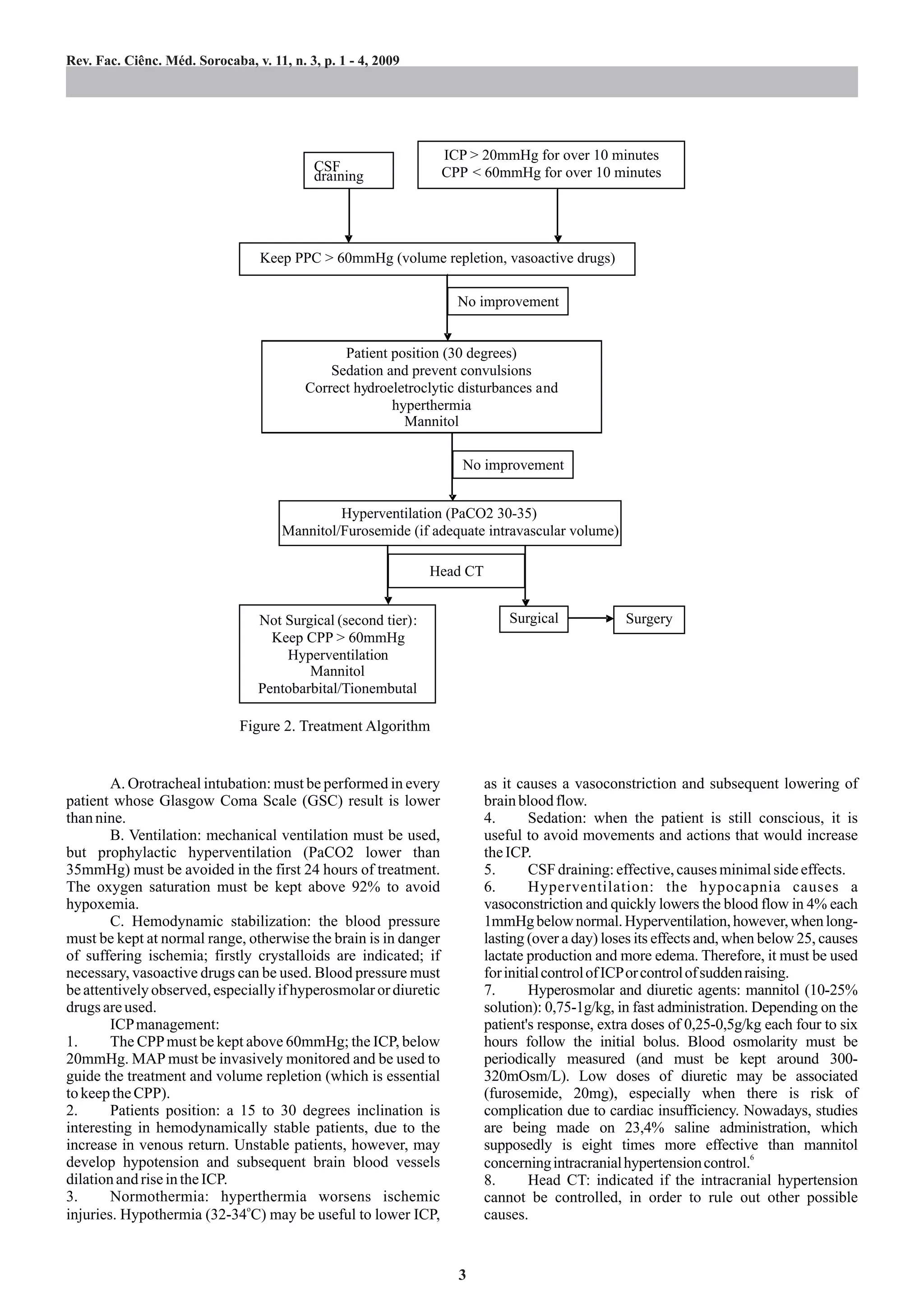
This document discusses the management of intracranial hypertension, highlighting its prevalence in emergency settings and the necessity to prevent secondary brain damage. It outlines the importance of monitoring intracranial pressure (ICP), various treatment protocols including the use of mannitol, and the significance of advanced life support measures. The document also addresses the complexities of diagnosing and treating this condition, emphasizing the need for careful management to mitigate risks such as ischemia and increased intracranial pressure.

![Revista da Faculdade de Ciências Médicas de Sorocaba
Second tier: unconventional maneuvers to refractory 2. Ferraz FAP, Braga FM. Hipertensão intracraniana: tumores
intracranial hypertension, includes: encefálicos. In: Prado FC, Ramos J, Valle JR. Atualização
1. Barbiturates: halves brain activity and neuronal energy Terapêutica. 23ª ed. São Paulo: Artes Médicas; 2007. p.
consumption, thus, lowering the ICP. Nevertheless, barbiturate 1042-3.
3. CarlottiI JR CG, ColliI BO, Dias LAA. Hipertensão
cause systemic vasodilatation, miocardic depression, arterial intracraniana. Medicina. (Ribeirão Preto) 1998; 31:552-62.
hypotension and pulmonary secretions accumulations. And, as 4. Allam G. Aumento da pressão Intracraniana e herniação
the brain blood flow lowers, encephalic ischemia may develop. cerebral. In: Jones HRJ. Neurologia de Netter. Porto Alegre:
Pentobarbital: attack dose: 3-10mg/kg (30 infusion), followed Artmed; 2006. p. 335-43.
by 5mg/kg/h for three hours. The maintenance dose shall be 5. Giugno KM, Maia TR, Kunrath CL, Bizzi JJ. Treatment of
adjusted in order to prevent suppressions in the EEG. intracranial hypertension. J Pediatr. (Rio de Janeiro) 2003;
2. Decompressive craniectomy: reserved for the surgical 79(4):287-96.
and the most refractory cases; its results being better as soon as it 6. Suarez JI, Qureshi AI, Bhardwaj A. Treatment of refractory
intracranial hypertension with 23,4% saline. Crit Care Med.
is performed,4,7-9 and most survivors develop severe sequelae,
1998; 26(6):1118-22.
especially those older than 45. Better results come out in 7. Faleiro RM, Pimenta JG, Faleiro LCM, Cordeiro AF, Maciel
younger patients; on the other hand, older patients usually CJ, Gusmão SNS. [Decompressive craniotomy for the early
present co-morbidities that may worsen the prognosis. treatment of traumatic intracranial hypertension]. Arq
Subdural collections, hydrocephaly, convulsions and infections Neuropsiquiatr. 2005; 63(2B):508-13.
are some of the complications that might occur. 8. Faleiro RM, Faleiro LCM, Oliveira MM, Silva T, Caetano EC,
Gomide I, et al. [Decompressive craniectomy in children and
adolescents with head injury: analysis of seven cases]. Arq
REFERENCES Neuropsiquiatr. 2006; 64(3B):839-44.
9. Nobre MC, Monteiro M, de Albuquerque AC, Veloso AT,
1. Machado FS, Joaquim MAS, Capone NetoA. Monitorização e Mendes VA, Silveira MF, et al. [Decompressive craniectomy
manuseio da hipertensão intracraniana, in: Schettino G, for treatment of intracranial hypertension secondary to large
Cardoso LF, Mattar Júnior J, Torggler Filho F. Paciente crítico ischemic cerebral infarction: analysis of 34 cases]. Arq
diagnóstico e tratamento. São Paulo: Manole; 2006. Neuropsiquiatr. 2007; 65(1):107-13.
REVISTA DA FACULDADE DE CIÊNCIAS MÉDICAS DE SOROCABA
Agradecemos a colaboração da Associação dos Docentes da PUC-SP
Diretoria
Enio Marcio Maia Guerra
João Luiz Garcia Duarte
Celeste Gomes Sardinha Oshiro
José Eduardo Martinez
Dirce Setsuko Tacahashi
Nelson Boccato Jr.
4](https://image.slidesharecdn.com/intracranialhypertensionmanagement-rfcms-100404202054-phpapp01/75/Intracranial-Hypertension-Management-4-2048.jpg)