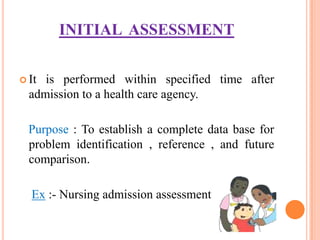
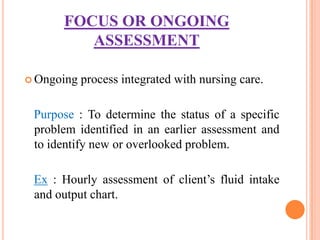
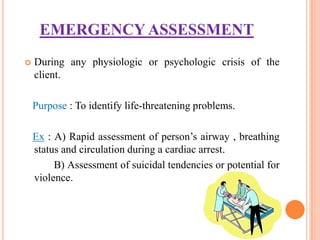
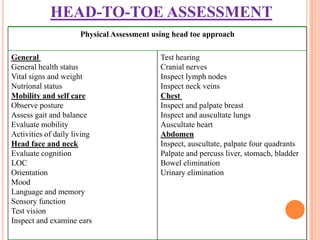
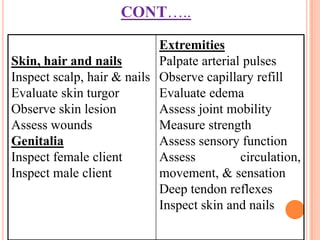
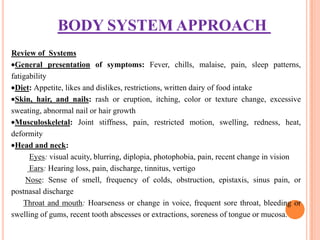
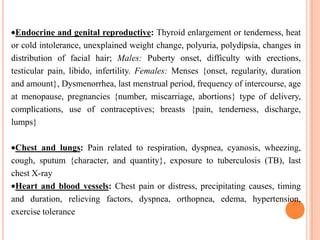
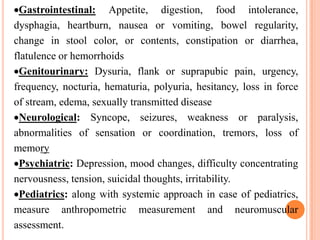
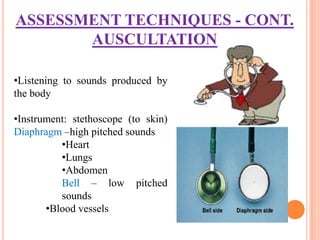
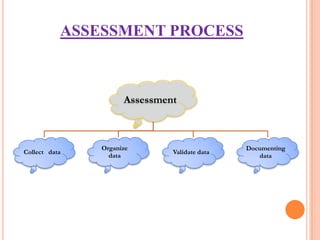
Nursing assessment involves collecting data to understand a patient's health status. It includes gathering subjective information from the patient and objective data through examination. The nurse organizes, validates, and documents the assessment data to identify health problems, strengths, and needs to develop an appropriate plan of care. Common assessment techniques are inspection, palpation, percussion, and auscultation to examine each body system.