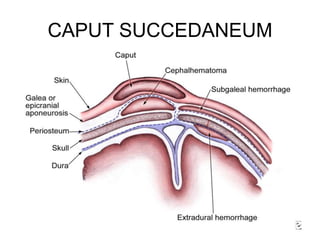
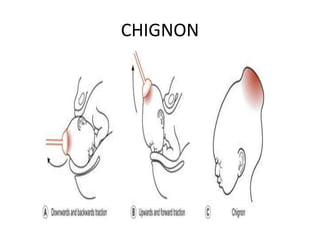
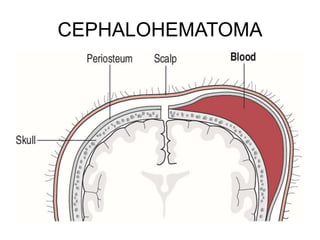
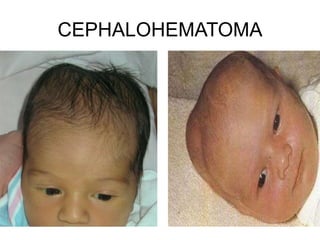
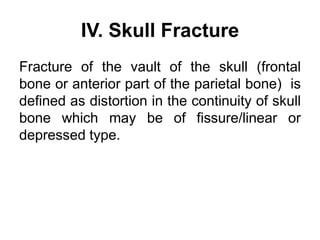
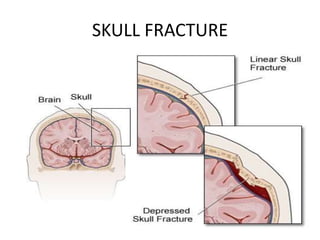
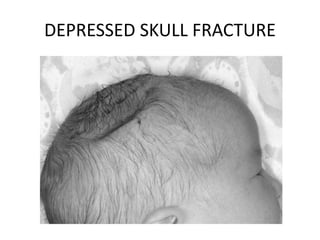
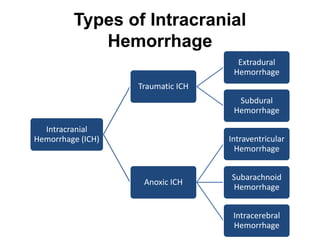
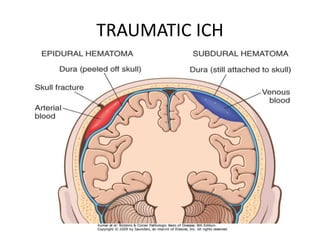
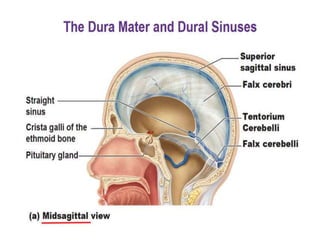
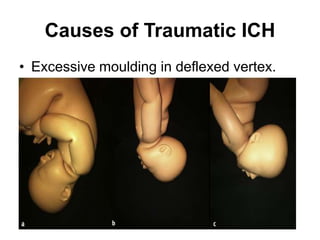
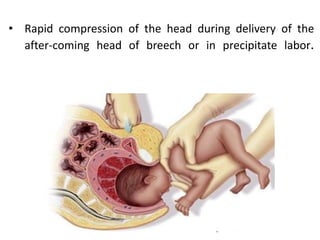
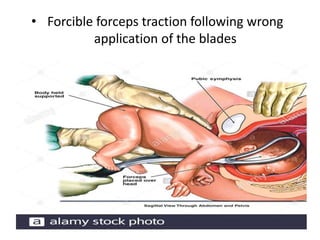
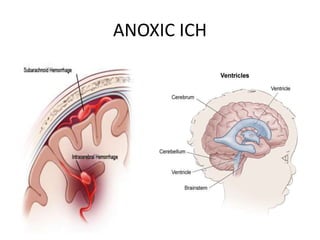
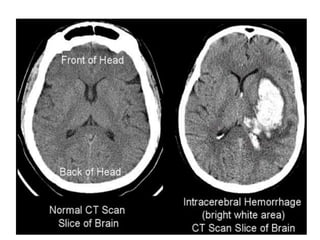
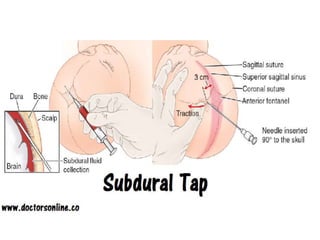
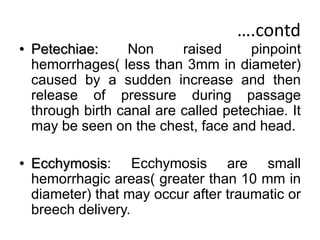
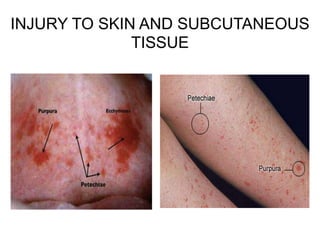
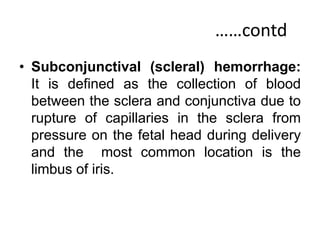
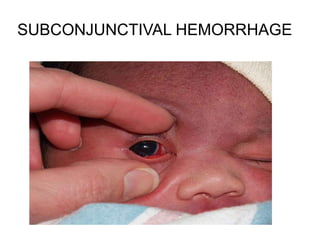
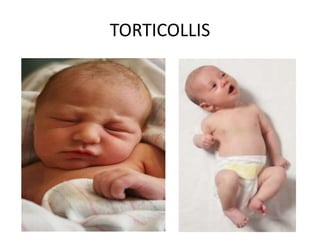
This document discusses various types of birth injuries including skull injuries and soft tissue injuries in newborns. Skull injuries include caput succedaneum, cephalohematoma, scalp injuries, and skull fractures. Soft tissue injuries involve the skin, subcutaneous tissues, muscles, and visceral organs. Intracranial hemorrhages are also described, which can be traumatic, anoxic, or involve the ventricles, subarachnoid space, or brain tissue. Risk factors, clinical features, diagnosis, and management are provided for each type of injury.