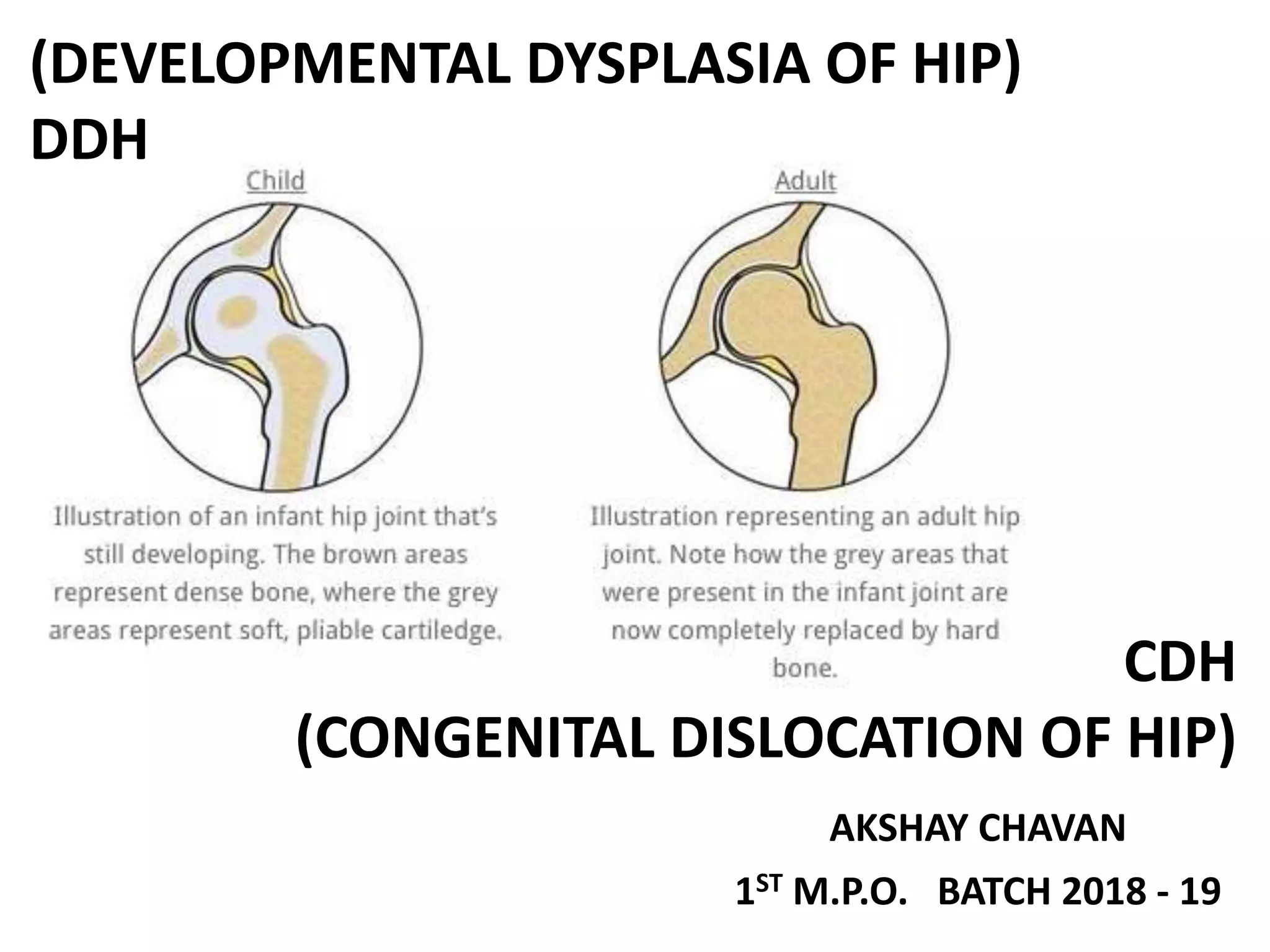
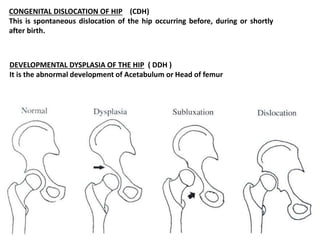
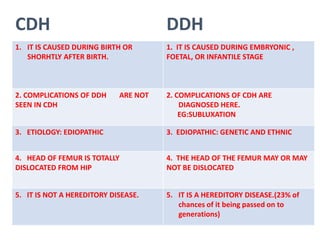
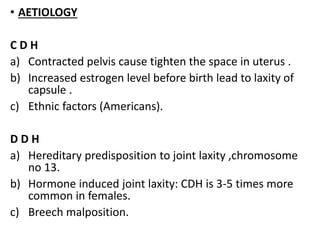
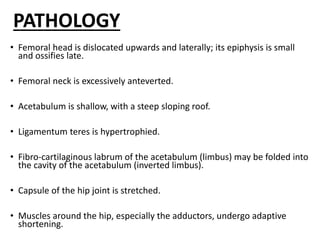
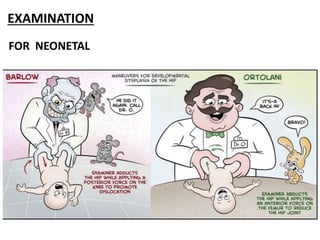
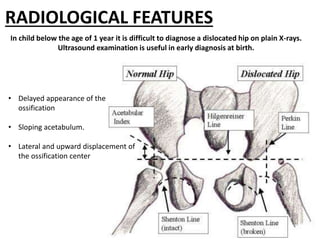
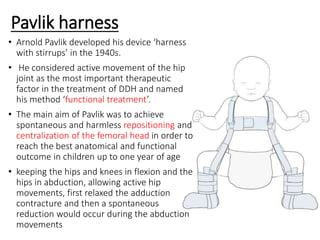
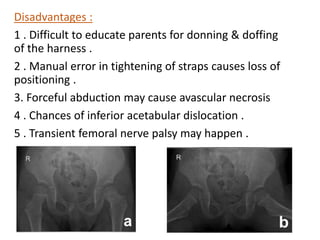
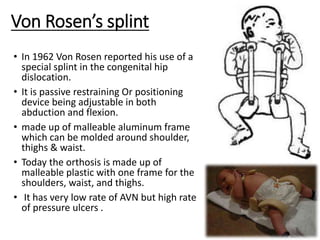
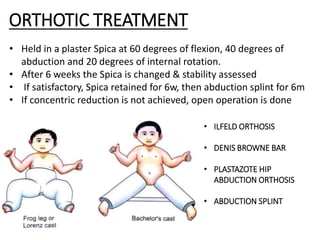
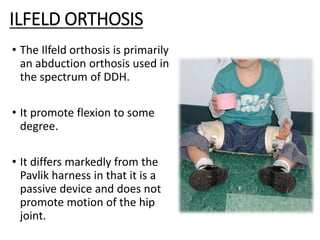
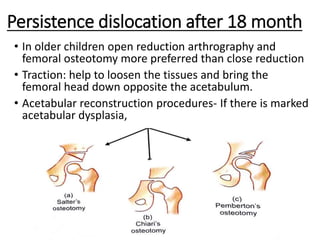
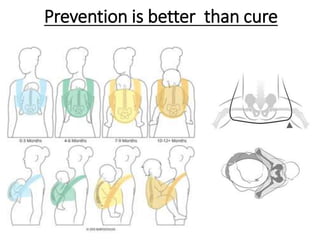
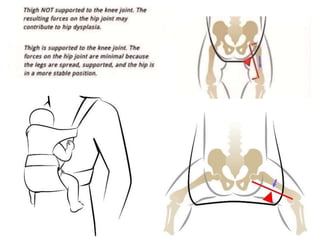
This document provides information on congenital dislocation of the hip (CDH) and developmental dysplasia of the hip (DDH). It discusses the causes, signs, symptoms, examination findings, treatment options including orthotic interventions like the Pavlik harness and Frejka pillow. CDH occurs at or shortly after birth while DDH develops during the embryonic, fetal or infantile stage. Treatment aims to achieve and maintain reduction of the femoral head into the acetabulum through splinting or bracing until the hip joint stabilizes.