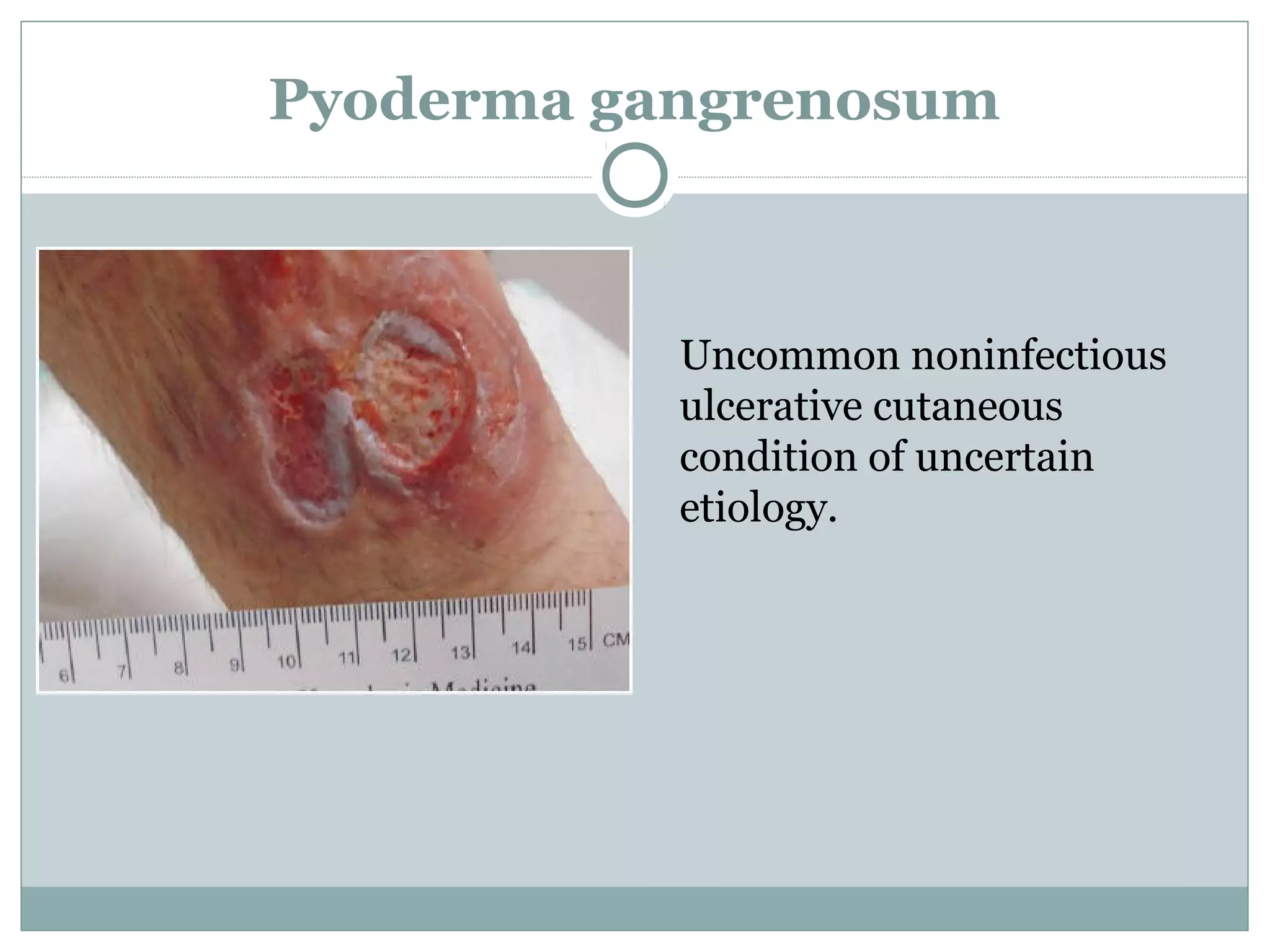
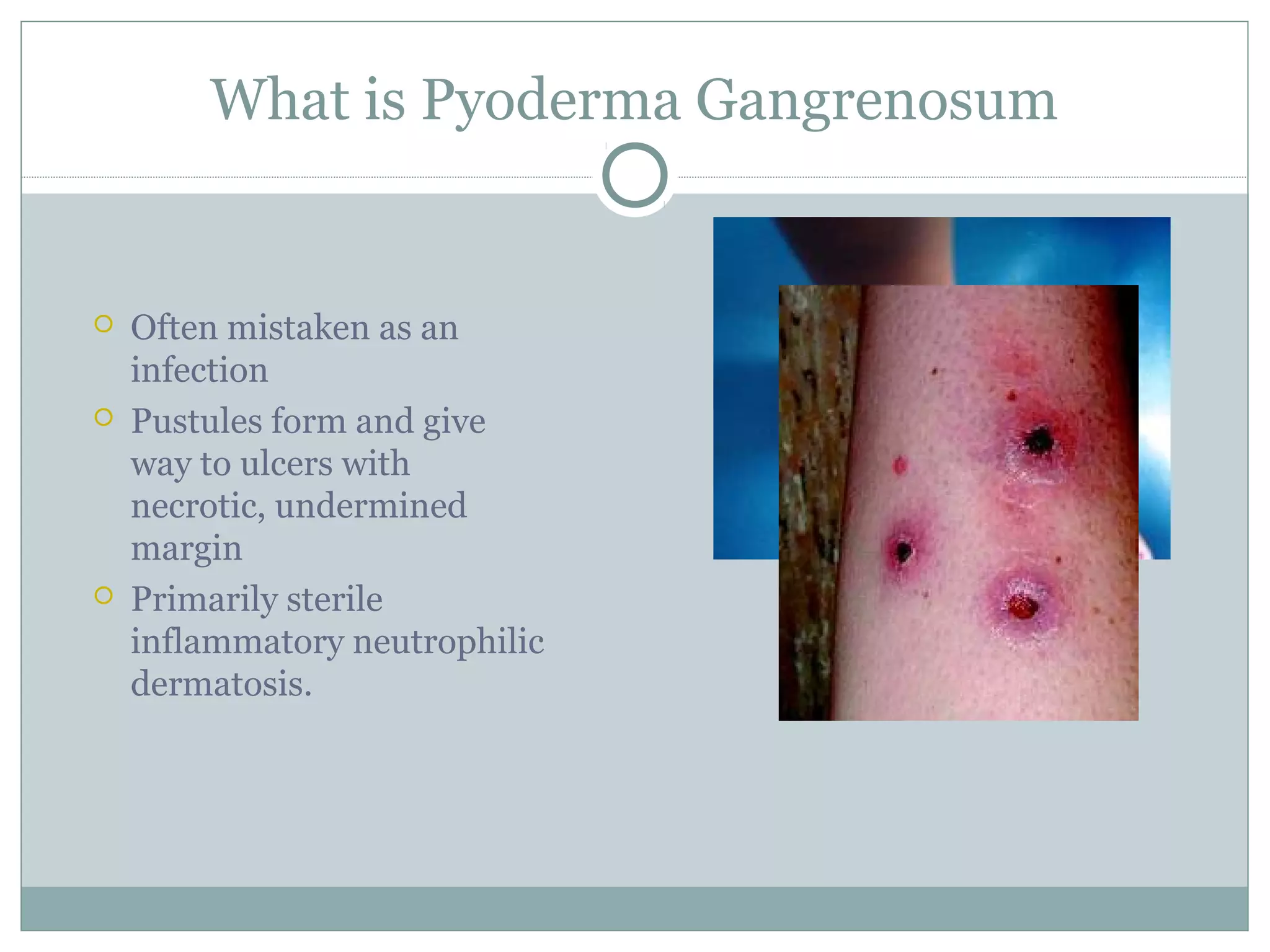
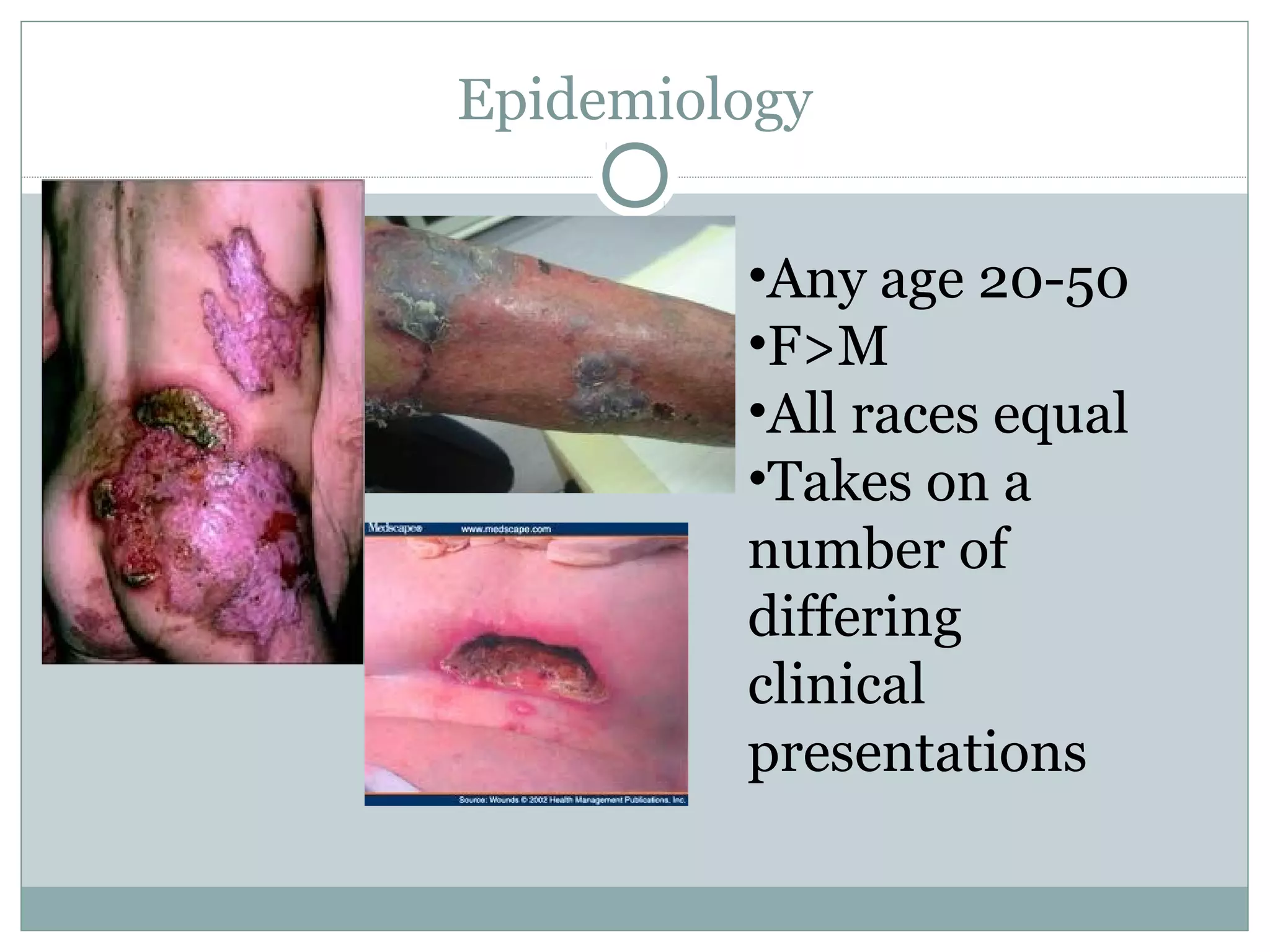
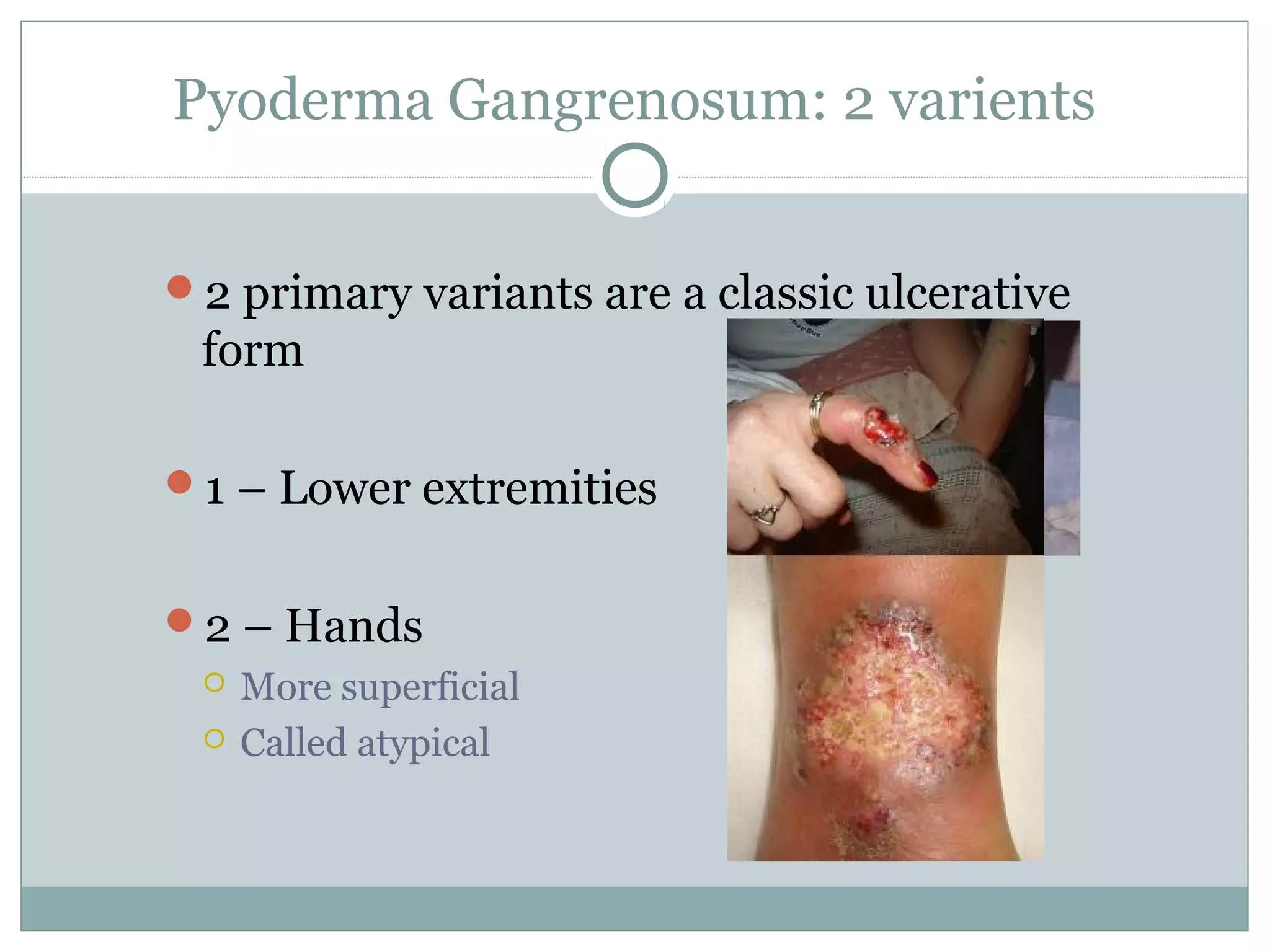
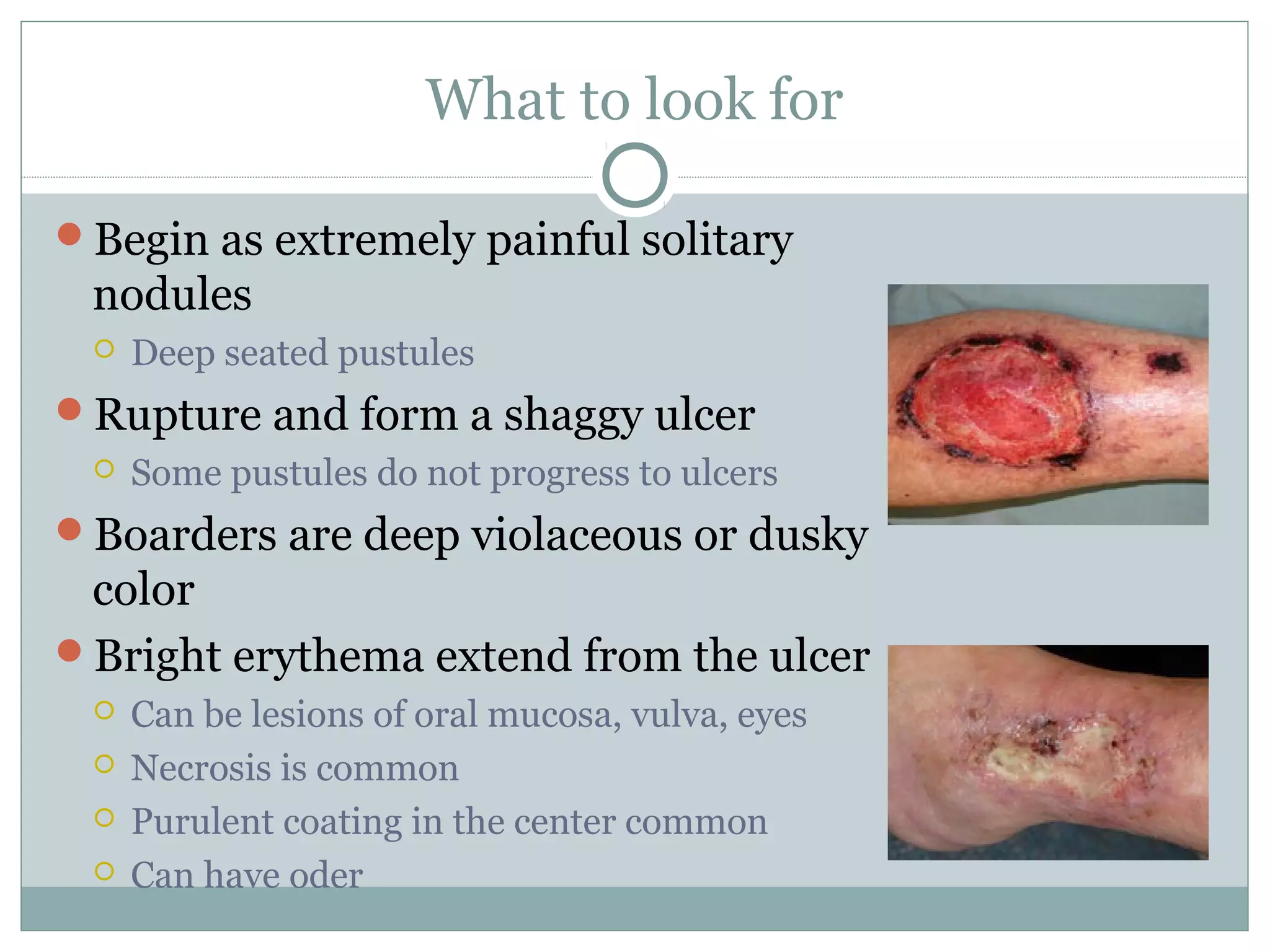
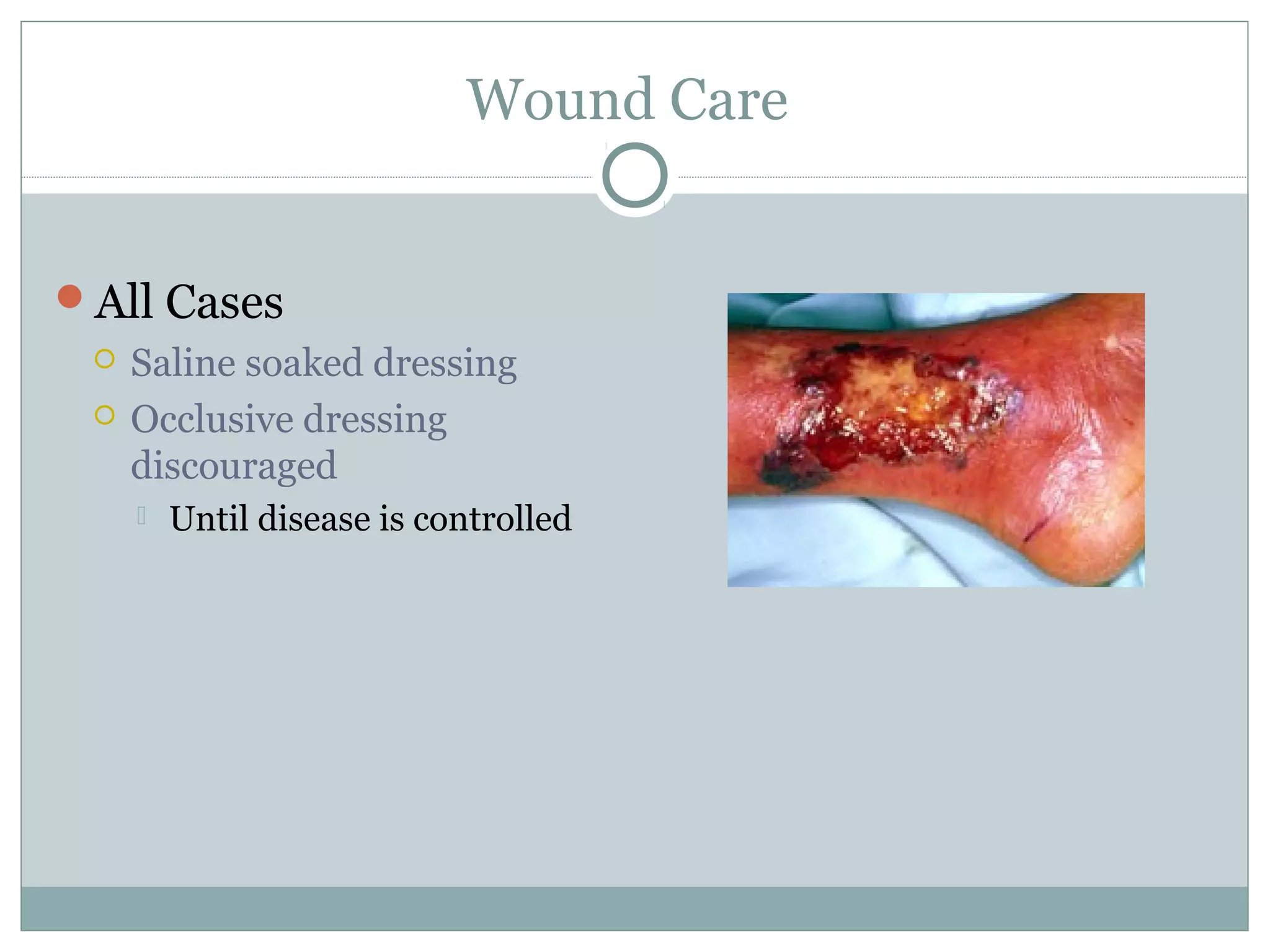
Pyoderma gangrenosum is an uncommon inflammatory skin condition of unknown cause characterized by sterile pustules that form ulcers with necrotic margins. It typically affects adults ages 20-50 and presents as painful lesions that can develop rapidly. While the pathophysiology is poorly understood, it involves dysregulation of the immune system and neutrophils. Treatment involves immunosuppressants like corticosteroids and cyclosporine. Proper diagnosis requires ruling out infection and avoiding biopsy or surgery, as trauma can worsen lesions.