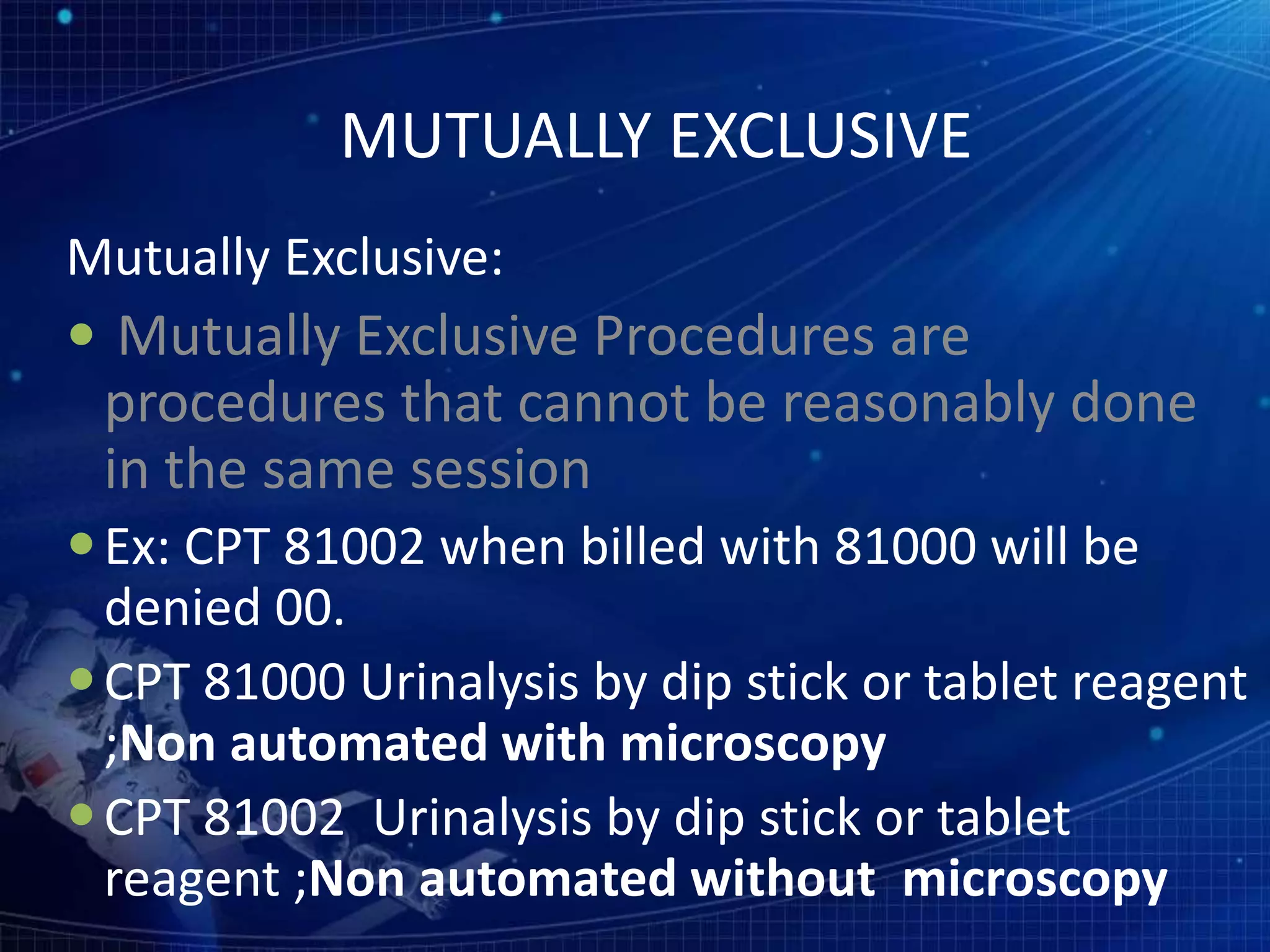
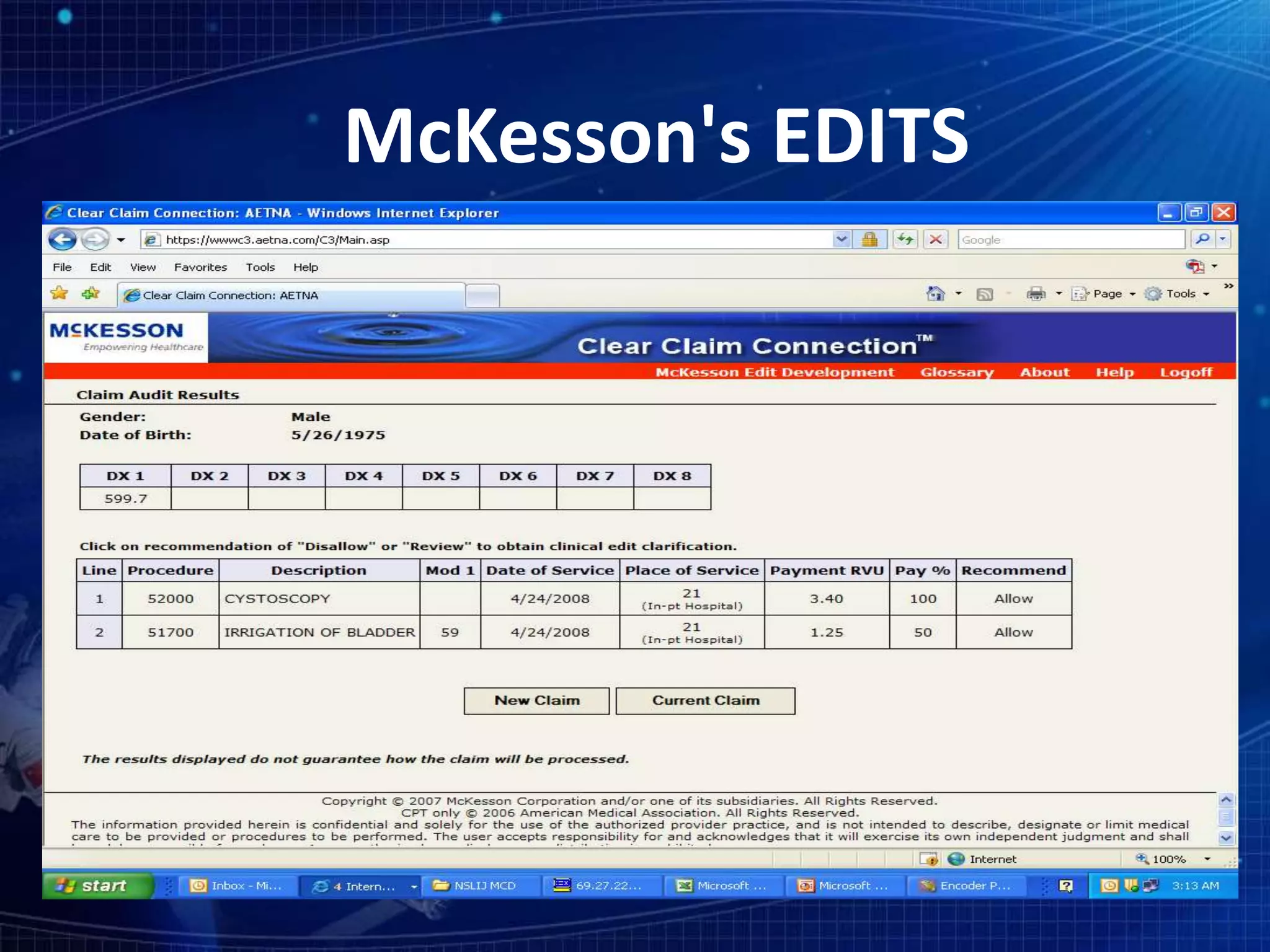
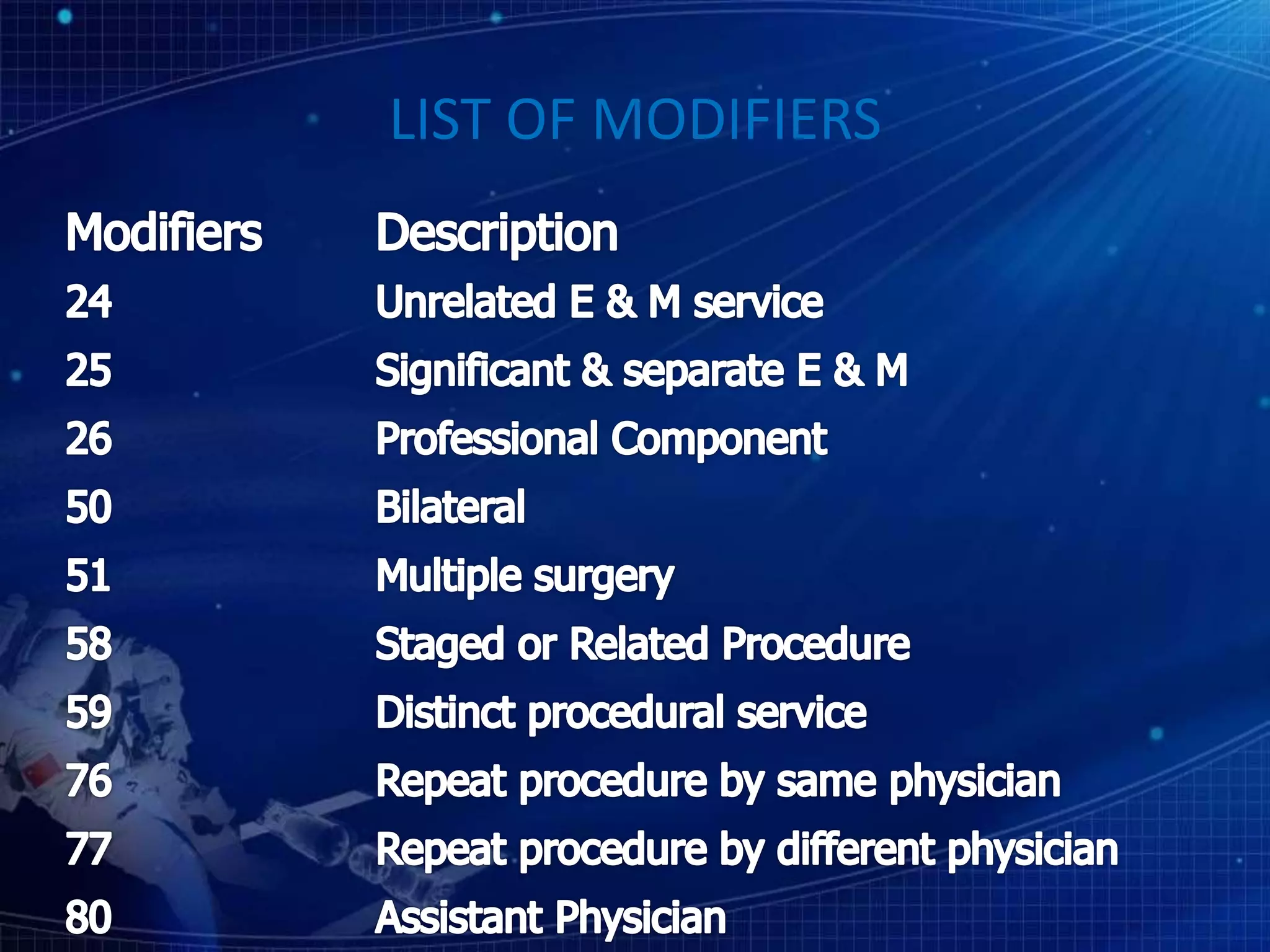
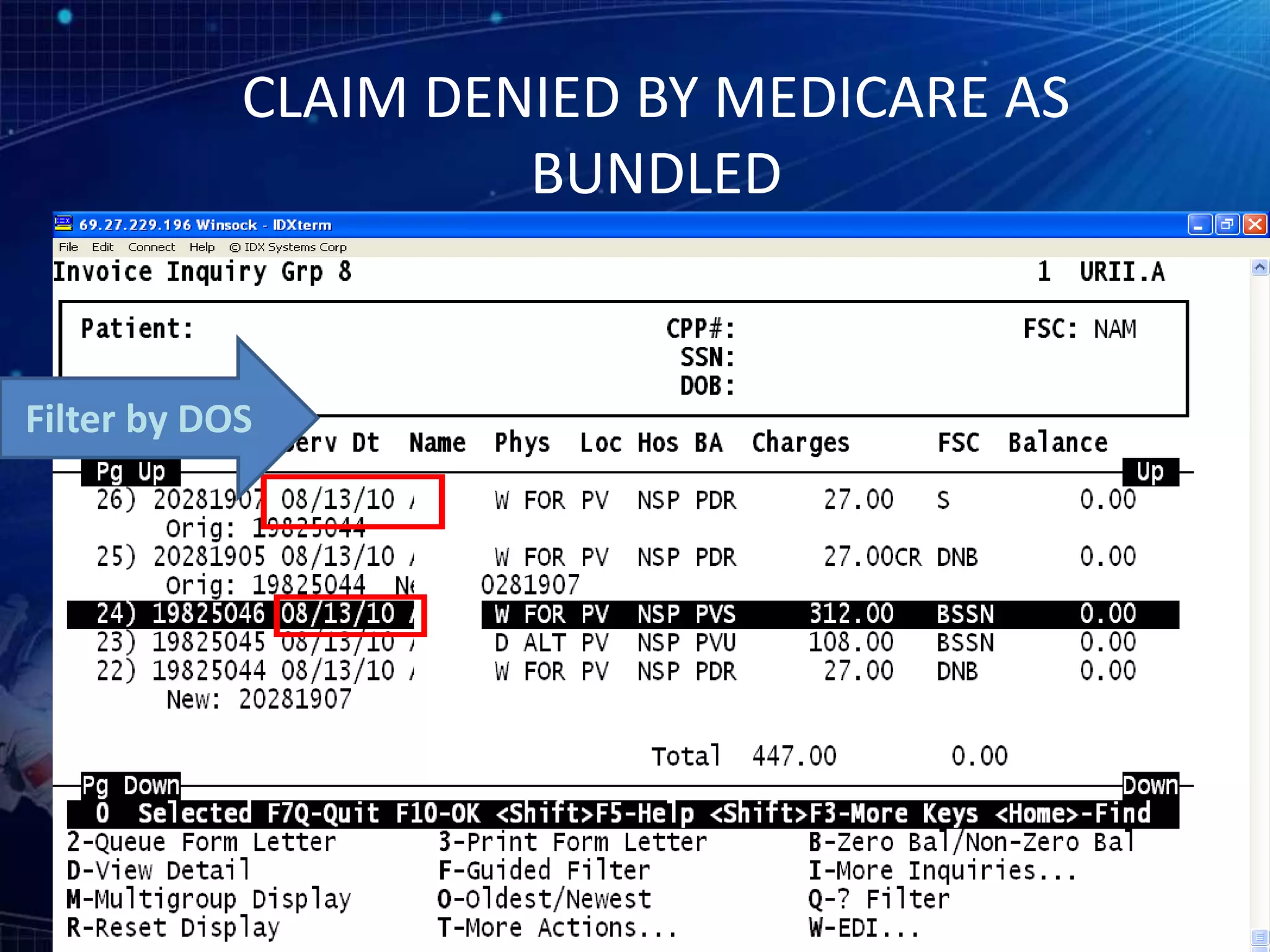
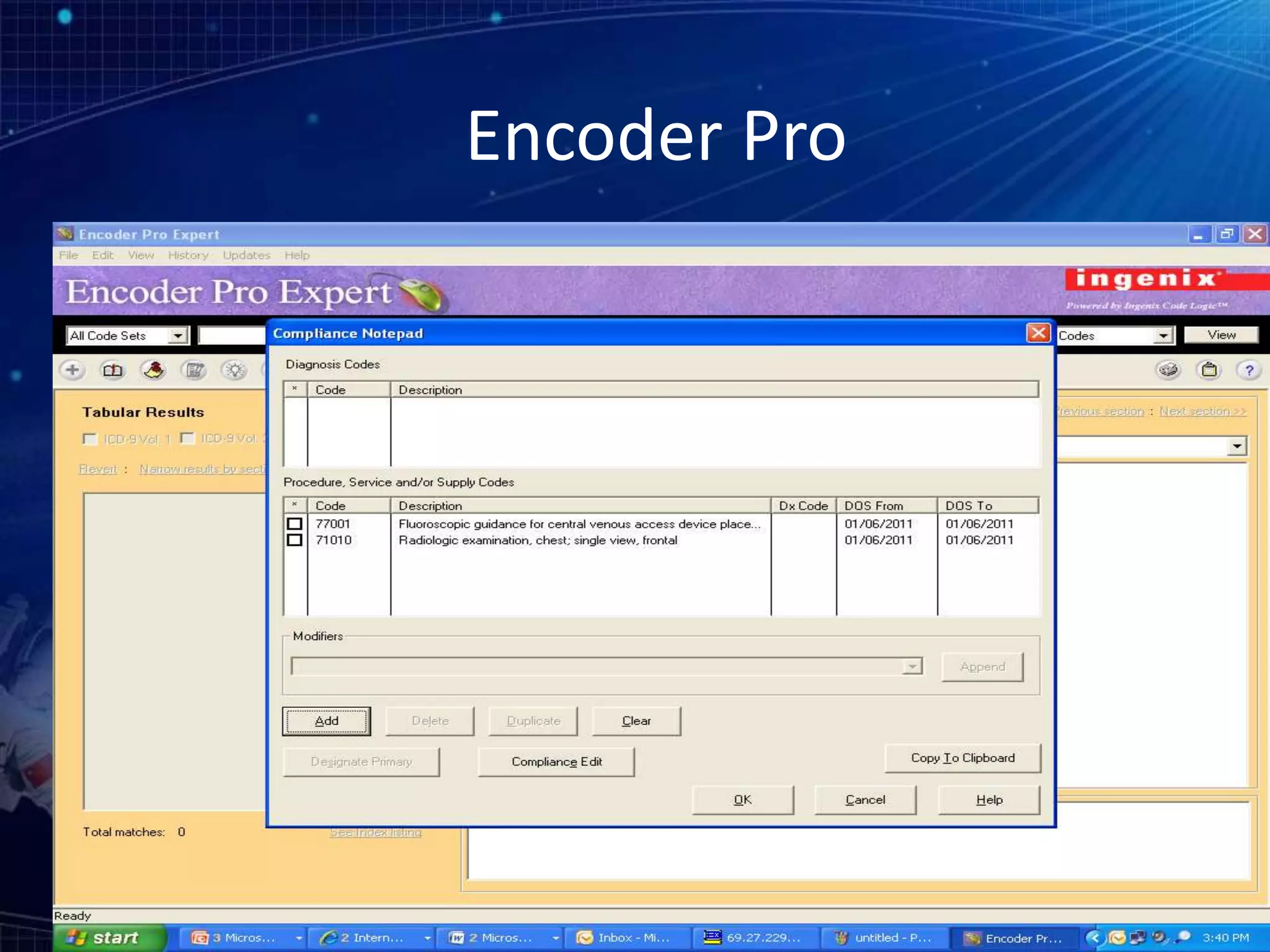
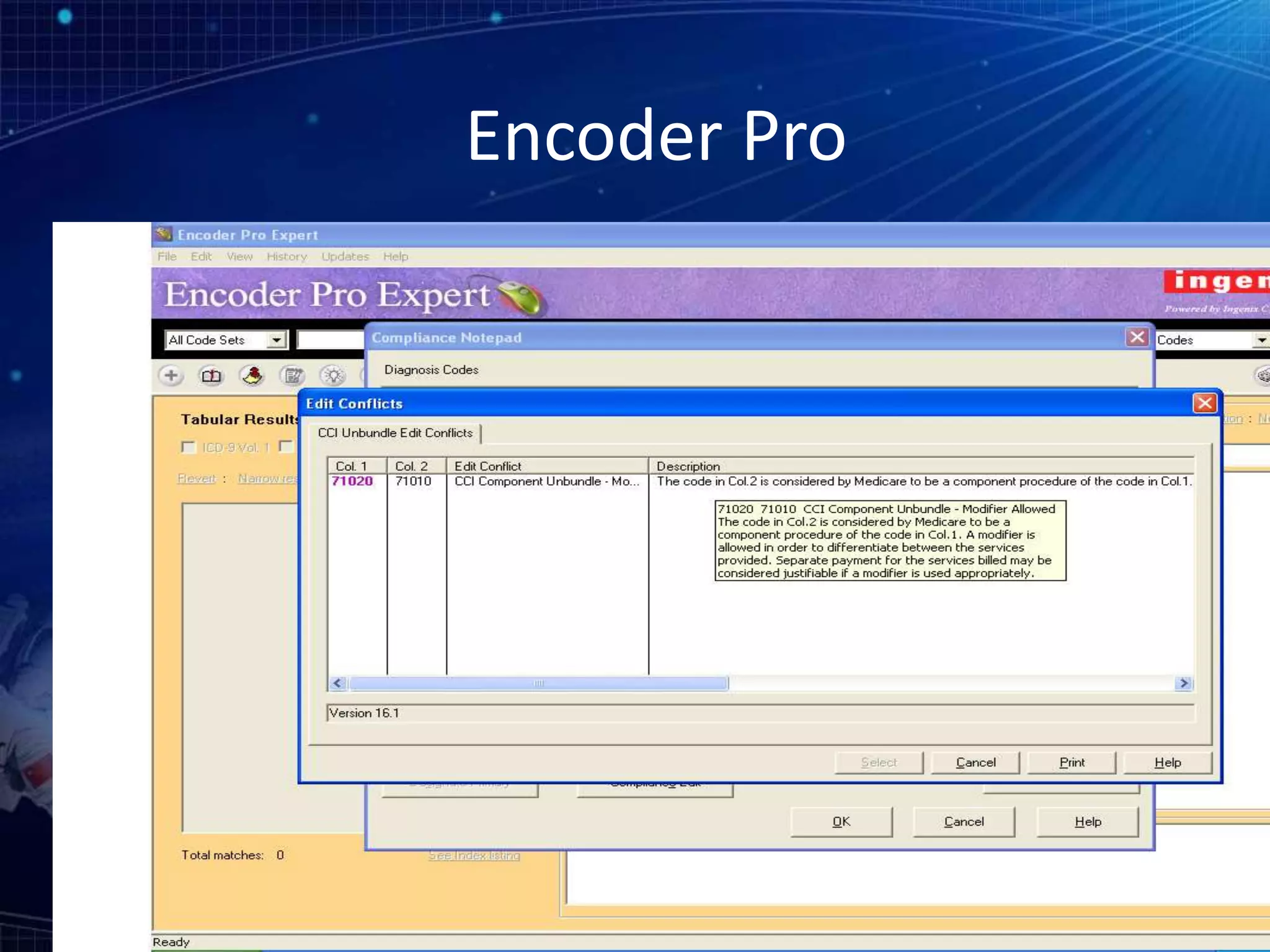
This document discusses various types of denials including inclusive, mutually exclusive, comprehensive and component codes. It provides examples of inclusive coding and defines mutually exclusive procedures that cannot be billed together. It discusses checking CCI edits, commercial websites, and encoder software to determine correct coding. Reasons for denials include missing or incorrect modifiers, downcoding, and billing higher and lower level codes together. Modifiers and their appropriate uses are outlined. Global periods are defined as pre and post-op care periods after a procedure to avoid separate billing.