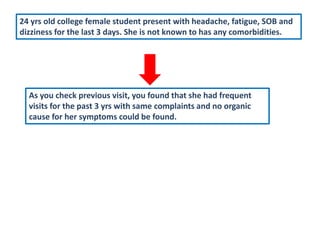
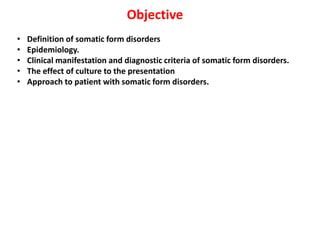
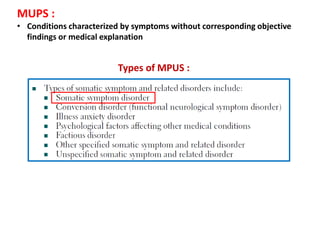
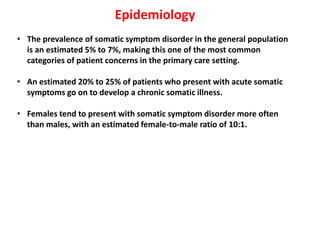
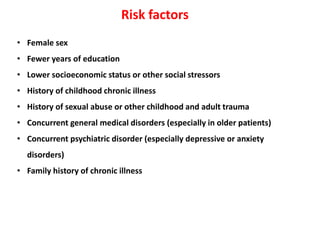
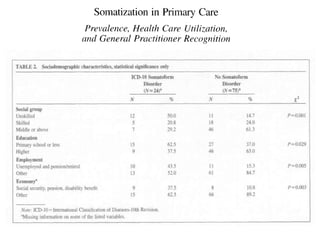
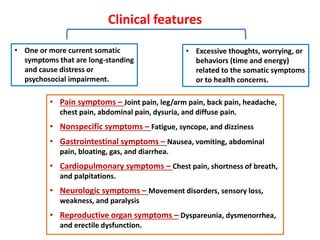
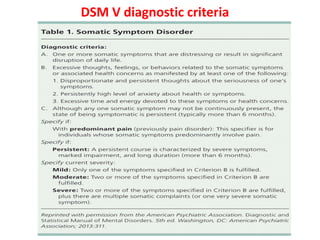
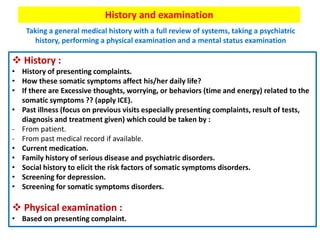
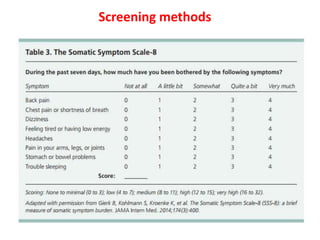
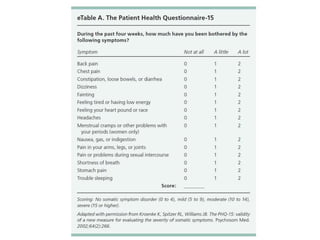
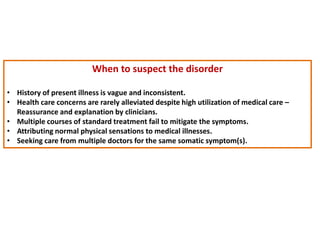
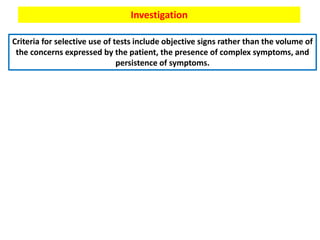
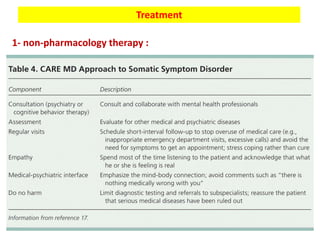
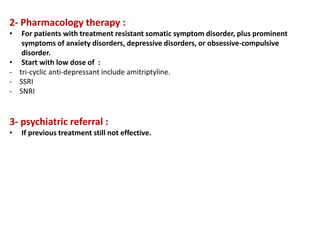
This document discusses medically unexplained physical symptoms (MUPS) and somatic symptom disorder. It defines MUPS as physical symptoms that exist without objective medical findings or explanations. Somatic symptom disorder is characterized by physical symptoms caused by psychological or emotional distress. The document reviews the epidemiology, risk factors, clinical features, diagnostic criteria, cultural influences, and approaches for evaluating and treating patients with somatic symptom disorder.