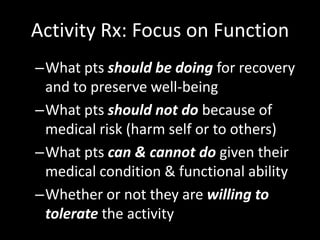
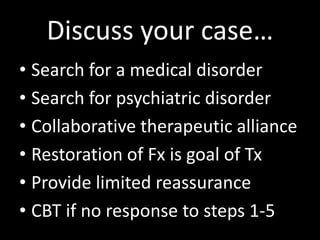
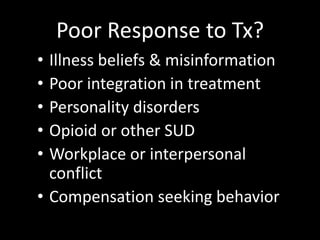
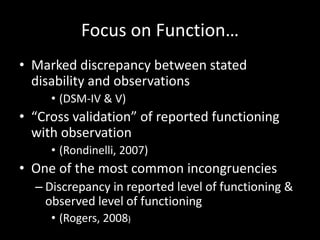
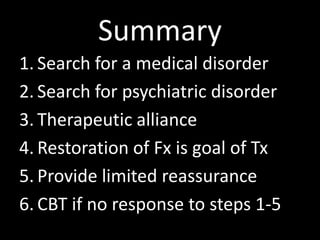
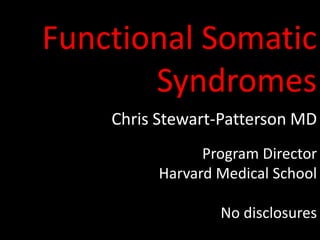
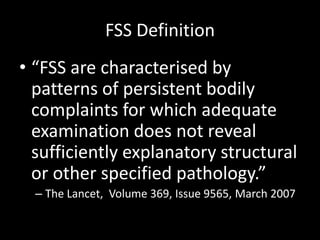
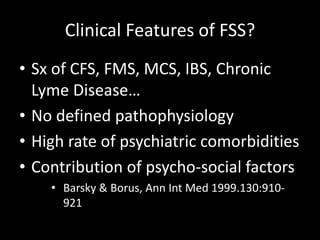
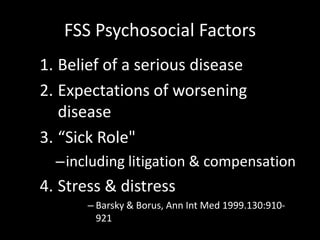
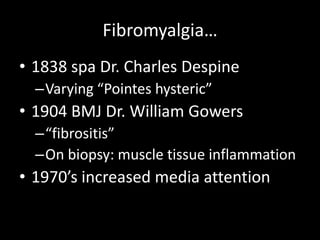
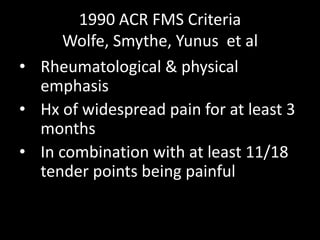
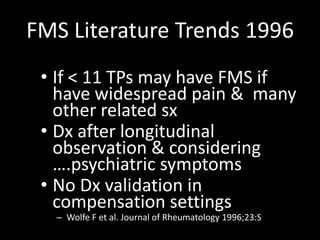
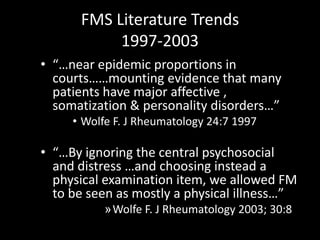
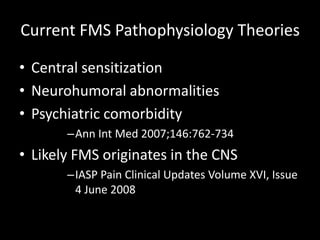
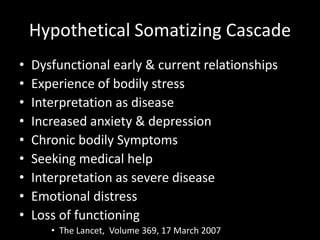
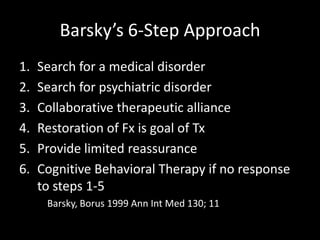
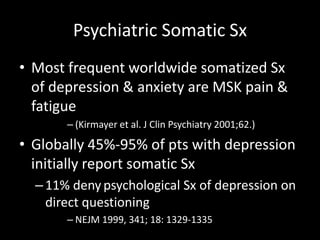
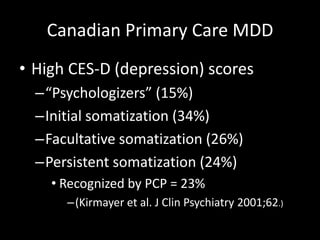
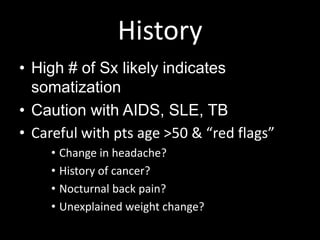
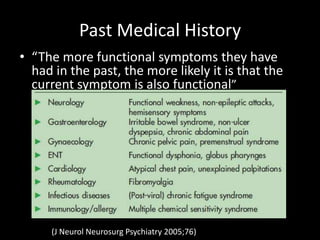
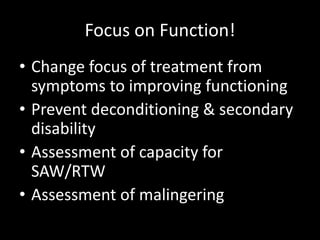
This document discusses functional somatic syndromes (FSS), conditions characterized by medically unexplained physical symptoms. It provides an overview of several FSS including fibromyalgia, chronic fatigue syndrome, and irritable bowel syndrome. While the pathophysiology of FSS is not fully understood, they often involve central sensitization and are commonly associated with psychiatric comorbidities. The document emphasizes taking a biopsychosocial approach to FSS that focuses on function rather than symptoms, includes limited reassurance and cognitive behavioral therapy, and considers potential psychosocial contributing factors. Proper evaluation involves screening for medical and psychiatric disorders, with treatment aiming to improve functioning rather than solely reducing symptoms.
![Difficult Encounters
• MUS & high somatic Sx counts
• 2-3 times more likely to have a
depressive or anxiety disorder
• A stepped care approach may
improve care & enhance physician
satisfaction
• Kroenke. J Clin Psychiatry 2003;5 [suppl 7]: 11–
18)](https://image.slidesharecdn.com/session4-stewart-pattersonfunctionalsomaticsyndromes-140414211653-phpapp02/85/Session-4-stewart-patterson-functional-somatic-syndromes-5-320.jpg)




![Disability Days in Last 3 months
• (Kroenke J Clin Psychiatry 2003;5[suppl 7]: 11–18)](https://image.slidesharecdn.com/session4-stewart-pattersonfunctionalsomaticsyndromes-140414211653-phpapp02/85/Session-4-stewart-patterson-functional-somatic-syndromes-39-320.jpg)