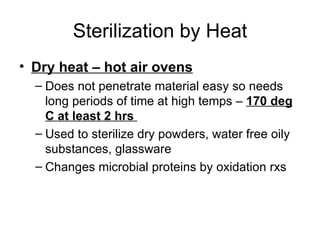
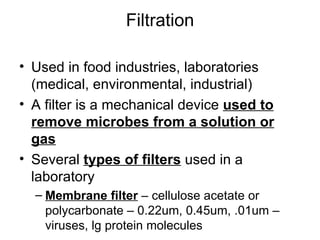
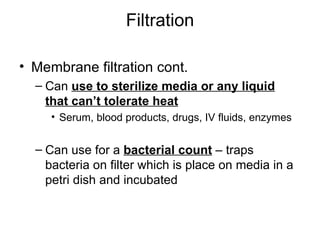
There are three main methods for controlling microbial growth: sterilization, disinfection, and antisepsis. Sterilization completely kills all microbes, including endospores. Disinfection reduces pathogens but not endospores. Antisepsis uses chemicals to prevent infection of living tissues. Common sterilization methods include heat, filtration, radiation, and chemicals. Heat sterilization uses autoclaves and dry heat, while pasteurization reduces pathogens in foods. Filtration and membranes remove microbes from liquids and air. Chemicals and heavy metals disrupt membranes and proteins. Proper control of microbes is important in medicine and food preparation.