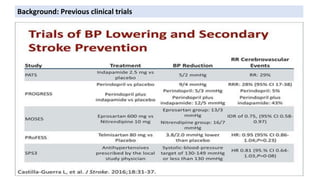
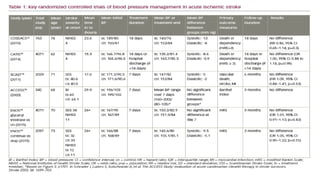
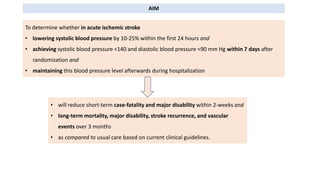
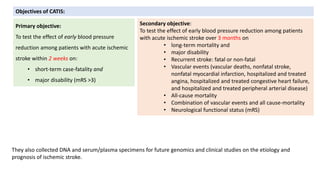
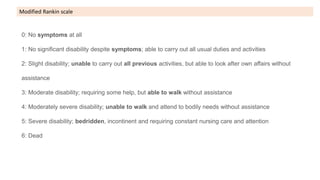
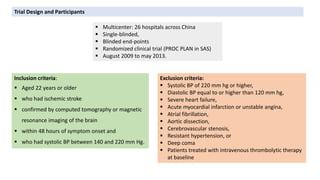
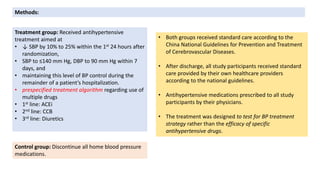
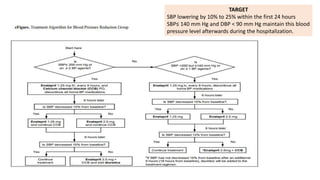
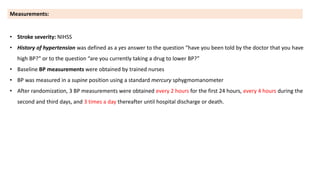
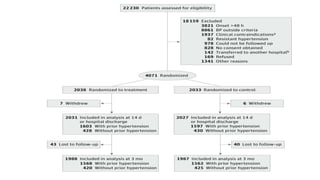
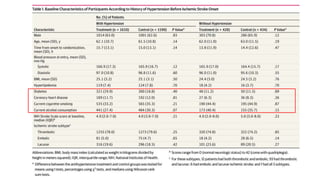
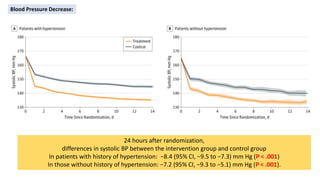
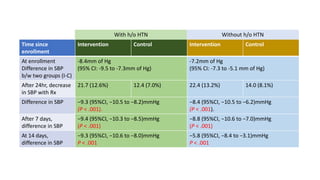
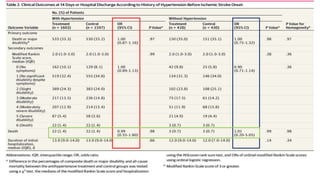
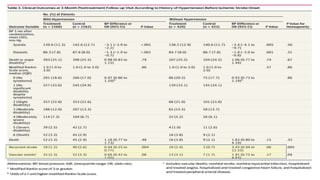
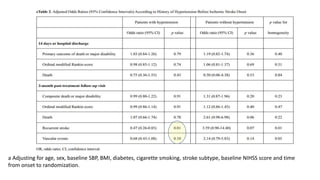
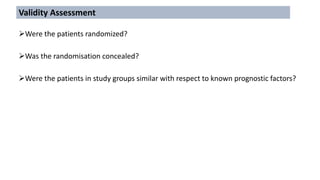
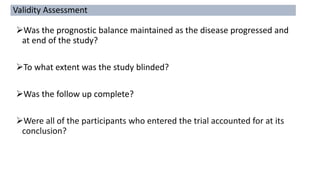
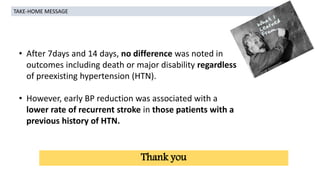
This study aimed to determine if early antihypertensive therapy in patients with acute ischemic stroke leads to different outcomes in those with and without a history of hypertension. Over 4 years, 4,071 patients were randomly assigned to either strict blood pressure control or usual care. Strict control led to greater reductions in blood pressure over 24 hours, 7 days and 14 days, with no differences in short-term death or disability regardless of hypertension history. However, early blood pressure reduction was associated with a lower rate of recurrent stroke in patients with a history of hypertension.