USG,Cystometry ,UDS
- 47. IMAGING • MRI • Hot cross burn sign- mcp/pons- MSA-c • Putaminal rim- MSA-p • The slight hyperintensity of the lateral margin of the putamen on T2-weighted MRI is a characteristic finding in patients with MSA involving the extrapyramidal system • MSA-C-cerebellum and middle cerebellar peduncle
- 49. INVESTIGATIONS • DAT scan abnormal in all MSA, PSP, and PD • MIBG scintigraphy abnormal in PD, normal in MSA • IBZM SPECT is normal in PD,abnormal in MSA (but also in PSP and CBD • PET- The caudate putamen index- lower in patients with MSA than in PD
- 50. TREATMENT • Symptomatic • PD- l-dopa/ dopa agonists- cranio cervical dystonia postural hypotension • Amantidine- gait disturbances • Orthostatic hypotension- high salt, fludrocortisone, midodrine,droxidopa,pyridostigmine • Urinary dysfunction- oxybutinin • Erectile dysfunction– sildenafil, Intracavernosal inj. Or penile implants
- 51. Depression • SSRI/TCA Promising studies • Rasagiline • Intrarterial/IV - autologous stem cells Future trials • Alpha synuclein targeting antibodies
- 52. CORTICOBASAL DEGENERATION • Sixth to eighth decades of life - mean age 63 years • Sporadic disease , 4–6% of parkinsonism.
- 53. • Clinical presentations • The most common presentation (55%) -“useless arm” (ie, a rigid, dystonic, akinetic, or apraxic arm), • Gait disorder (27%) • Prominent sensory symptoms • Isolated speech disturbance • Behavioural disturbance
- 54. CLINICAL FEATURES • Motor (asymmetric) • Limb clumsiness • Bradykinesia/ Akinesia • Rigidity • Tremor (action/postural) • Myoclonus • Limb dystonia • Blepharospasm • Choreoathetoid movements • Speech abnormalities • Gait disorder
- 55. • Higher cortical functions • Apraxia • Dementia • Alien-limb phenomenon • Aphasia • Frontal-lobe-release signs • Cortical sensory abnormalities • Depression • Apathy • Anxiety irritability • Disinhibition, delusions,obsessive compulsive disorde
- 56. DIAGNOSTIC CRITERIA • Inclusion criteria (one of A or B) • A) Rigidity (easily detectable without reinforcement) and one cortical sign: Apraxia, Cortical sensory loss, Alien-limb phenomenon • B) Asymmetric rigidity, dystonia (focal in limb; present at rest at onset),Focal reflex myoclonus (spreads beyond stimulated digits)
- 57. • Exclusion criteria • Early dementia (will exclude some patients) • Early vertical gaze palsy • Rest tremor • Severe autonomic disturbances • Sustained responsiveness to levodopa • Lesions on imaging studies indicate another pathological process
- 59. • Imaging • MRI • Asymmetric frontal, and parietal cortical atrophy becomes evident with dilatation of the lateral ventricle (temporal/parietal cortex (the later pattern is seen in dementia of the alzheimer type)
- 60. • Dopamine transporter SPECT- abnormal,differentiate them from those with alzheimer’s and pick’s diseases (in whom this scan is typically normal) early in the course of the disease. FDG-PET • Asymmetric reduction in fronto parietal regions
- 61. • The R2 component of the blink reflex recovery cycle (R2 BRRC) appears to be a useful tool to distinguish progressive supranuclear palsy (PSP) from corticobasal degeneration (CBD) • 4-repeat-tau aggregates - neocortex in CBD, brainstem in PSP Eur J Neurol.sciacca g et al, 2018 Aug;25(8):1100-e85. doi: 10.1111/ene.13673. Epub 2018 Jun 12.
- 62. TREATMENT • L-dopa trial (upto 1 gm/d) • Amantadine(450 mg/d) • Valproate, levetiracetam- myoclonus • Botox inj- dystonic hand • Antioxidants or vitamin E if the patient has memory loss • Palliative rx
- 63. DEMENTIA WITH LEWY BODY • Dementia -not occur in the early stages ,usually evident with progression. • Deficits on tests of attention, executive function, and visuospatial ability may be especially prominent.
- 64. CORE FEATURES • Two core features are sufficient for a diagnosis of probable, one for possible DLB • Fluctuating cognition with pronounced variations in attention and alertness • Recurrent visual hallucinations that are typically well formed and detailed features of parkinsonism
- 65. SUGGESTIVE FEATURES • REM sleep behavior disorder • Severe neuroleptic sensitivity • Low dopamine transporter uptake in basal ganglia demonstrated by SPECT or PET imaging • One or more of these + one or more core features (probable DLB ) • In the absence of any core features, one or more suggestive features - possible DLB. • Probable DLB should not be diagnosed on the basis of suggestive features alone
- 66. SUPPORTIVE FEATURES • Repeated falls and syncope, Transient unexplained loss of consciousness • Severe autonomic dysfunction • Hallucinations in other modalities • Depression • Relative preservation of medial temporal lobe structures on CT/MRI scan • Generalized low uptake on SPECT/PET perfusion scan with reduced occipital activity • Prominent slow wave activity on EEG with temporal lobe transient sharp waves
- 67. TEMPORAL SEQUENCE OF SYMPTOMS • Diagnosed when dementia occurs before or concurrently with parkinsonism (if it is present). • Parkinson disease dementia (PDD) - dementia that occurs in the context of well established parkinson disease. • The 1-year rule between the onset of dementia and parkinsonism – DLB .
- 68. INVESTIGATIONS • MRI BRAIN -diffuse cerebral atrophy with relative preservation of occipital and mesial temporal lobes compared to alzheimer disease. • SPECT & PET -decreased occipital lobe blood flow – DLB > AD -relative preservation of the posterior cingulate gyrus (cingulate island sign) - DLB > AD
- 69. • SPECT scanning studies in DLB patients : • Visual hallucinations - Were related to hypoperfusion of the parietal and occipital association cortices • Misidentifications - Were related to hypoperfusion of the limbic-paralimbic structures • Delusions - Were related to hyperperfusion of the frontal cortices
- 70. • CSF • Tau – DLB < AD • Beta amyloid are lower than normal in DLB, AD • LBCRS - lewy body composite risk score - help determine whether lewy body pathology is contributing to dementia.
- 72. CLINICAL MANAGEMENT • Motor parkinsonism-mild hallucinations and agitation may not require medical treatment. • Levodopa at low doses & titrate up. • Anticholinergics should be avoided,worsen cognition,psychosis • Neuropsychiatric symptoms.--Cholinesterase inhibitors atypical antipsychotic • Memantine improves cognitive function and neuropsychiatric features in patients with DLB. • Recently Pimavenserin selective 5 HT2 inverse agonist phase 3 trial promisi ng conrolling psychosis
- 76. RECENT TRIAL • Davunetide , Tideglusib - failed • Droxidopa - orthostatic hypotension –FDA approved • Losartan - supine hypertension - failed
- 77. CLINICAL FEATURES TAUPATHY SYNUCLEOPATHY Age of onset 7th 6th Initial symptoms Postural &gait disorder Tremor & bradykinesia Family history - +/- Multi infarct state +/- - Dementia +/- +/- Downgaze ophthalmoparesis + - Eyelid abnormalities + +/- Pseudobulbar palsy + +/- Gait Wide,stiff,unsteady Slow shuffling,narrow,festinating Rigidity Axial(neck) Generalised Facial expression Astonished,worried Hypomimia Tremor at rest - +/- Dystonia + +/-
- 78. Corticobulbar signs +/- - Symmetry of findings + - Weight loss - + Improvement with DA drugs _ + Levodopa induced dyskinesias _ +
- 86. SUMMARY • Careful clinical examination • AP mimickers • There are currently no biomarkers available. • There are currently no neuroprotective treatments available. • Symptomatic and supportive treatments with usually no sustained effect. • Further research required
- 87. REFERENCES • Eur J Neurol.sciacca g et al, 2018 Aug;25(8):1100-e85. doi:10.1111/ene.13673. Epub 2018 Jun 12. • Litvan I, Hauw JJ, Bartko JJ, et al. Validity and reliability of the preliminary NINDS neuropathologic criteria for progressive supranuclear palsy and related disorders.JNeuropathol Exp Neurol 1996;55(1):97Y105 • Strowd RE, Cartwright MS, Okun MS, et al. • Pseudobulbar affect: prevalence and quality of life impact in movement disorders.J Neurol 2010;257(8):1382Y1387. doi:10.1007/s00415-010-5550-3 • Bradley's Neurology in Clinical Practice,7th ed • Uptodate.com
- 88. Thank you
