The patient was a 36-year old man with a BMI of 44 kg/m2 who was referred for weight loss advice. During the initial assessment, the dietitian realized she made assumptions about the patient's capabilities rather than truly understanding his perspective, which revealed opportunities to improve. Upon reflection using Gibbs' reflective cycle and reviewing literature, the dietitian developed an action plan to better assess readiness to change, set tailored goals, and refer to other services to integrate this learning into her future practice.







![References
UK Department of Health (2006) Care pathway for the management of
overweight and obesity. London: DH.
Weigh Management Interest Group, INDI (2007) Position of the Irish
Nutrition and Dietetics Institute: weigh management. Available at:
http://www.indi.ie/docs/979_94_wmig.pdf [accessed March 16th 2012]
Grace C, Pearson D et al. (2008) DOM, UK: The Dietetic Weight
Management Intervention for Adults in the One to One Setting: is it time
for a radical rethink? Available at: www.domuk.org/docs/dietetic-
interventionfinalversion301007.doc [accessed March 18th, 2012]
Grace, C. (2011), A review of one-to-one dietetic obesity management
in adults. Journal of Human Nutrition and Dietetics, 24: 13–22.
doi: 10.1111/j.1365-277X.2010.01137.x](https://image.slidesharecdn.com/reflectivepracticepresentation-121230191326-phpapp01/85/Reflective-Practice-Presentation-10-320.jpg)
![References
Rolfe et al. (2001) Framework for reflective practice, as cited by Students
Learning with Communities: information for students: resources. Available
at: http://www.communitylinks.ie/students-learning-with-
communities/information-for-students/resources/
[accessed March 23rd, 2012]
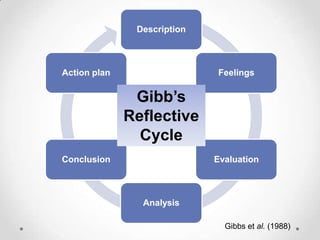
Gibbs et al. (1988) Gibb’s Reflective Cycle, as cited by Students Learning
with Communities: information for students: resources. Available at:
http://www.communitylinks.ie/students-learning-with-
communities/information-for-students/resources/
[accessed March 23rd, 2012]](https://image.slidesharecdn.com/reflectivepracticepresentation-121230191326-phpapp01/85/Reflective-Practice-Presentation-11-320.jpg)
