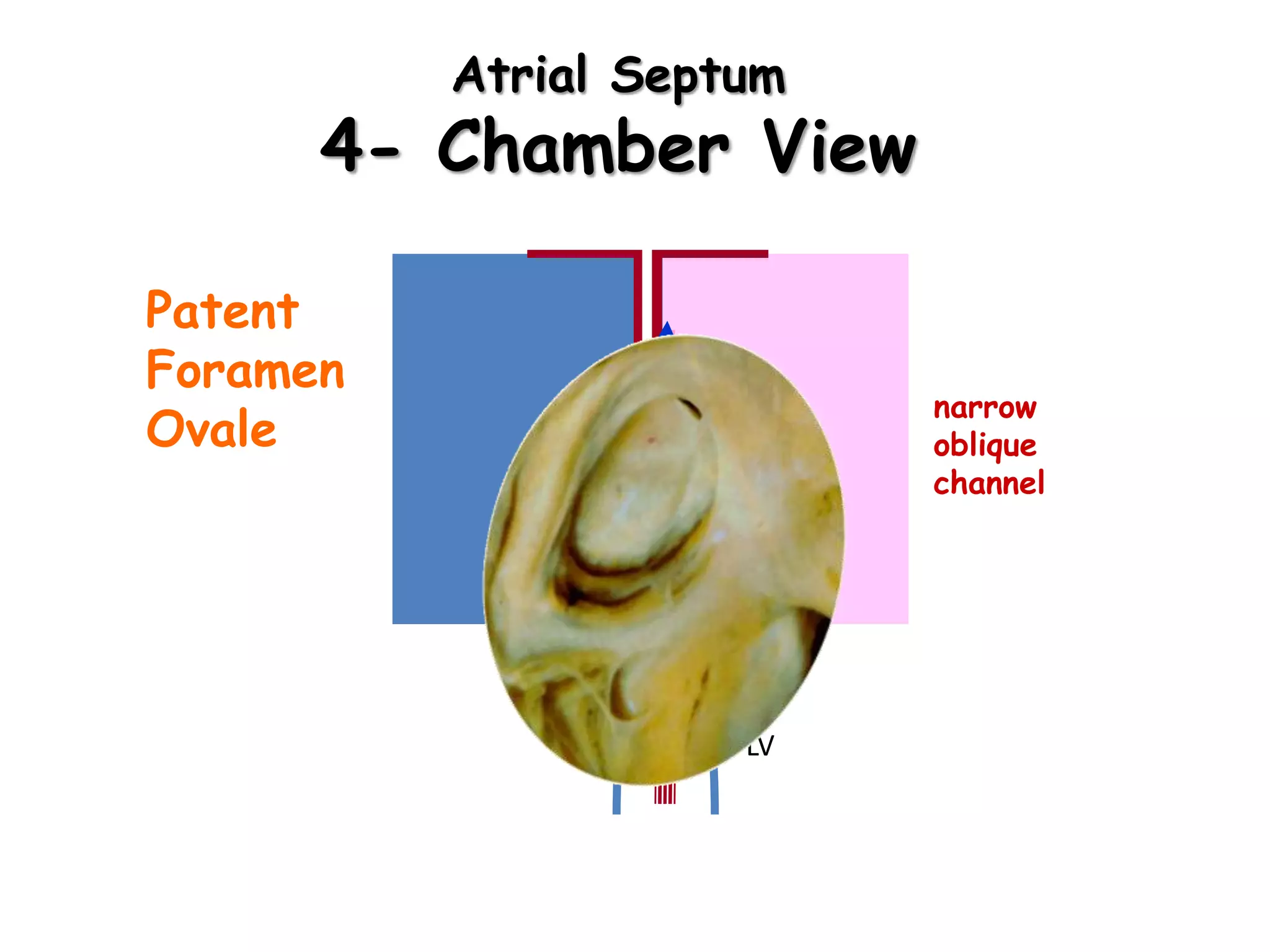
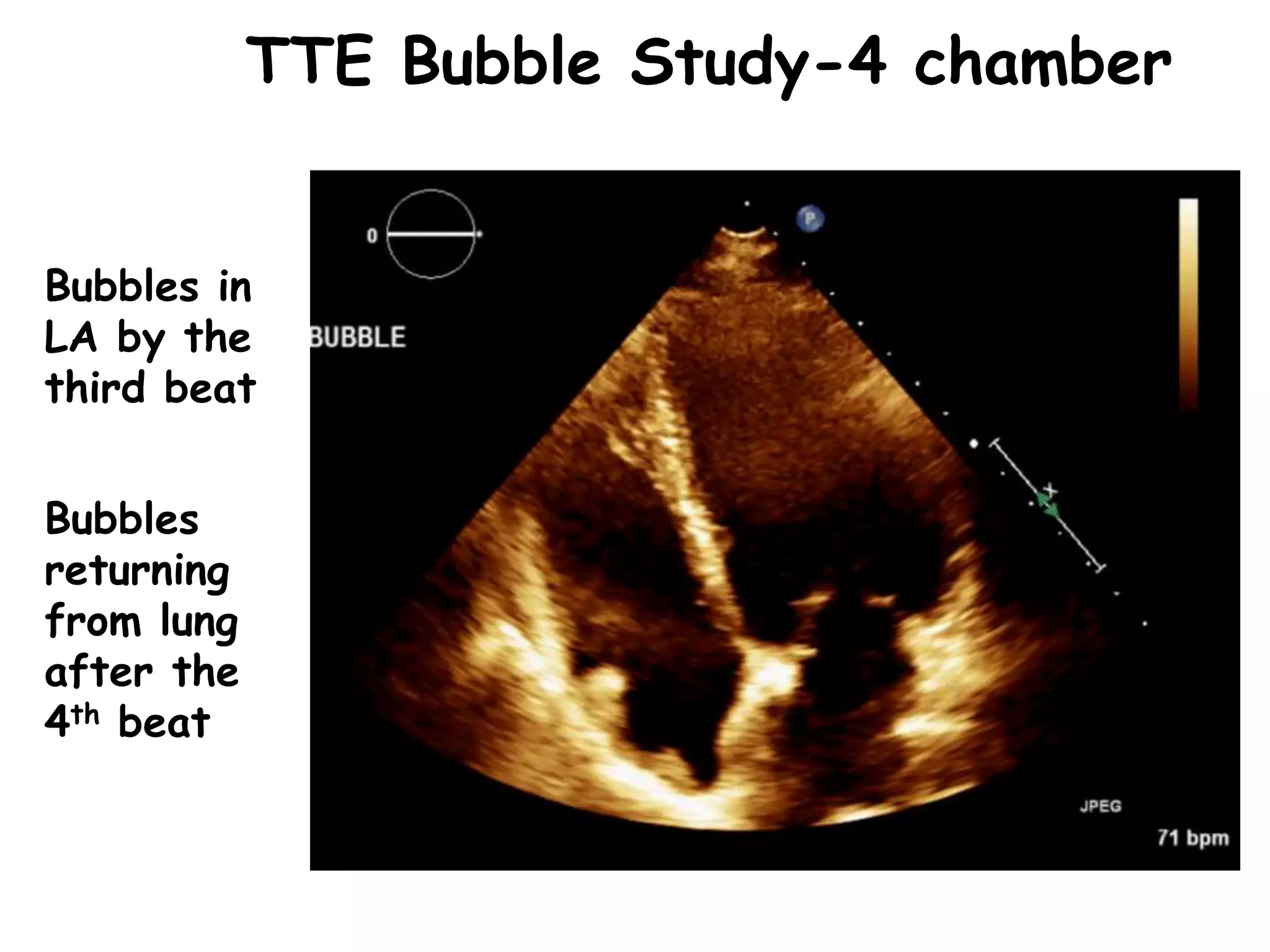
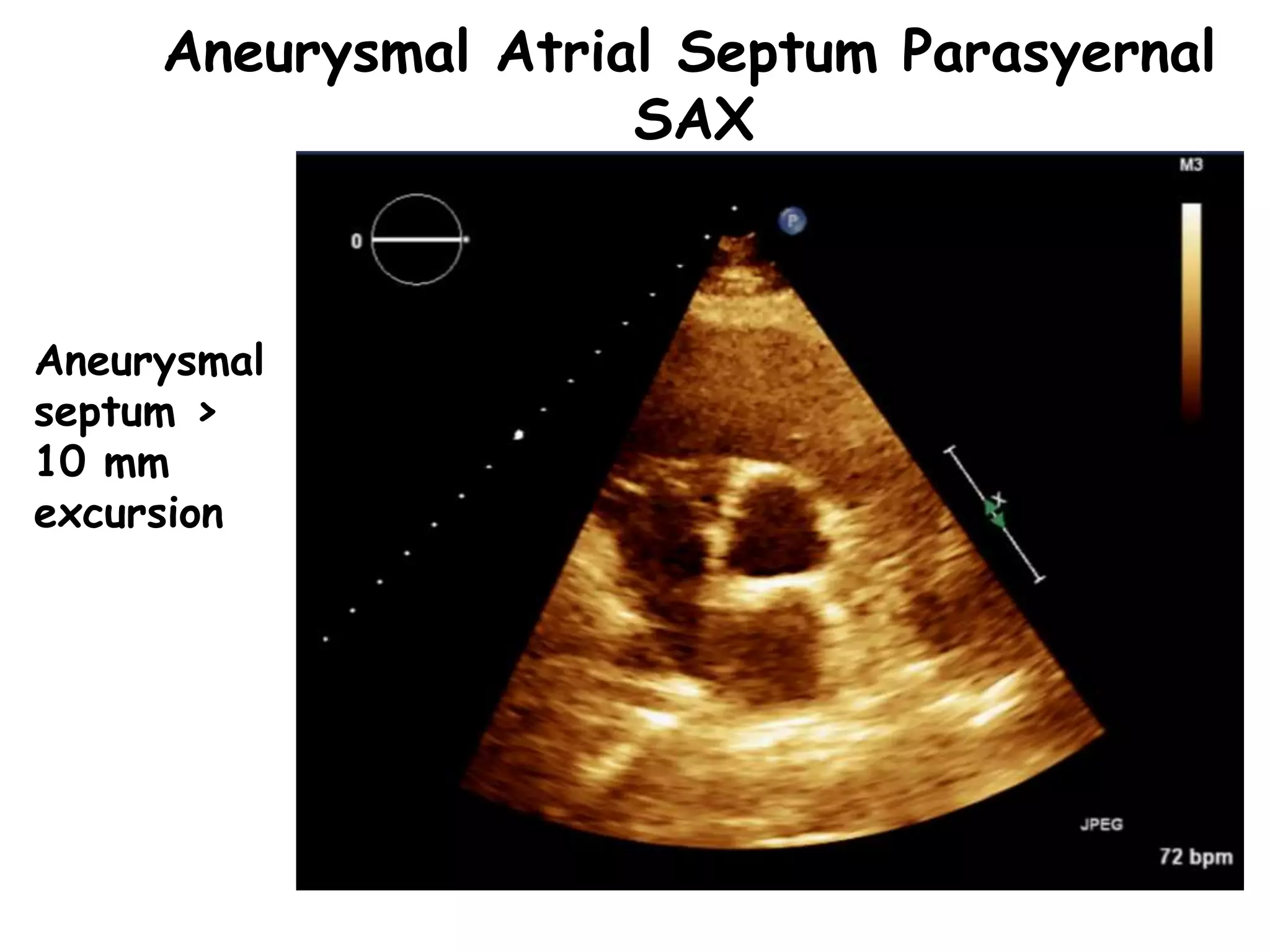
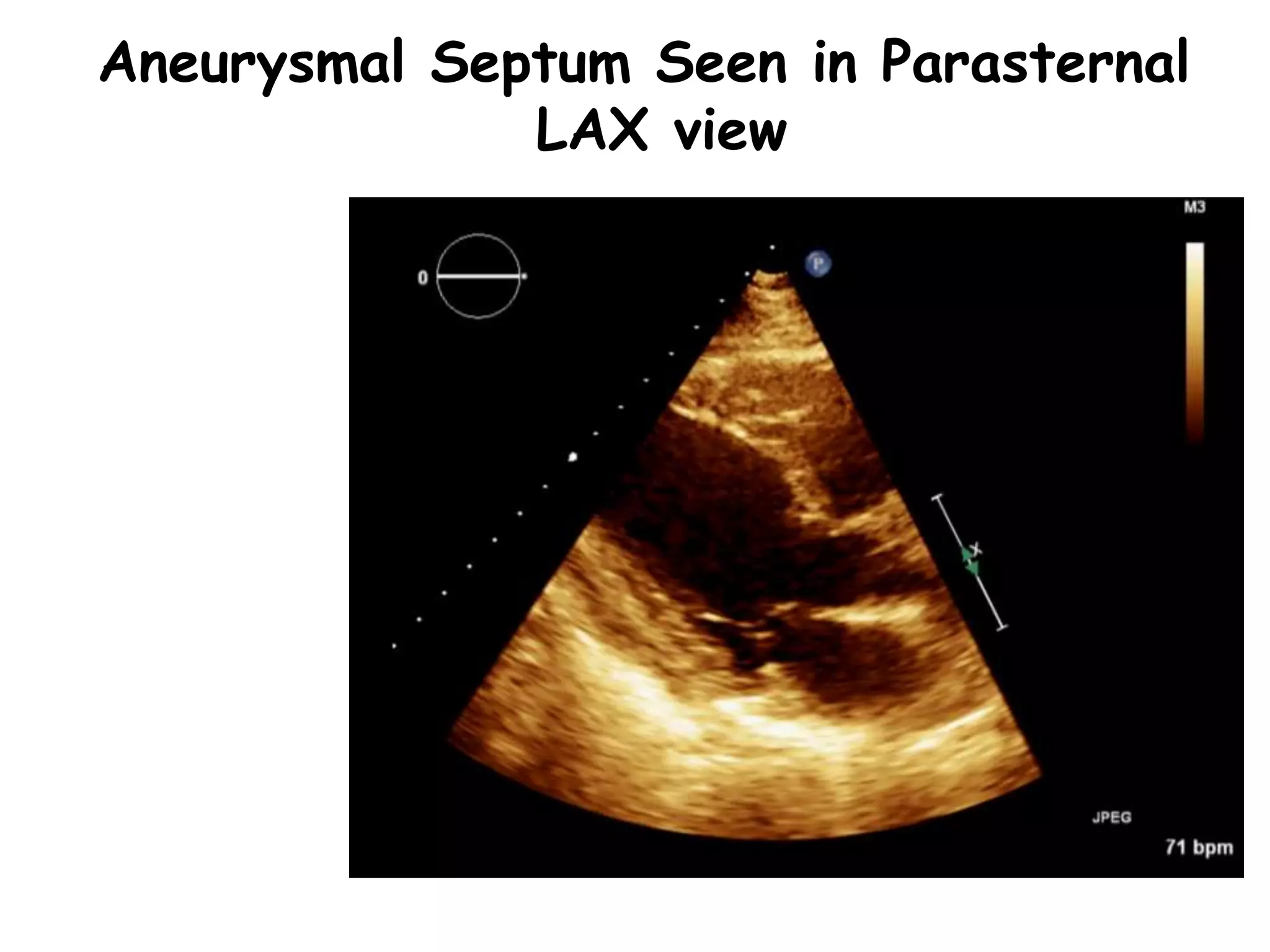
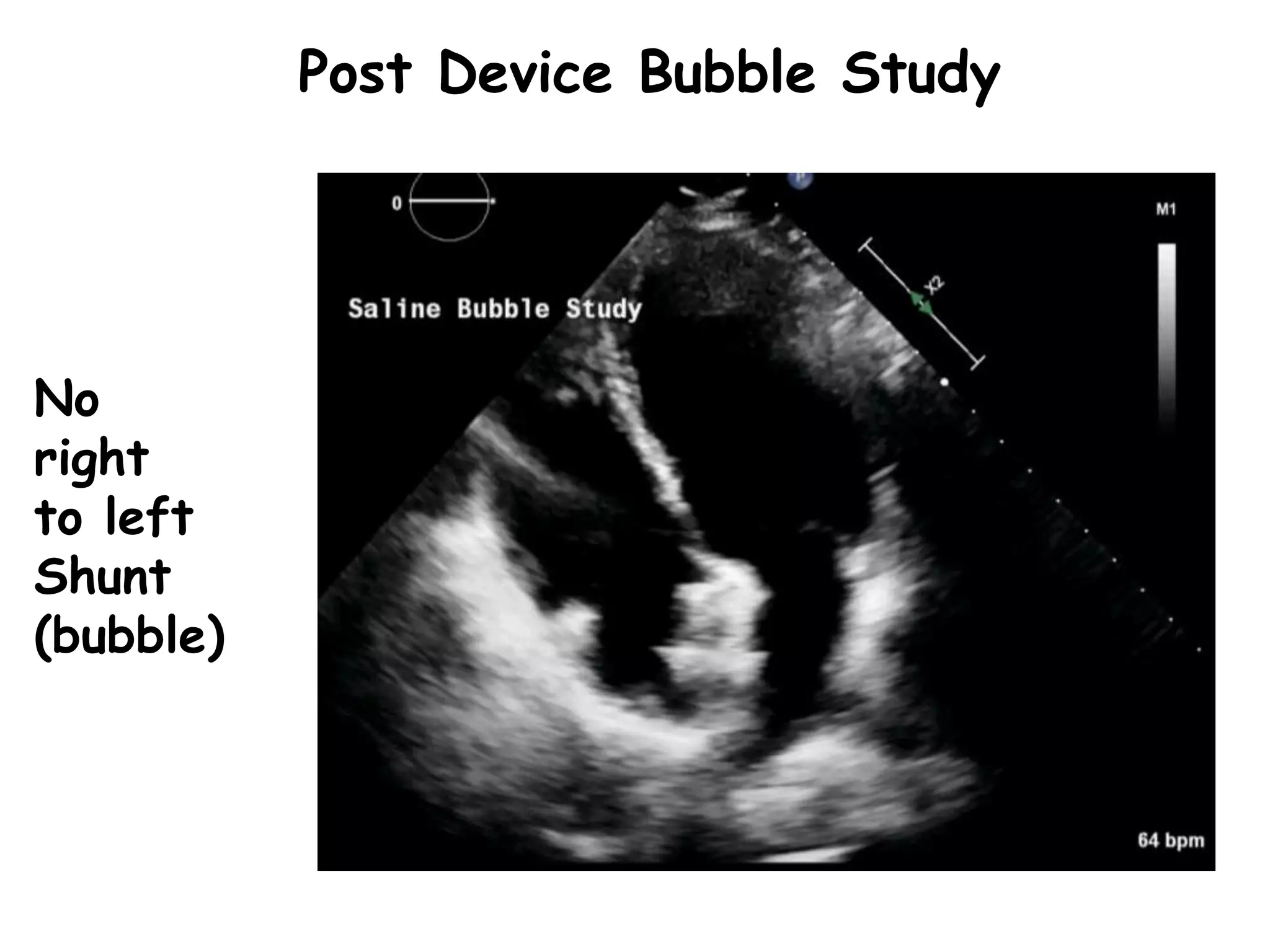
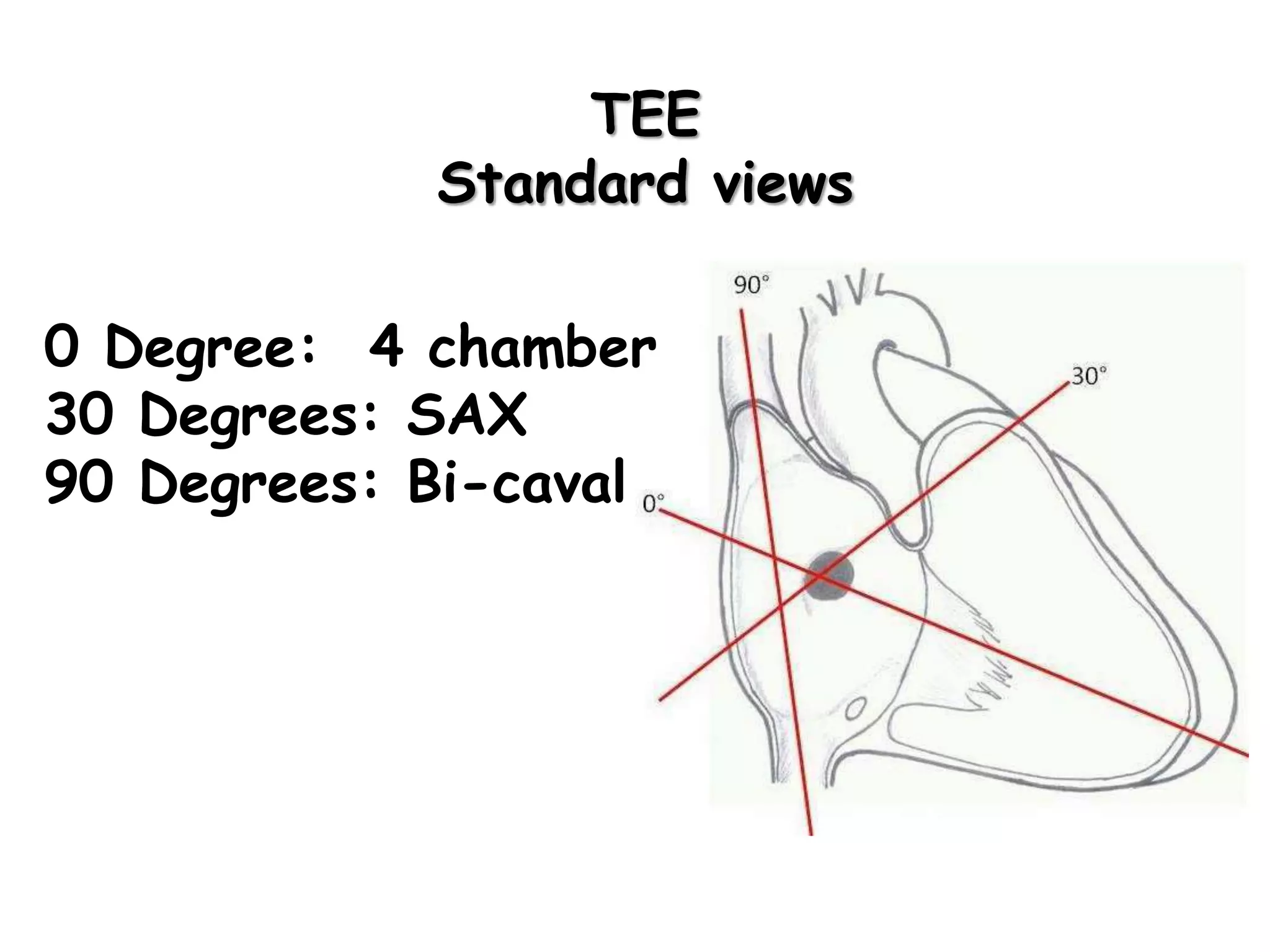
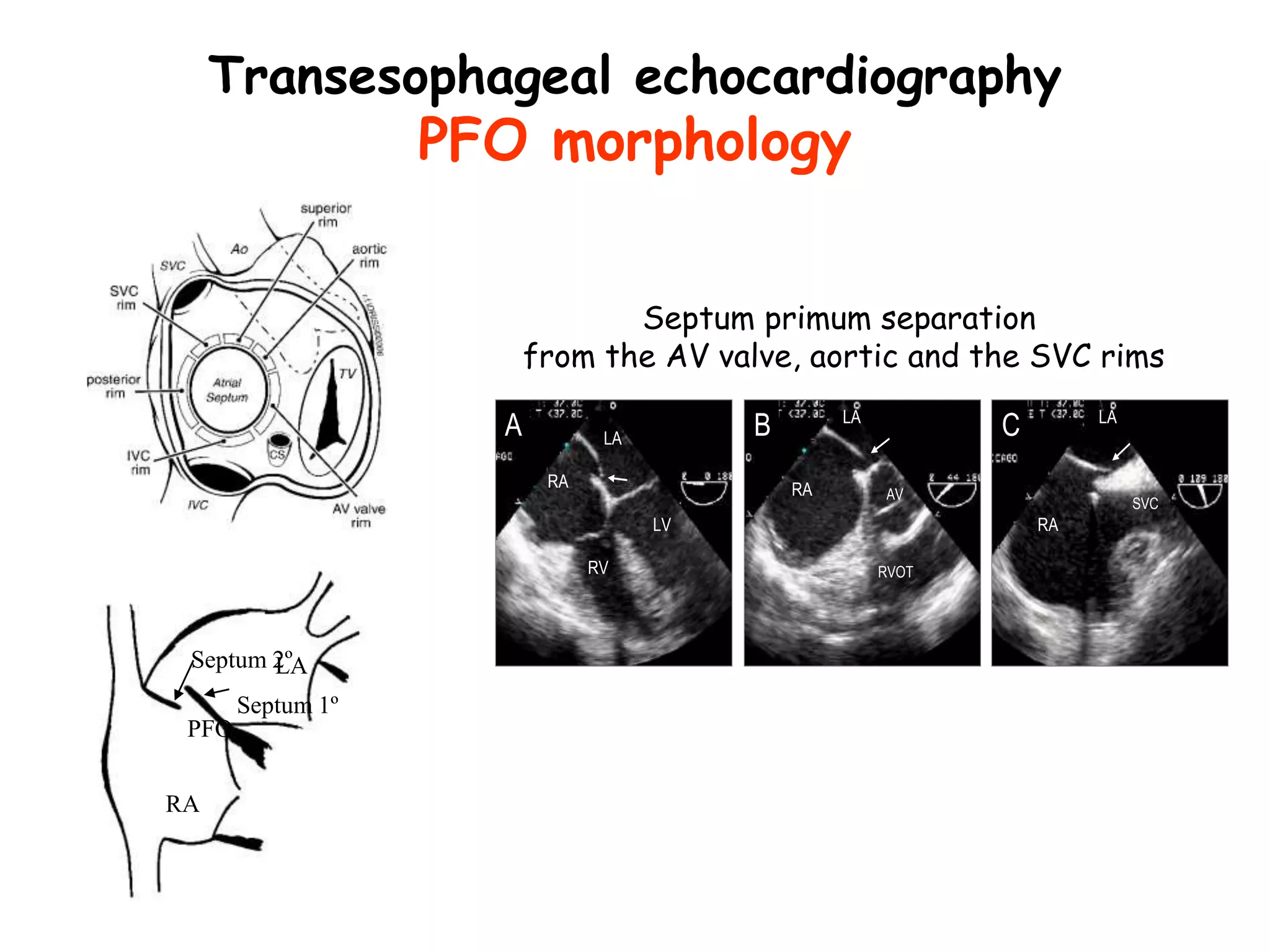
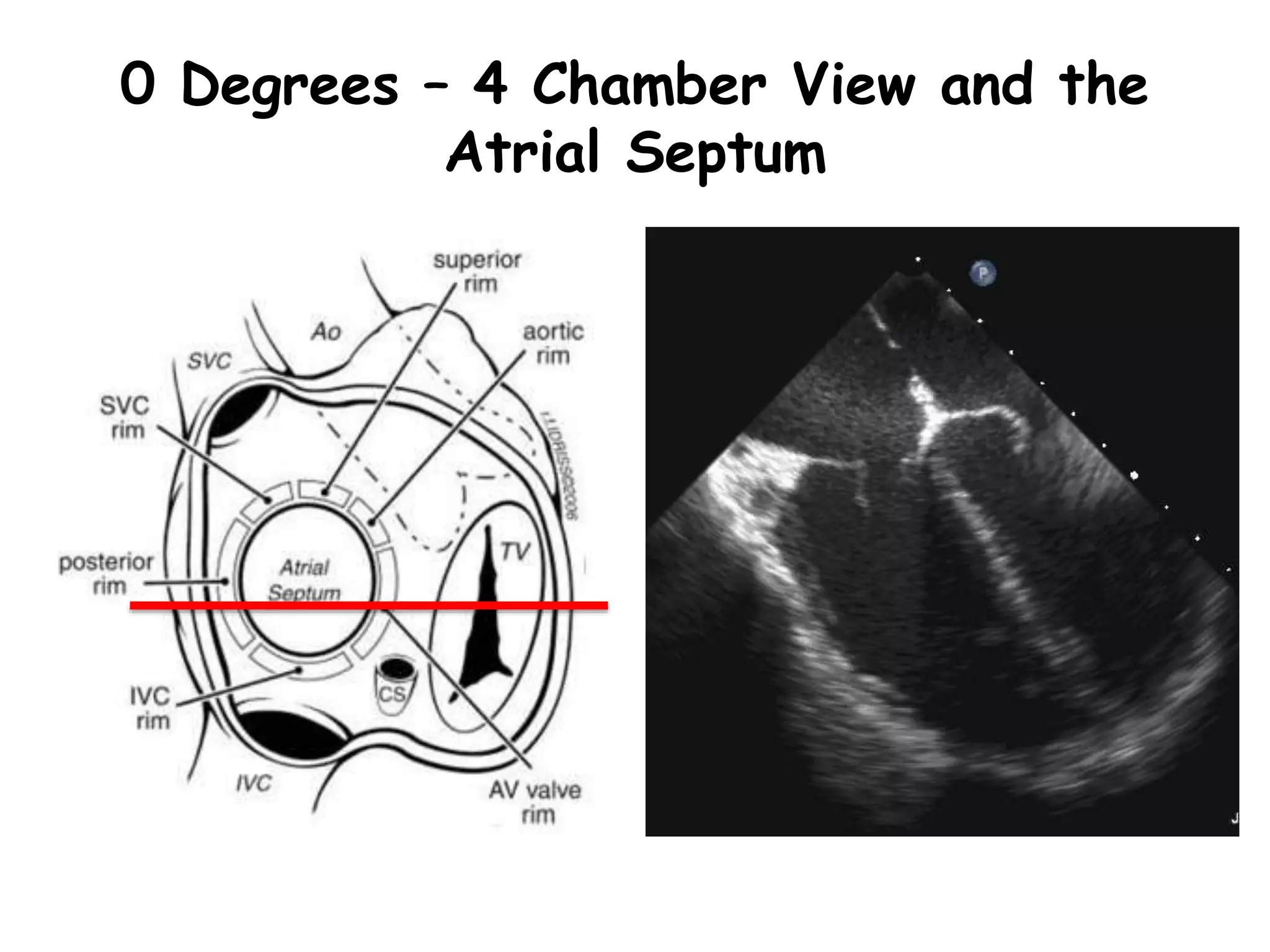
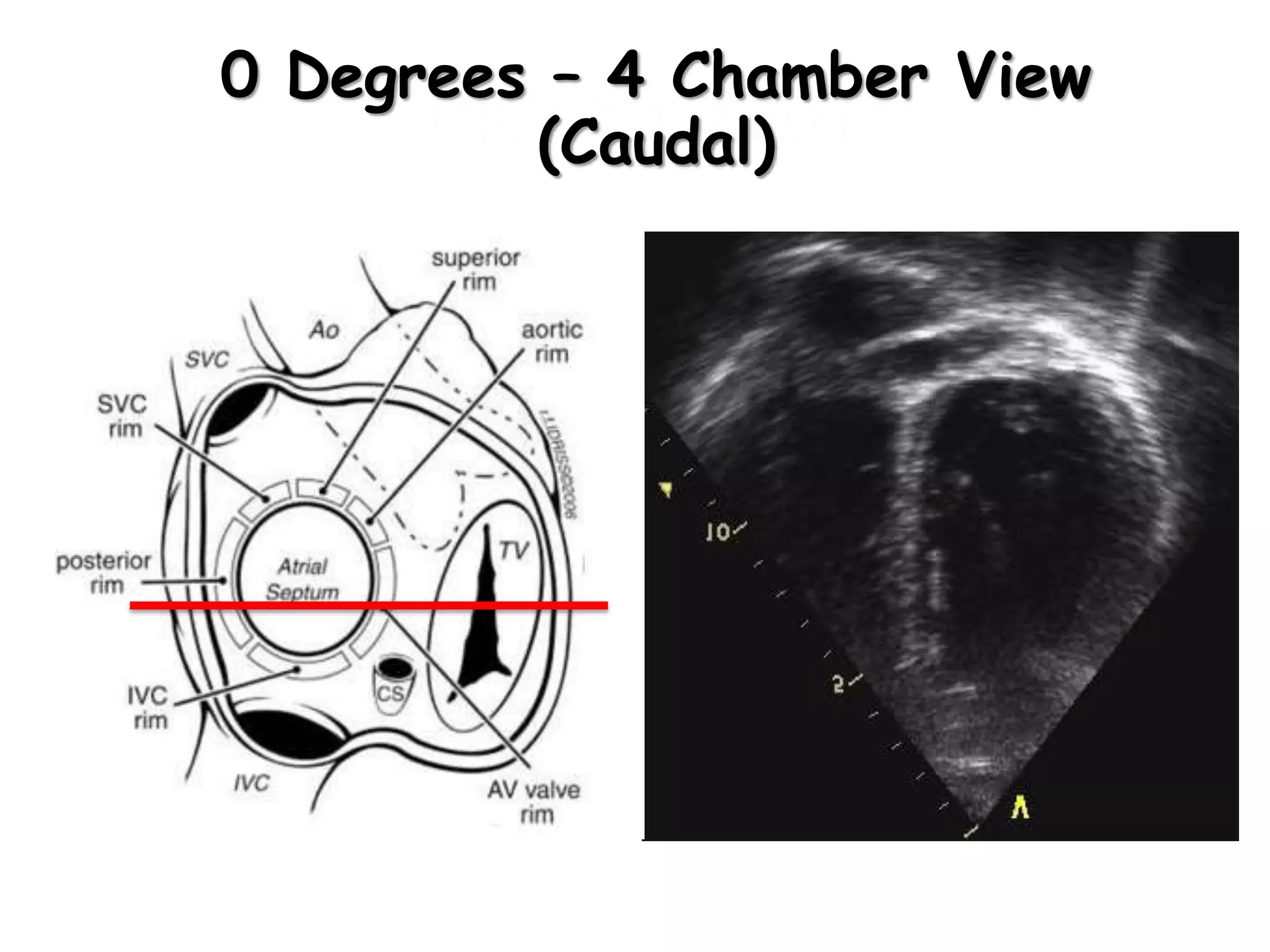
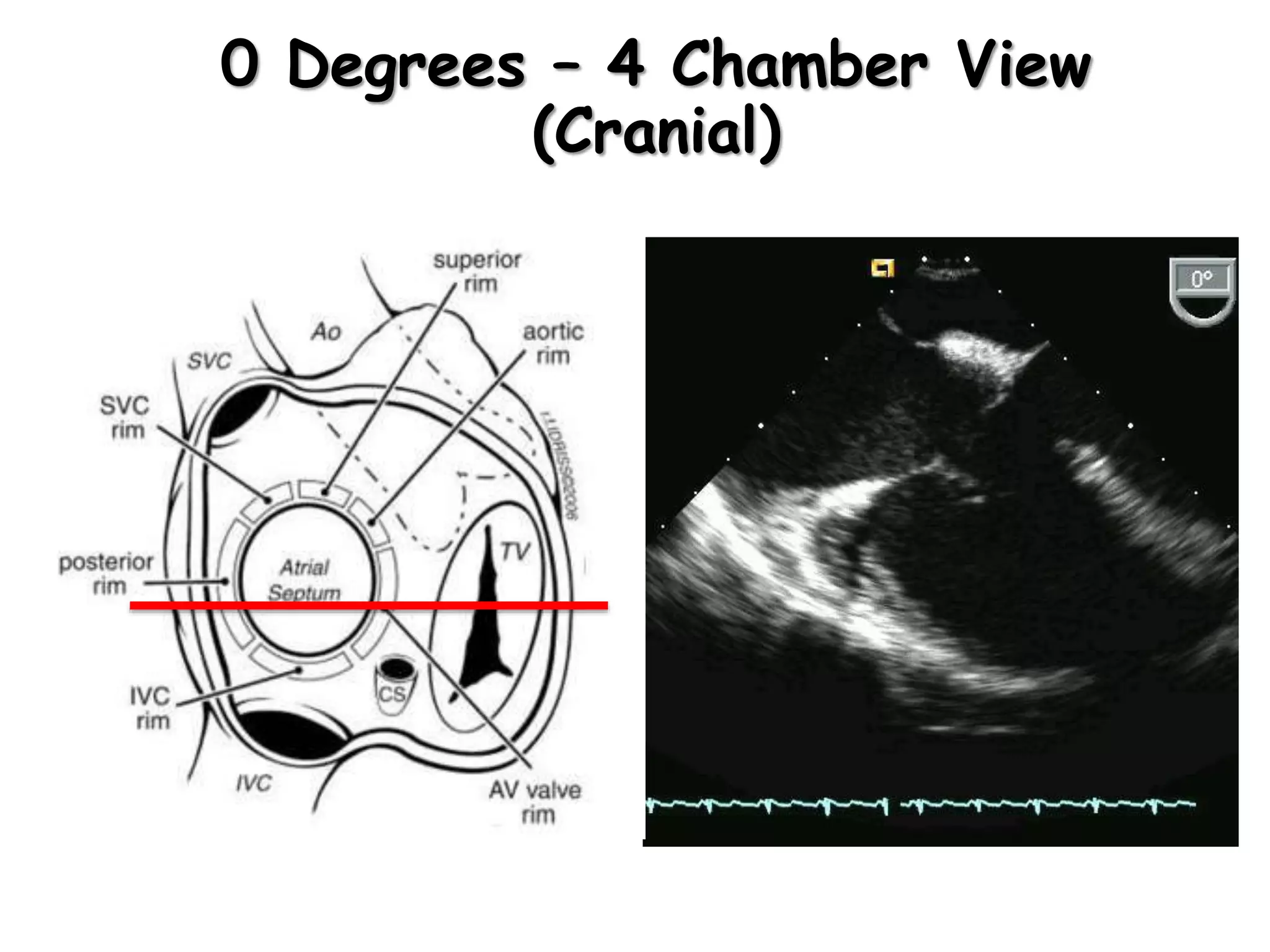
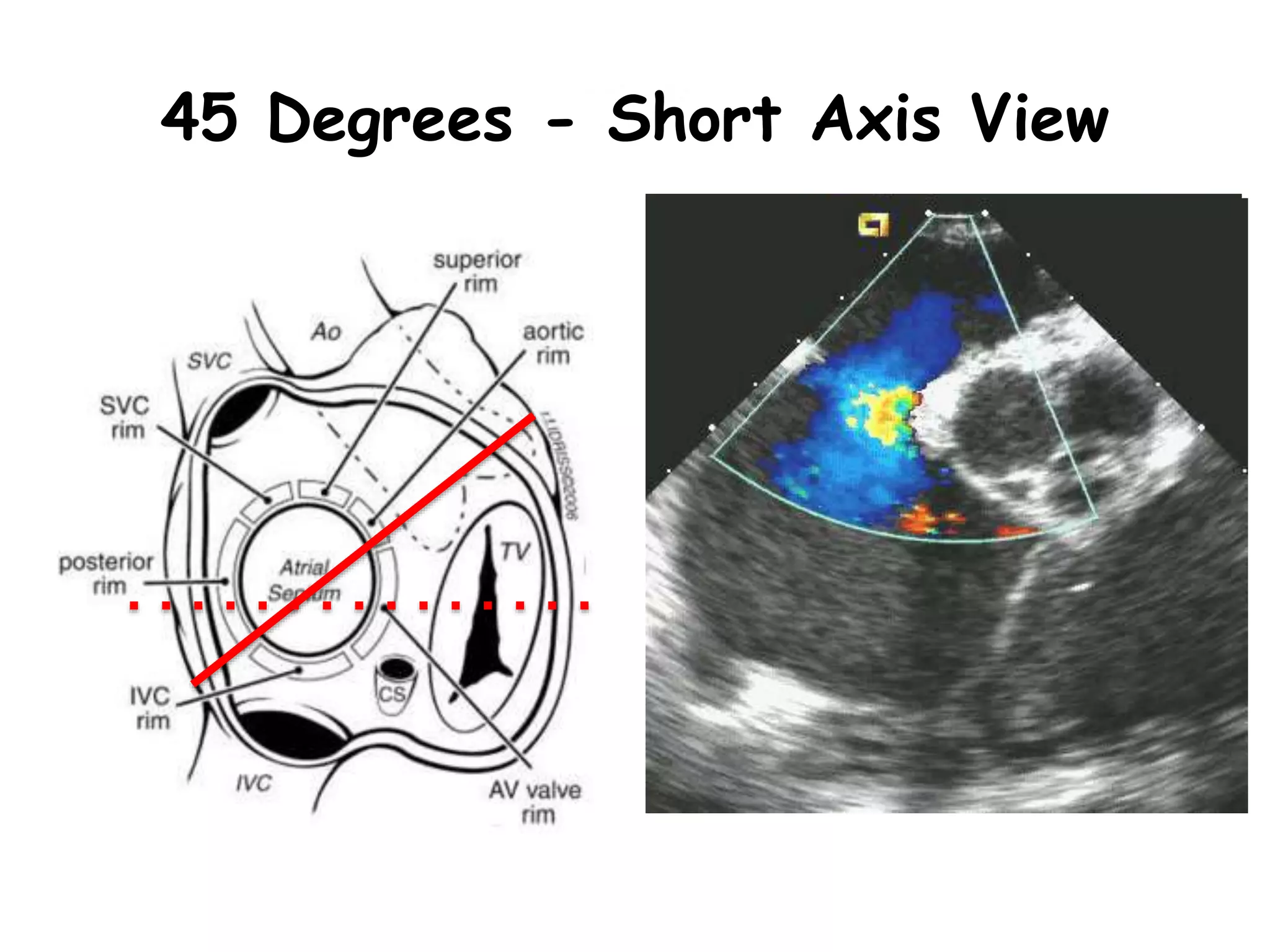
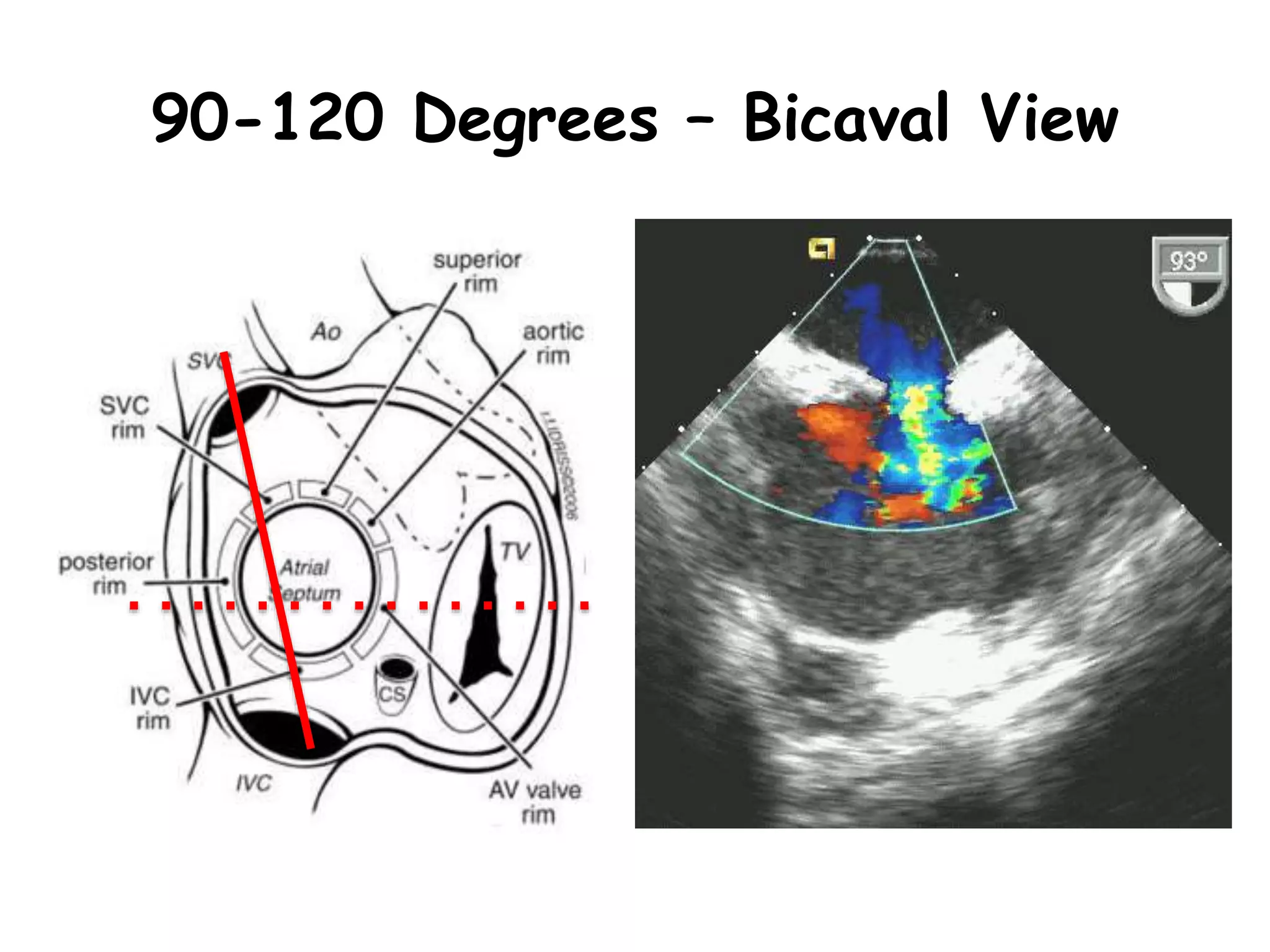
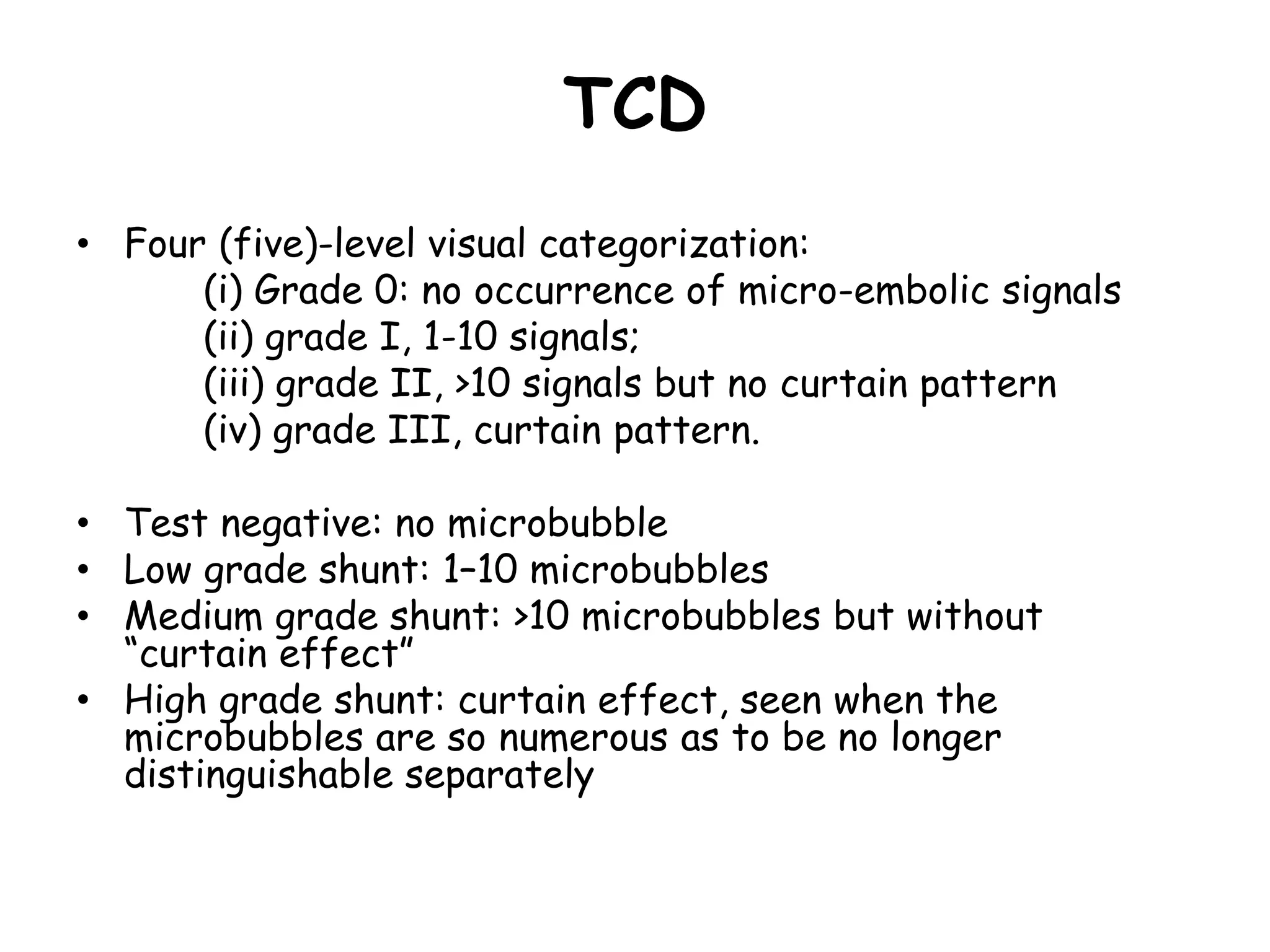
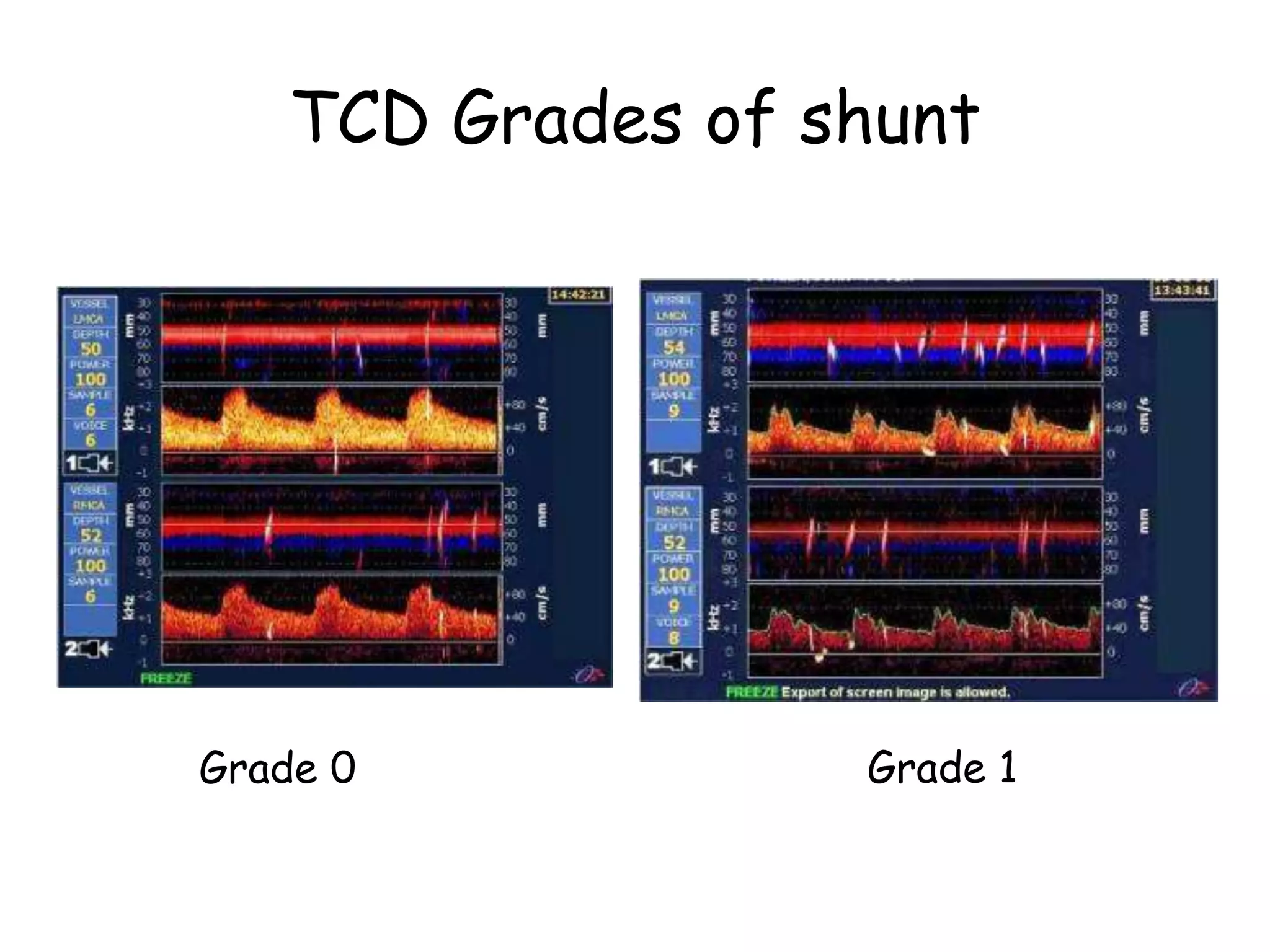
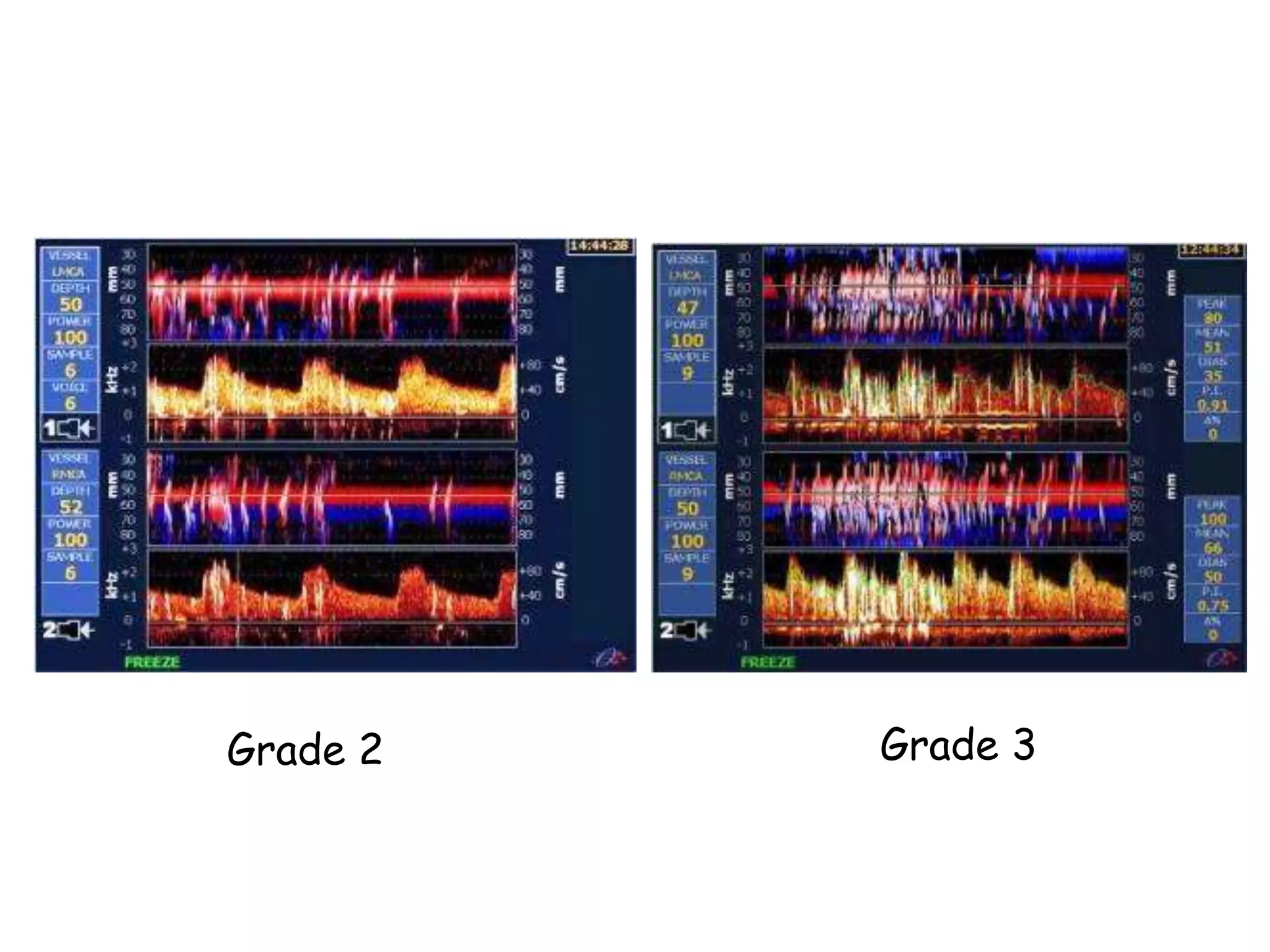
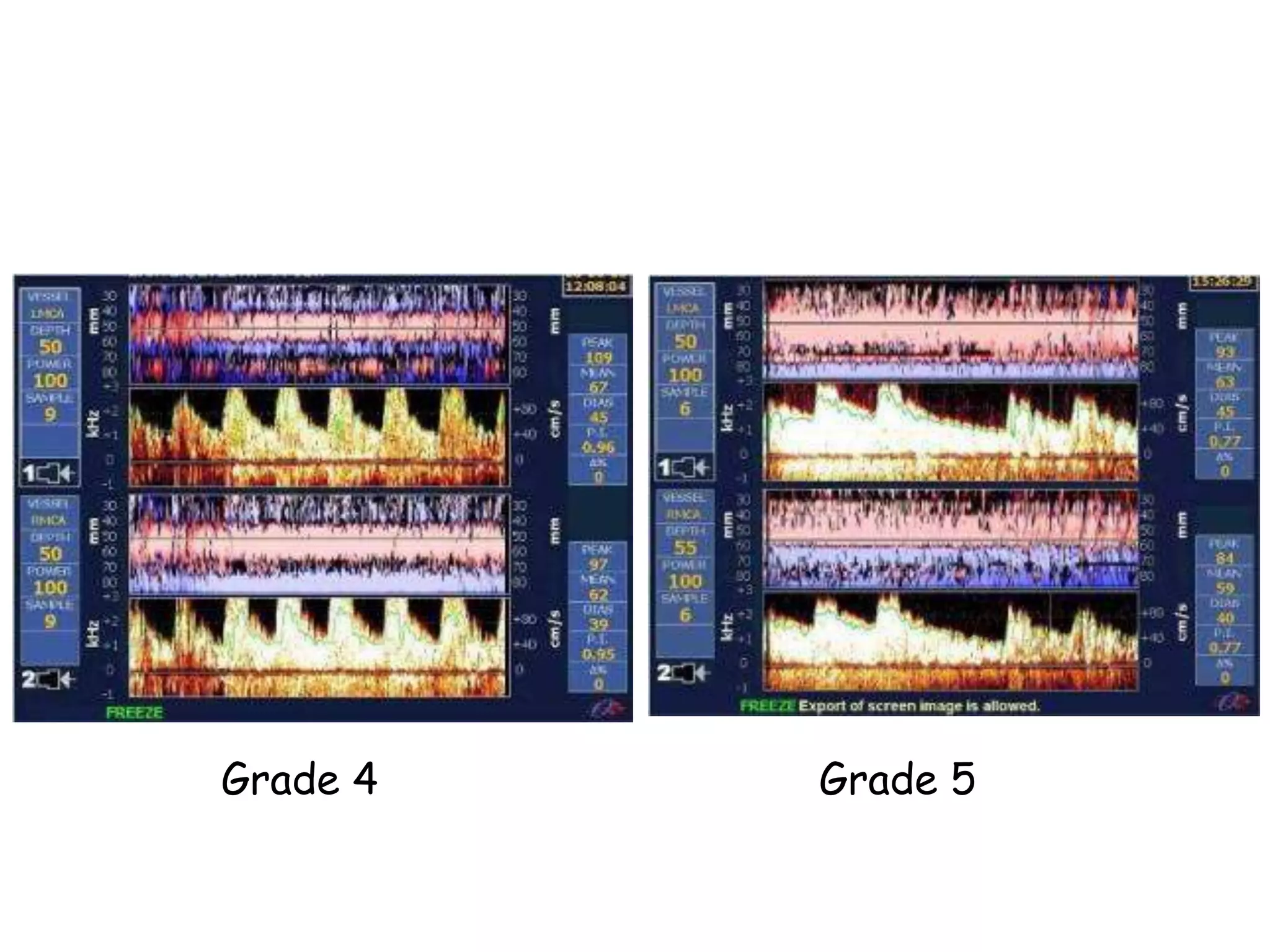
TTE, TEE, and TCD can be used to characterize PFOs. TTE can diagnose a PFO but may not provide detailed anatomy. TEE provides excellent images of PFO size, extension, tunnel characteristics. It is very useful for sizing and closing PFOs. TCD uses Doppler ultrasound to detect microbubbles passing through the brain during a Valsalva maneuver after injecting agitated saline. It grades the amount of right to left shunting from 0 to 3 or 5 but requires trained personnel. While not required, TCD can provide additional useful information about high grade shunts when evaluating PFOs.