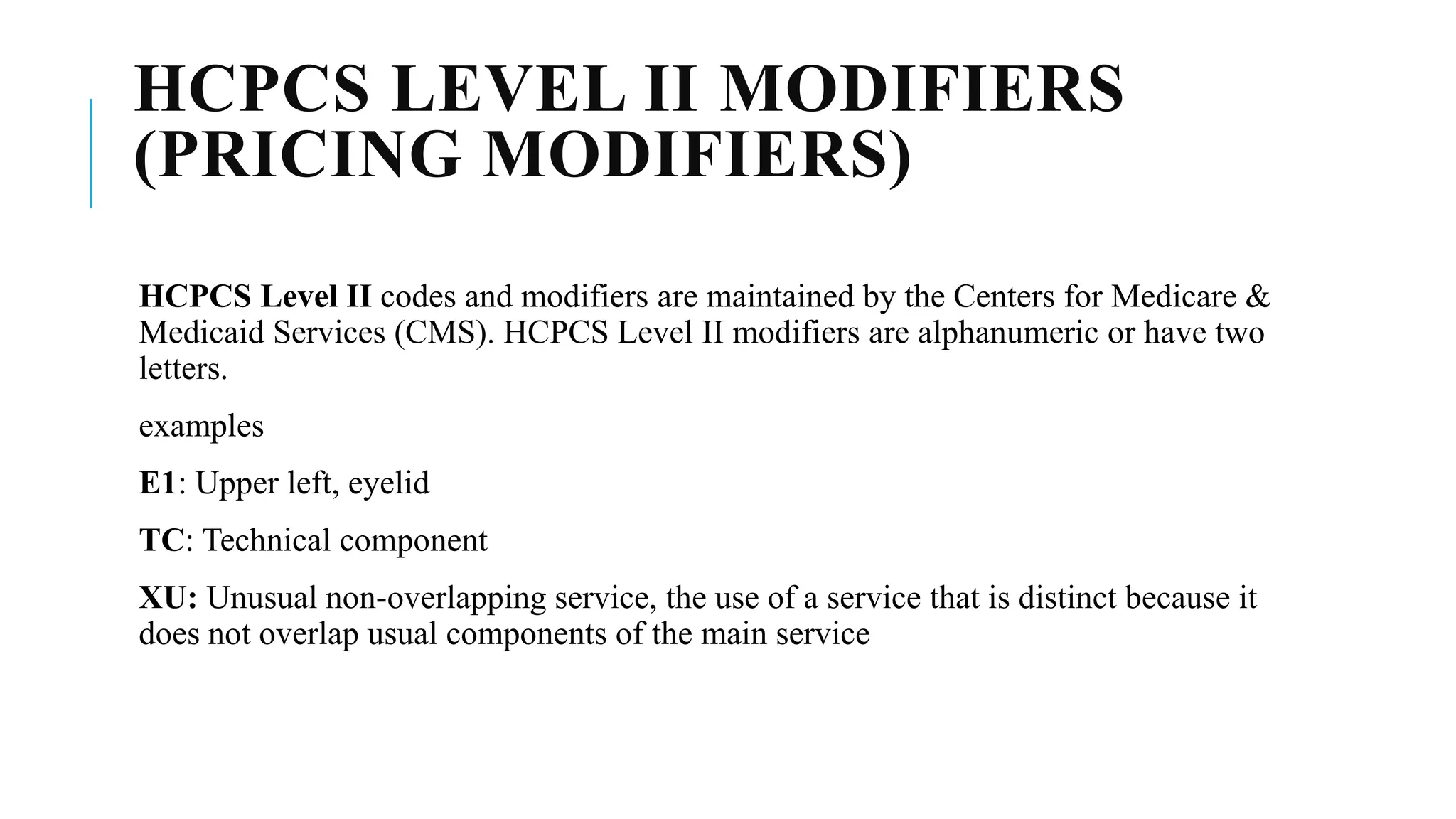
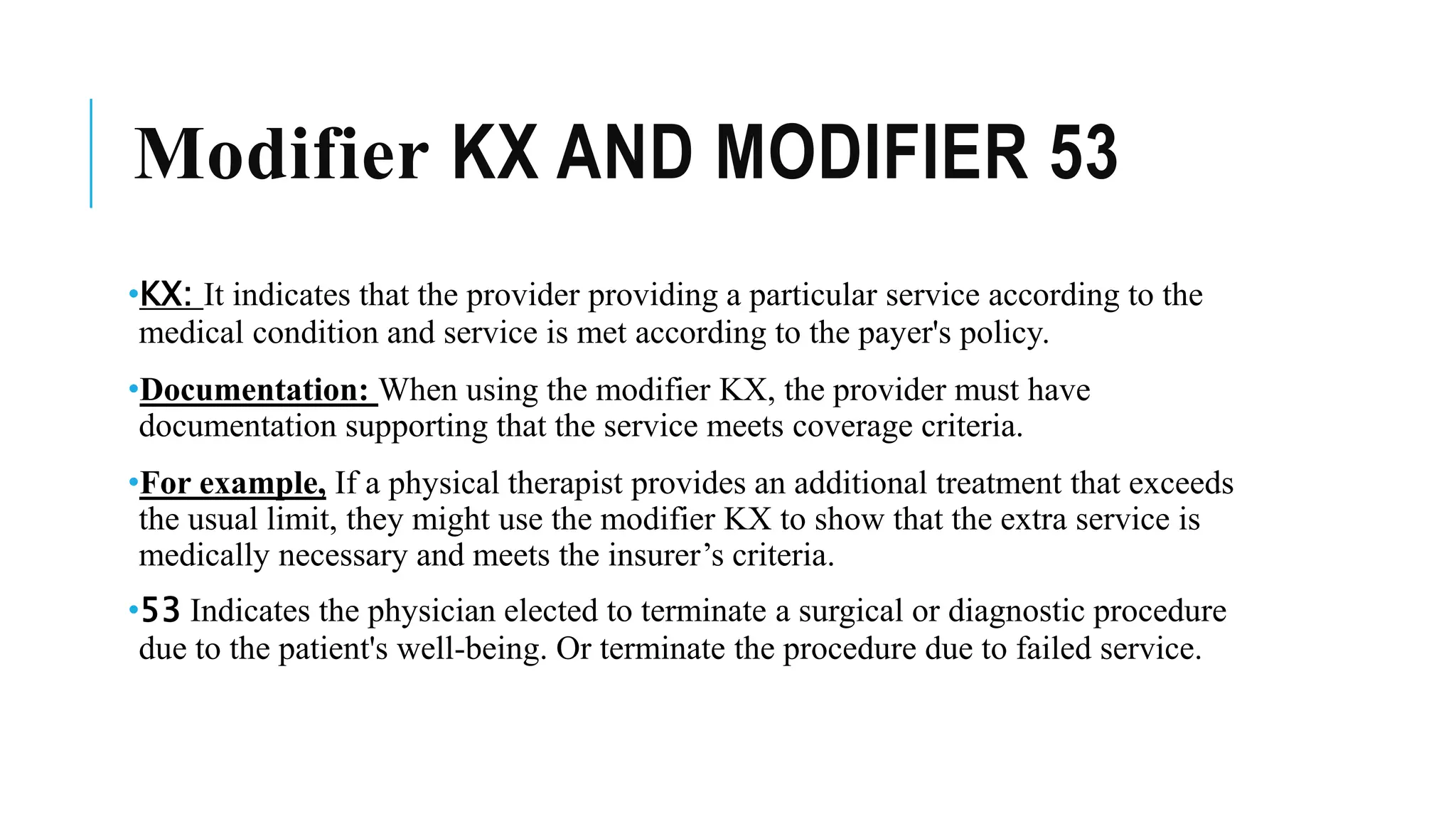
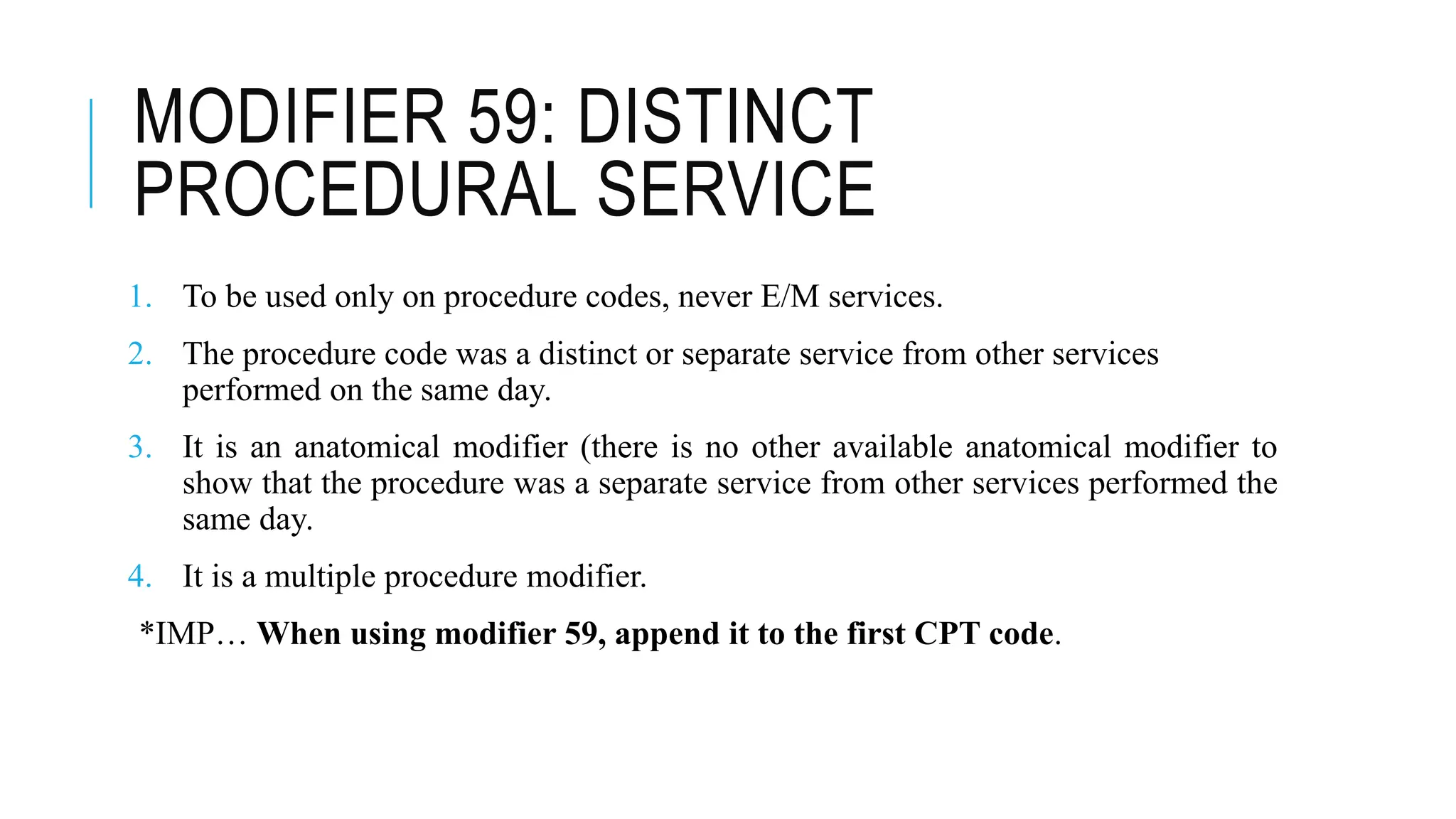
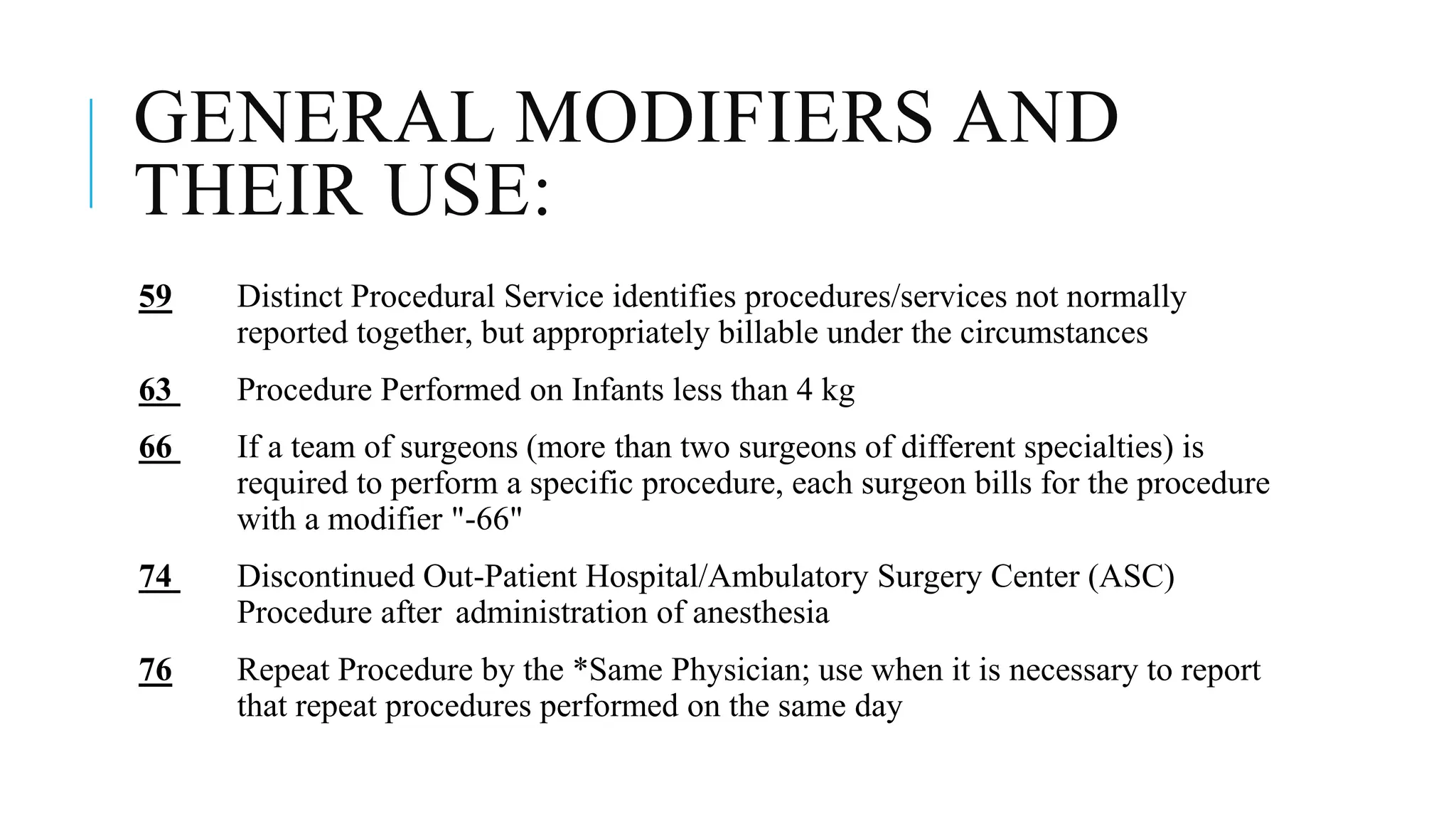
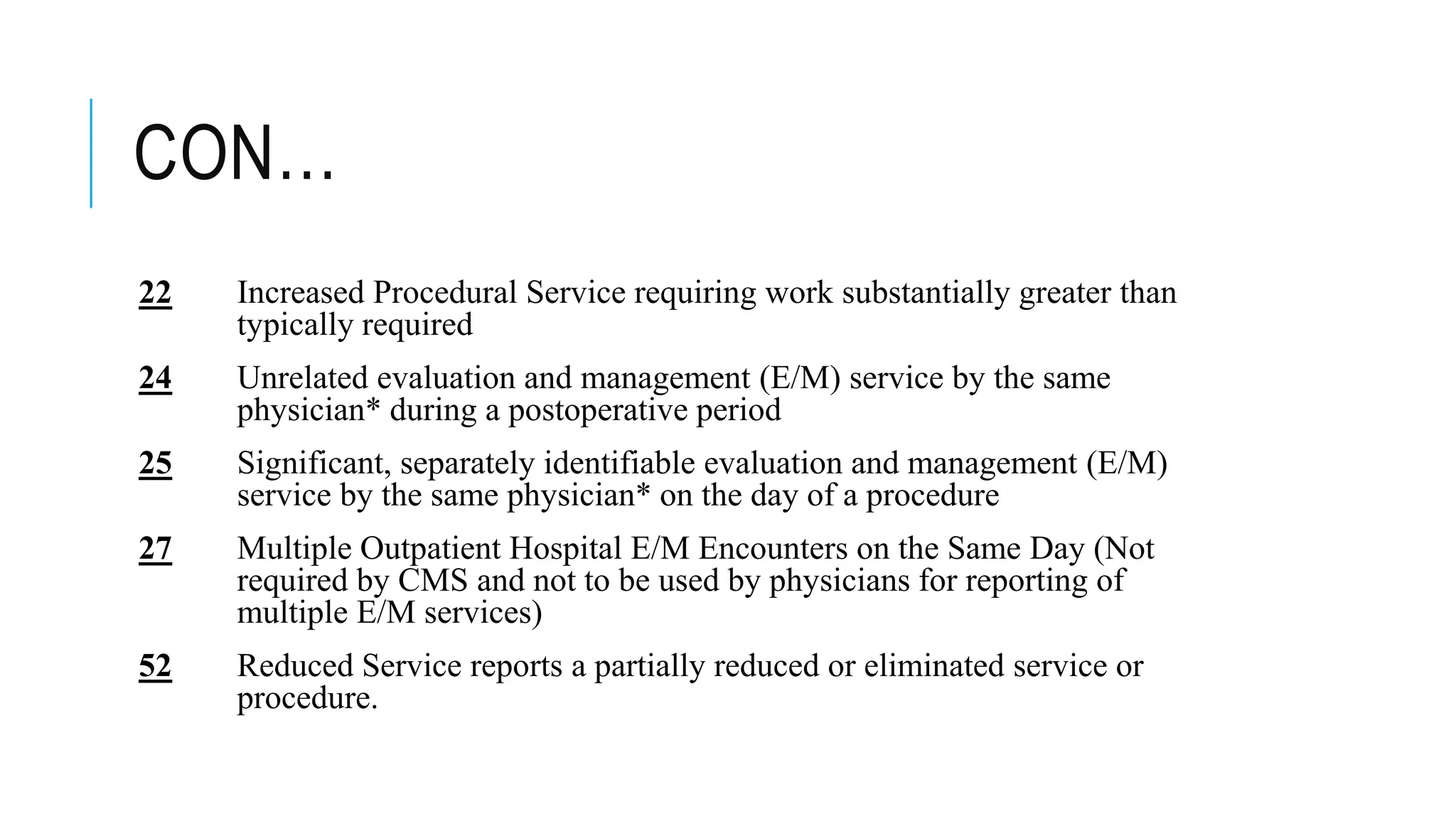
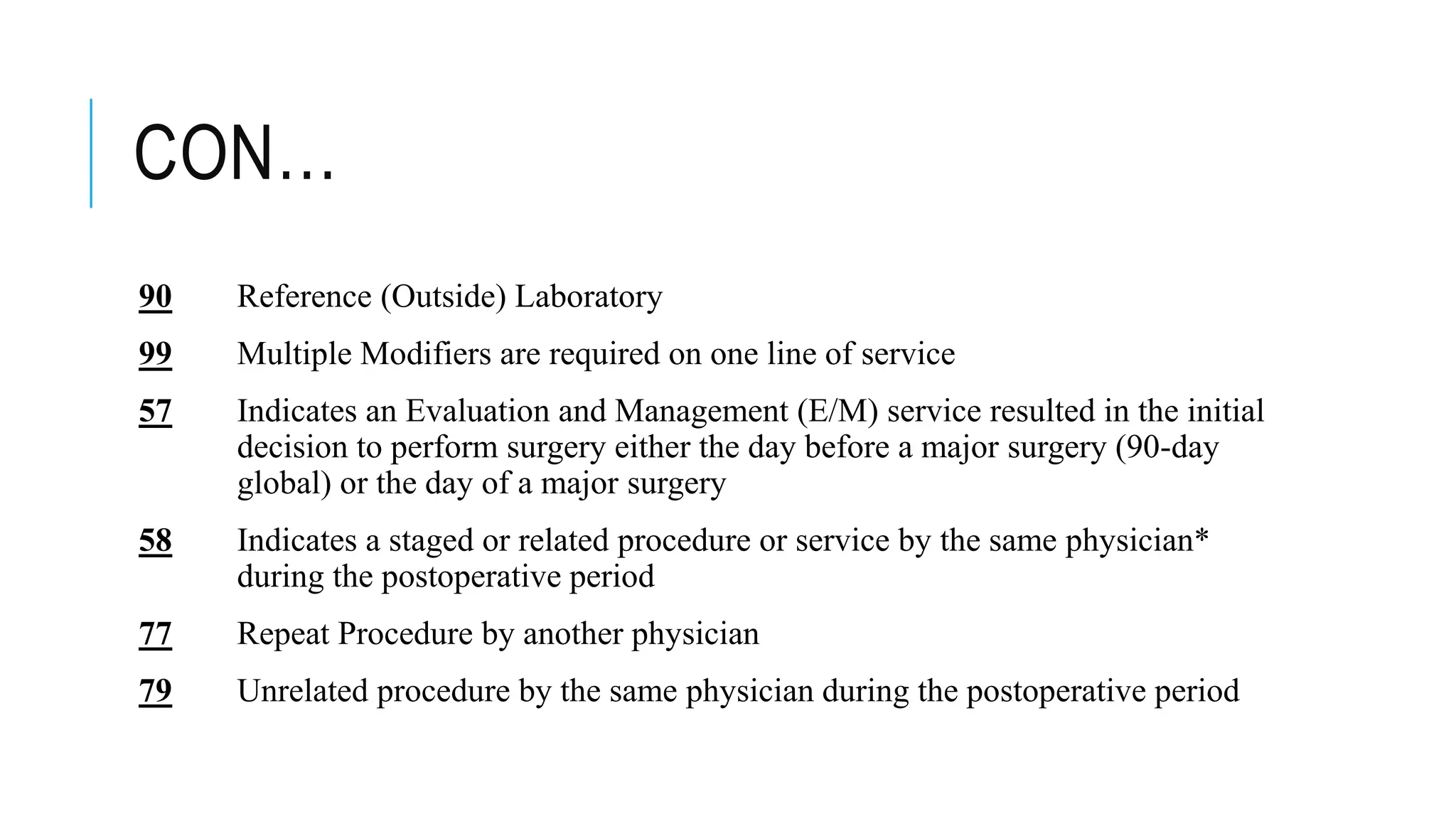
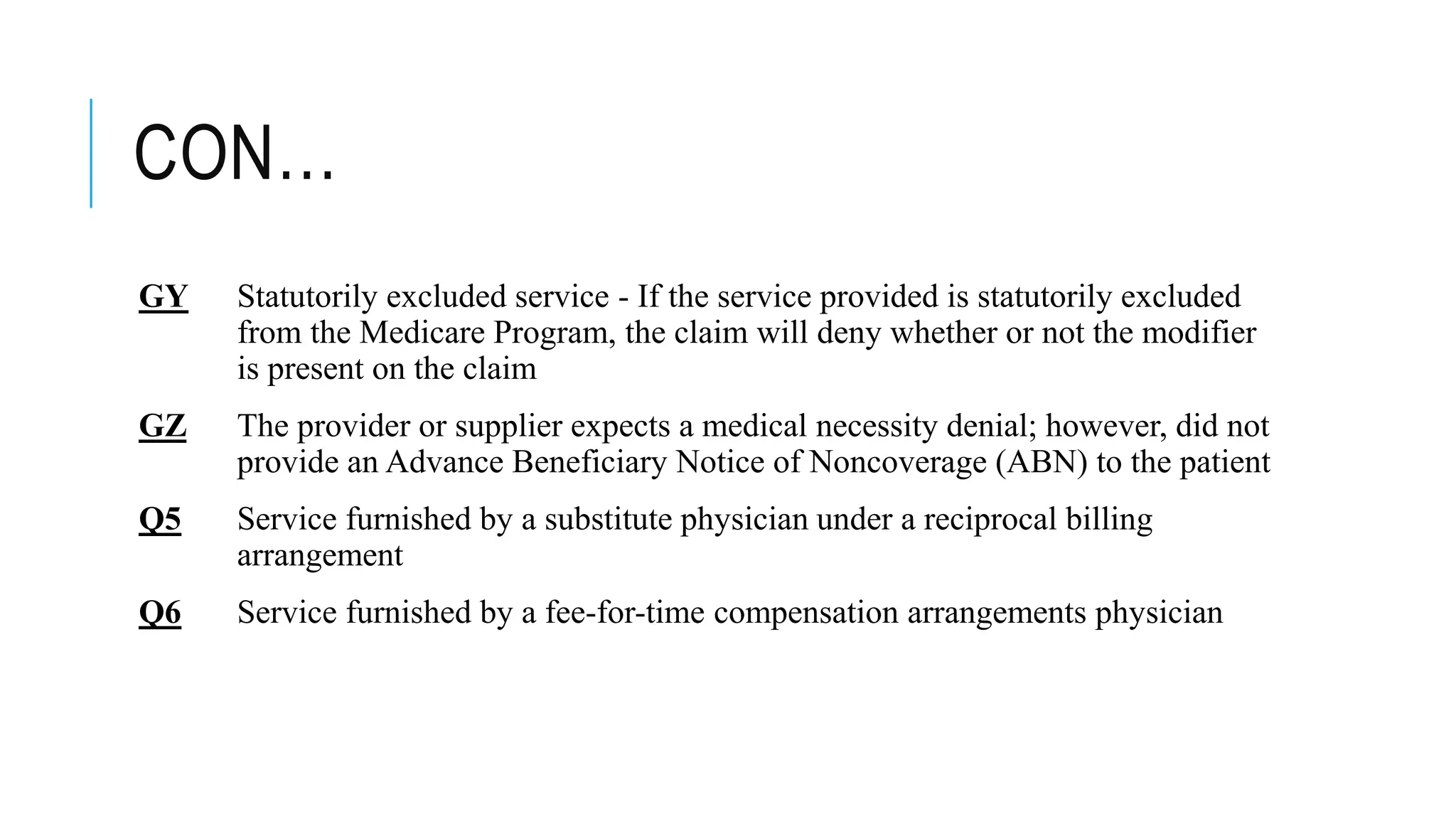
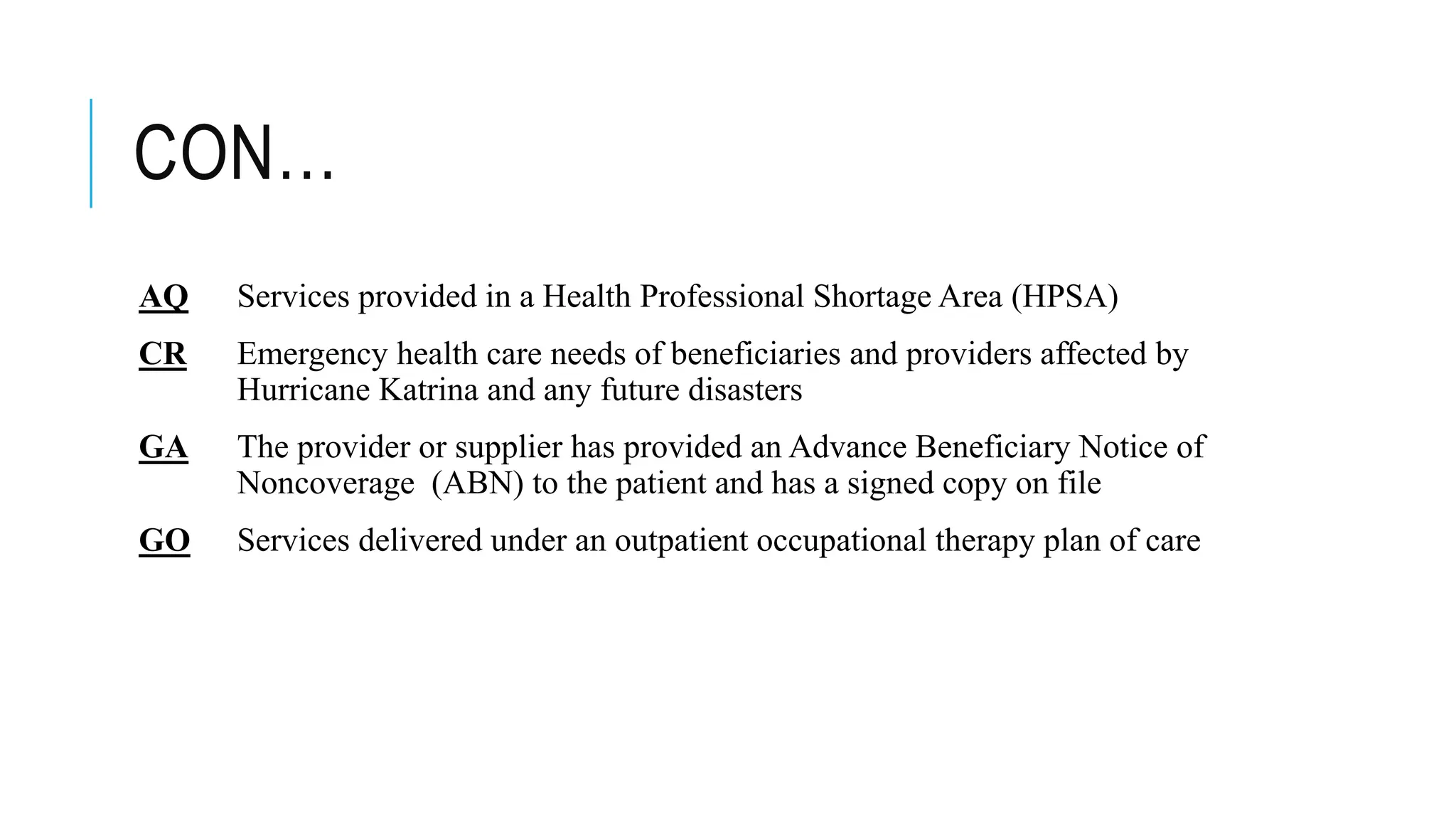
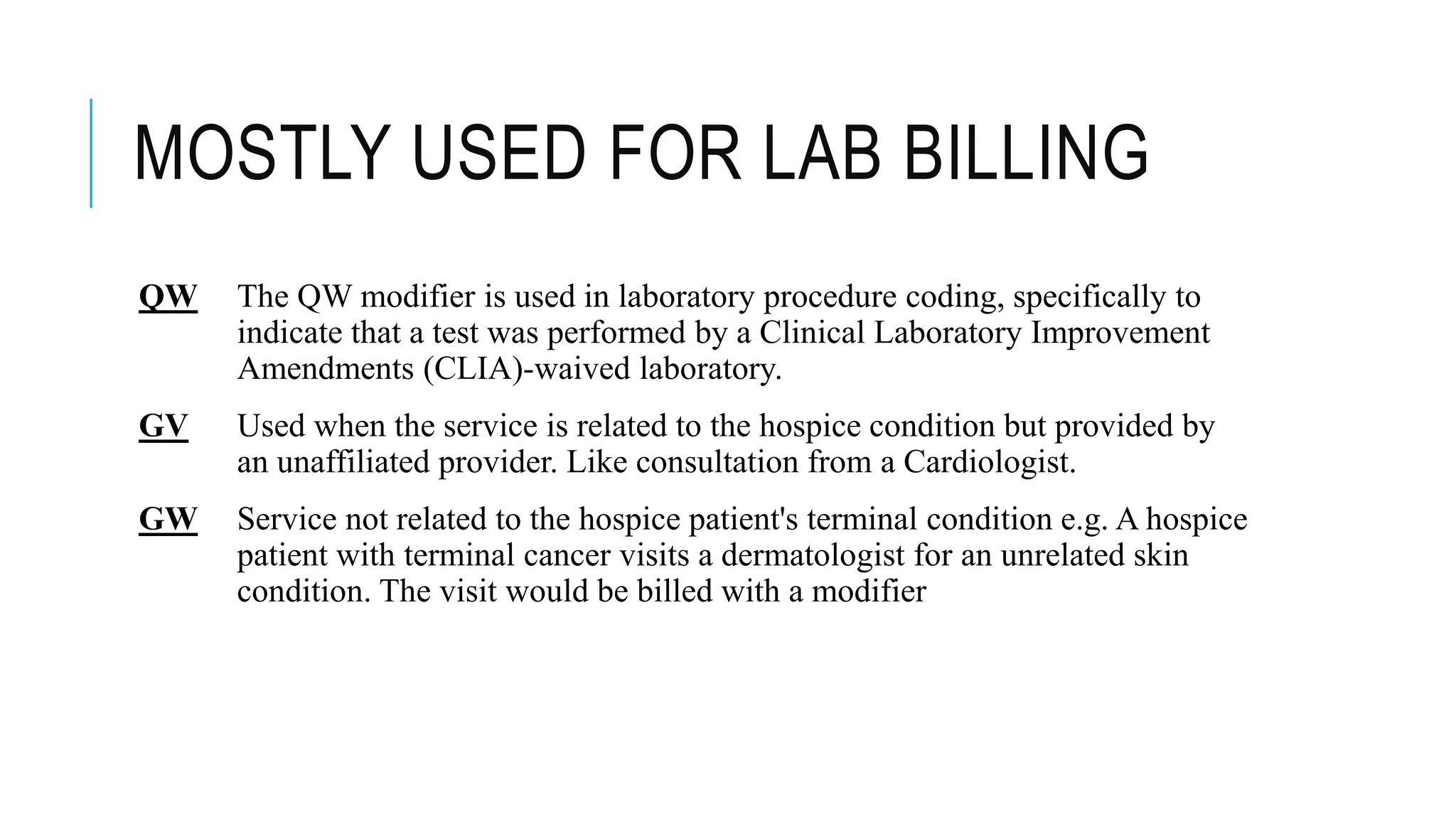
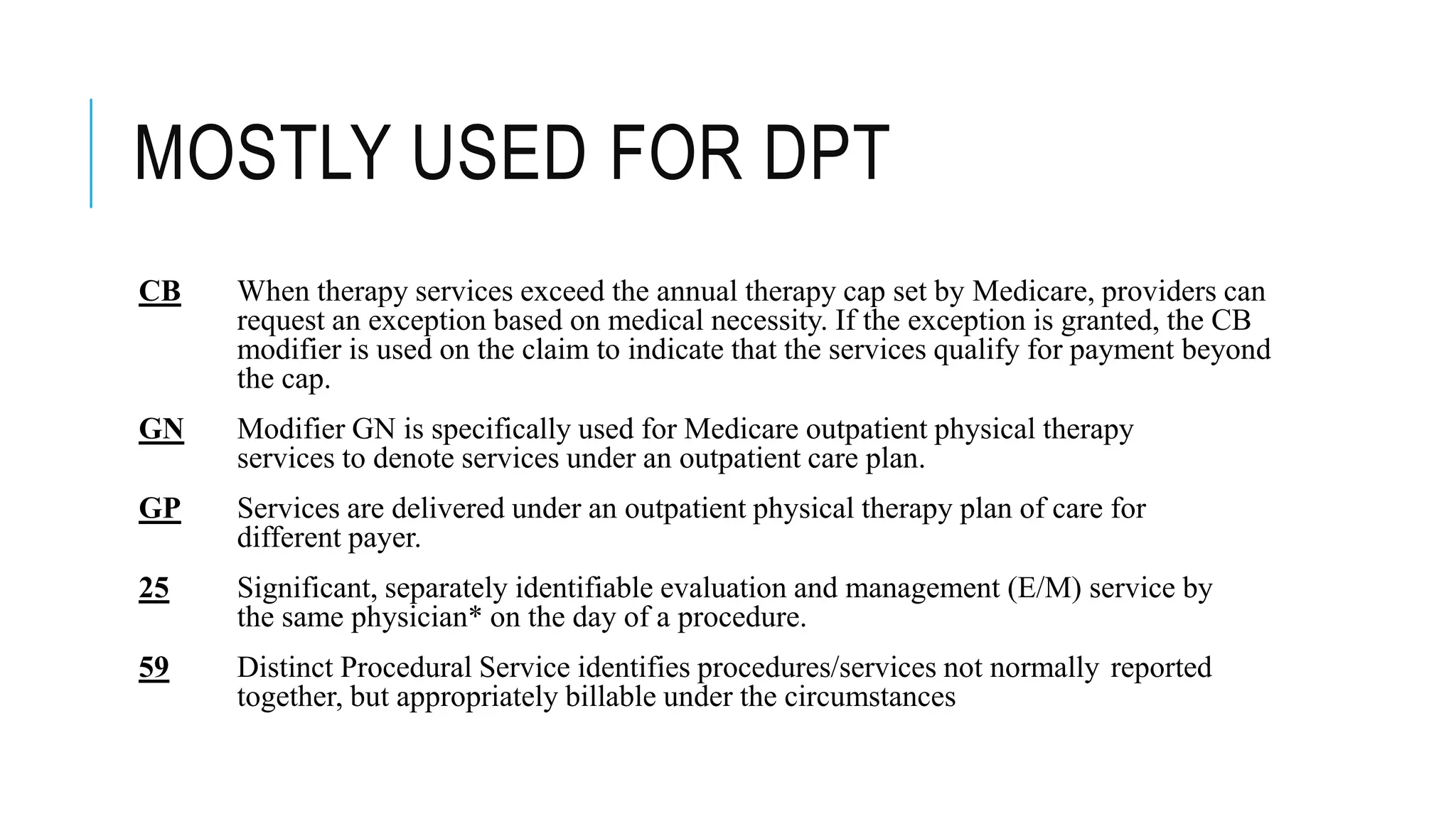
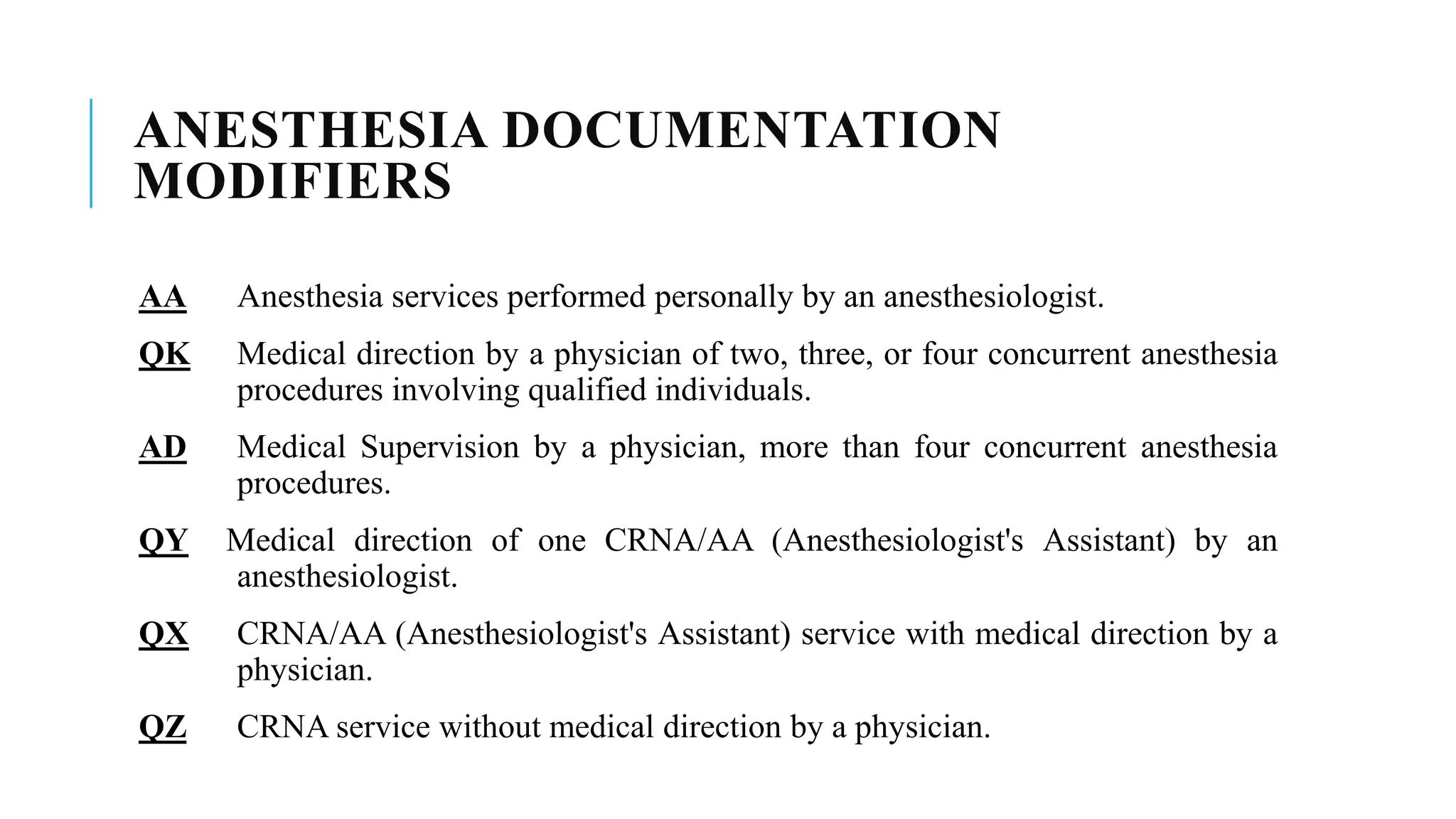
The document provides an overview of medical coding modifiers used in healthcare billing, particularly focusing on CPT and HCPCS Level II modifiers. Modifiers convey additional information about procedures or services without altering the original code's meaning and are essential in various billing scenarios. A wide range of specific modifiers are detailed, each with its distinct application and requirements, including documentation necessary for modifiers like KX and 59.