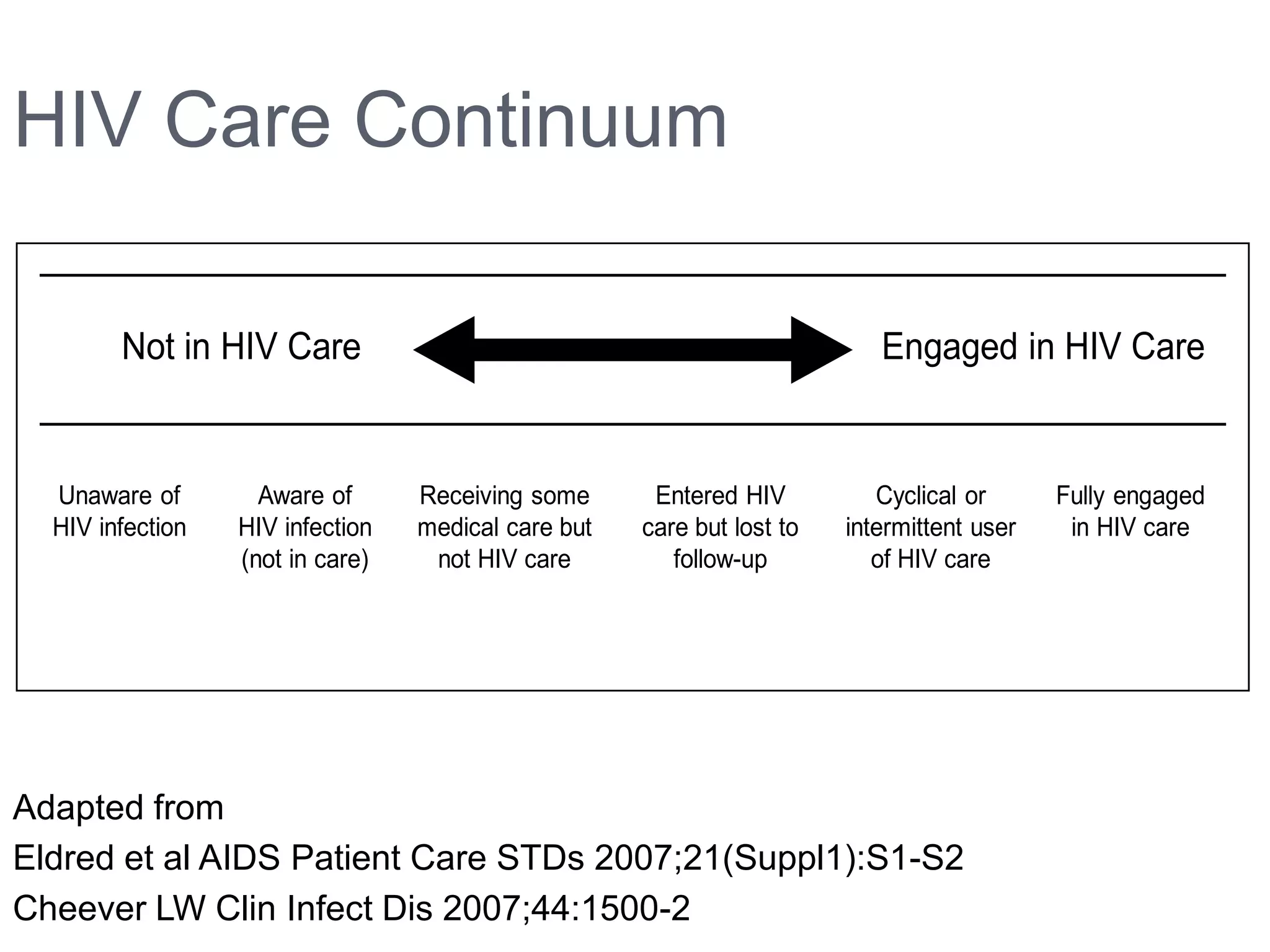
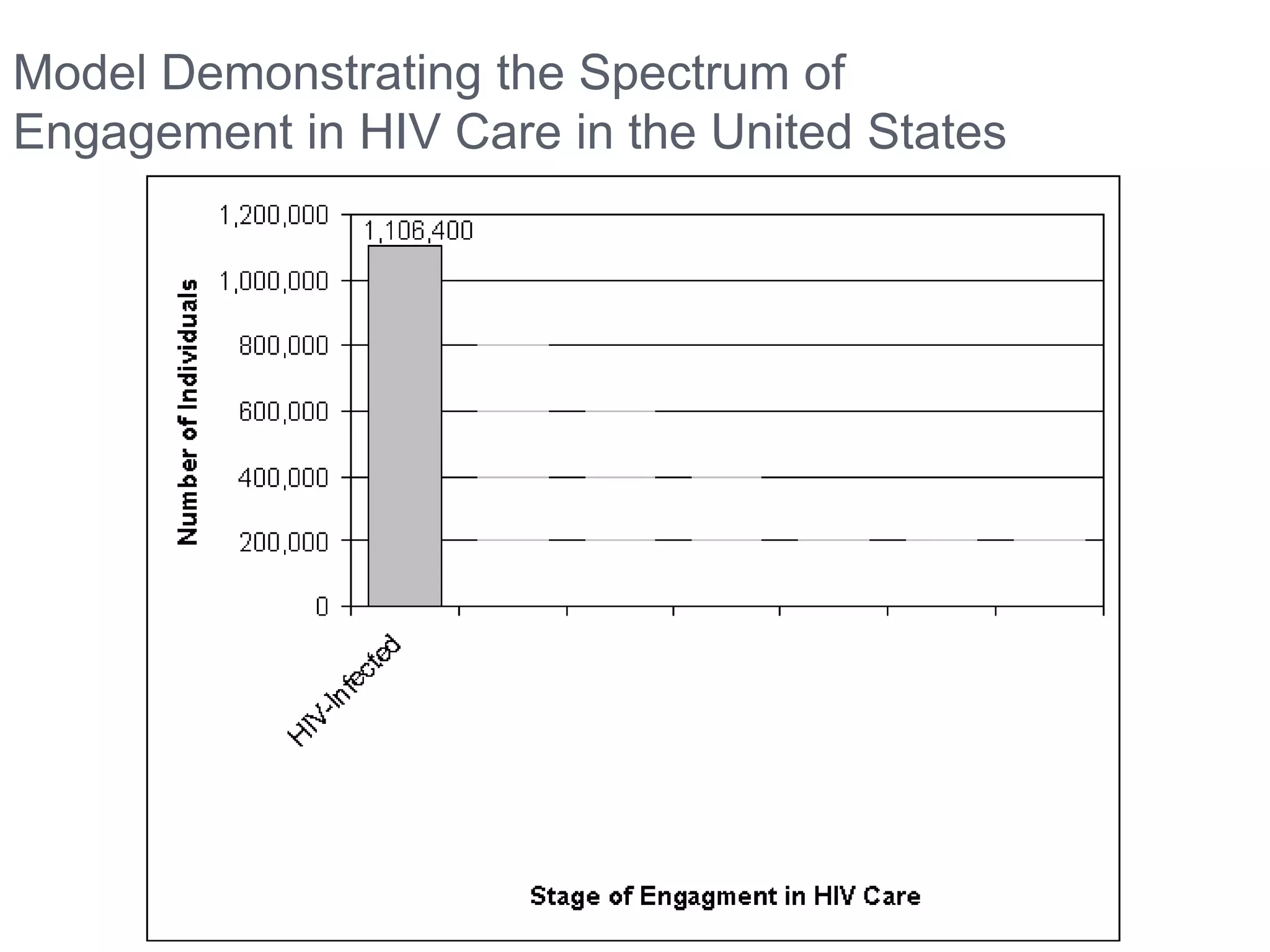
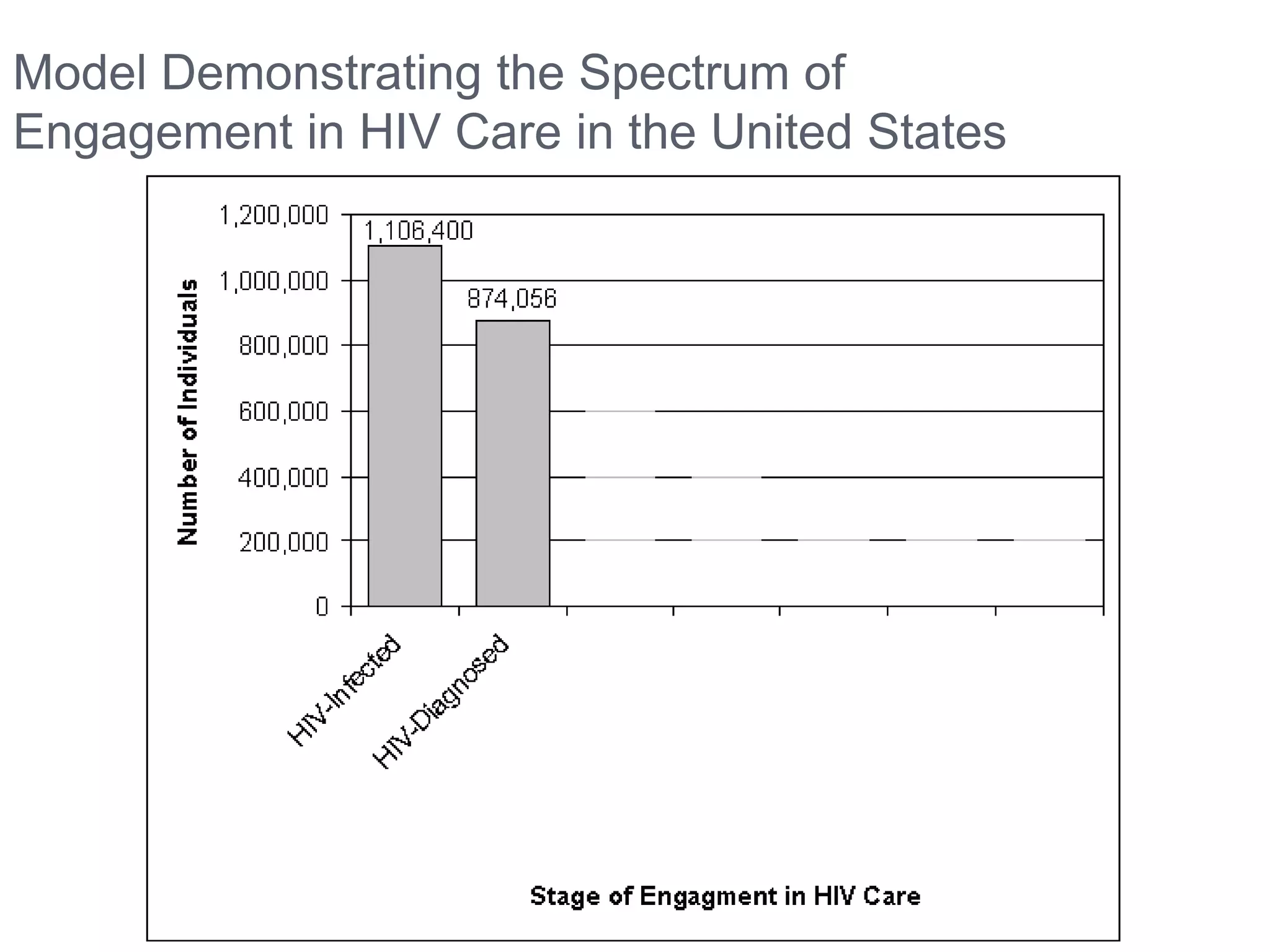
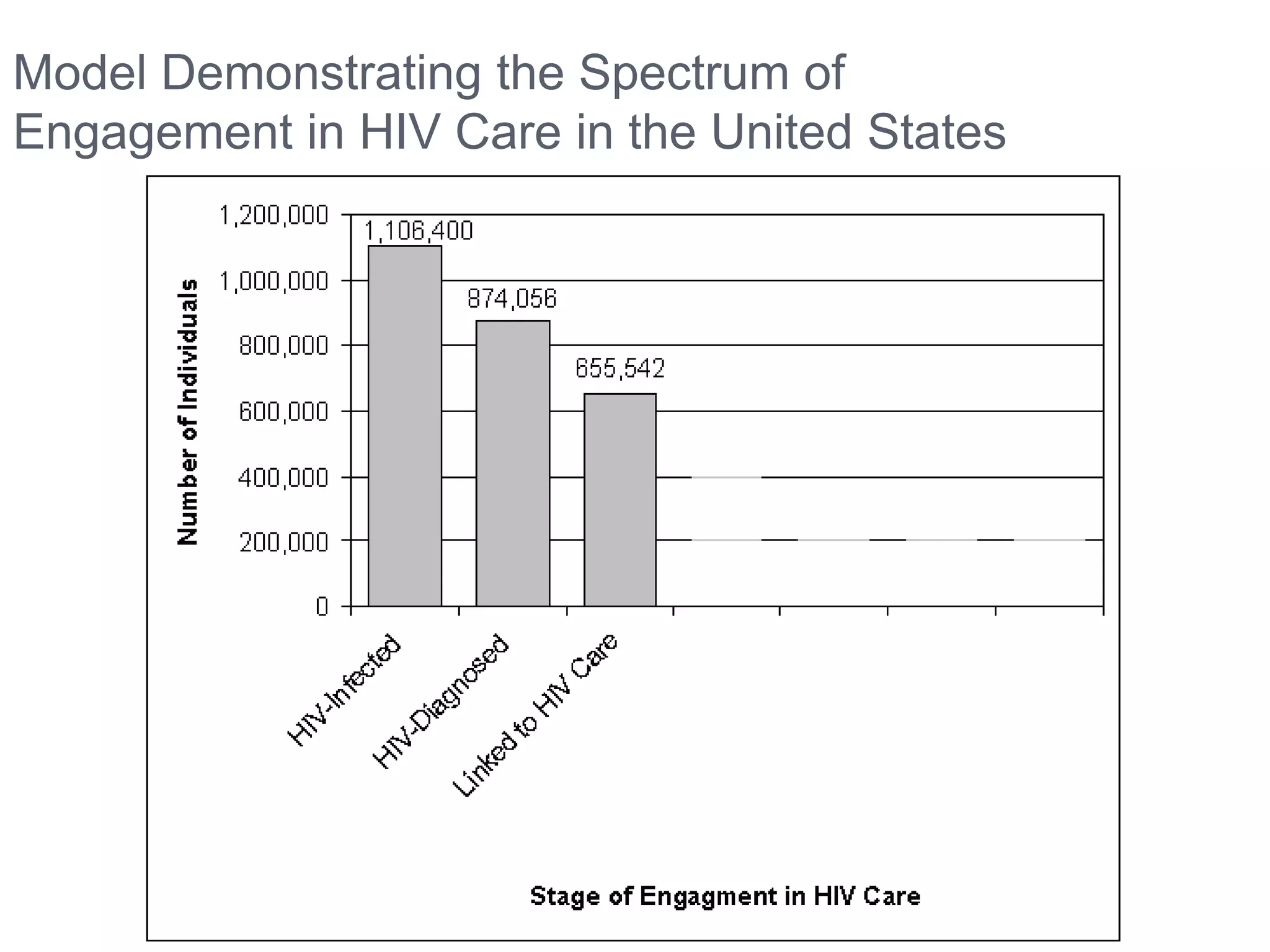
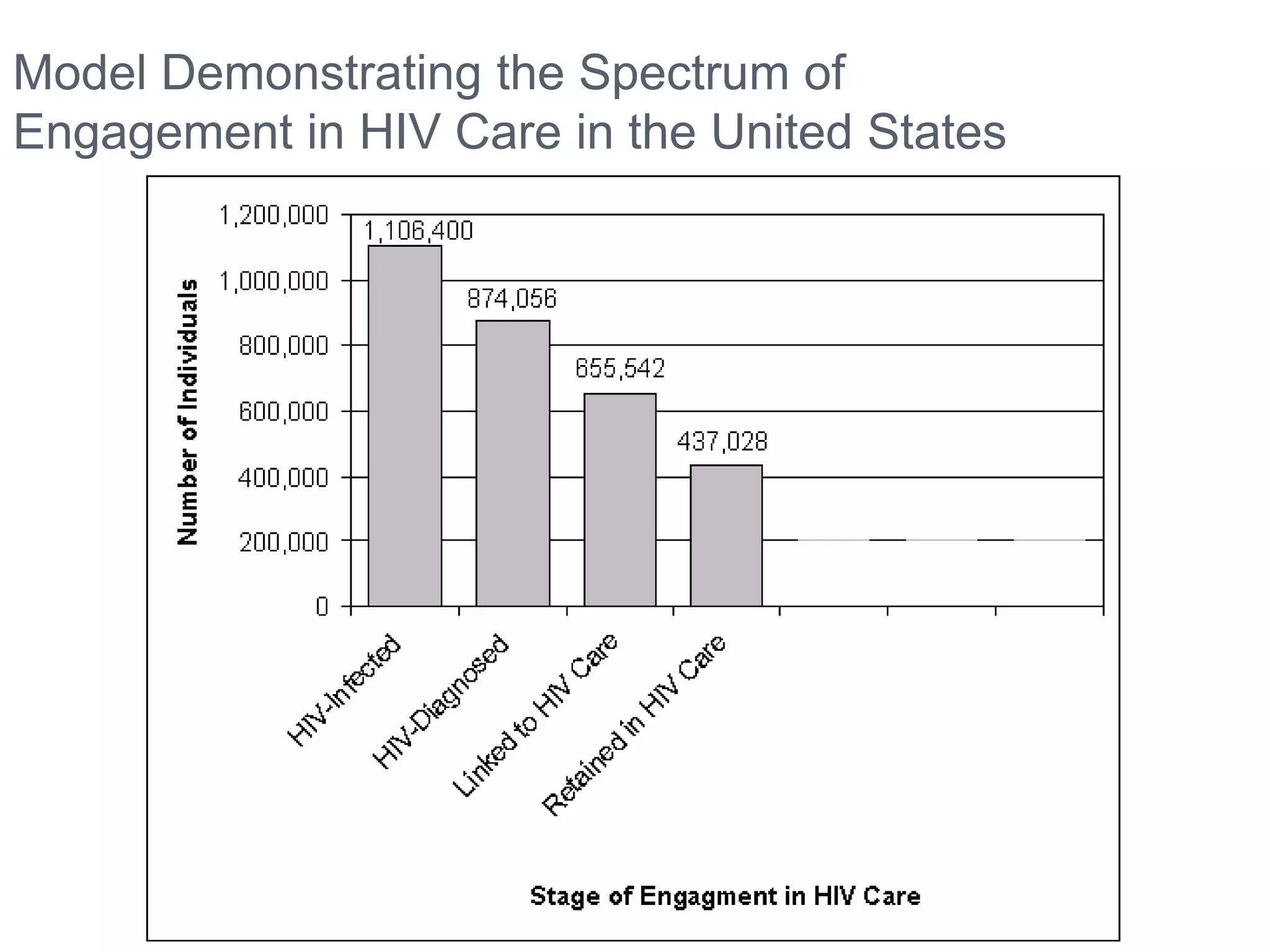
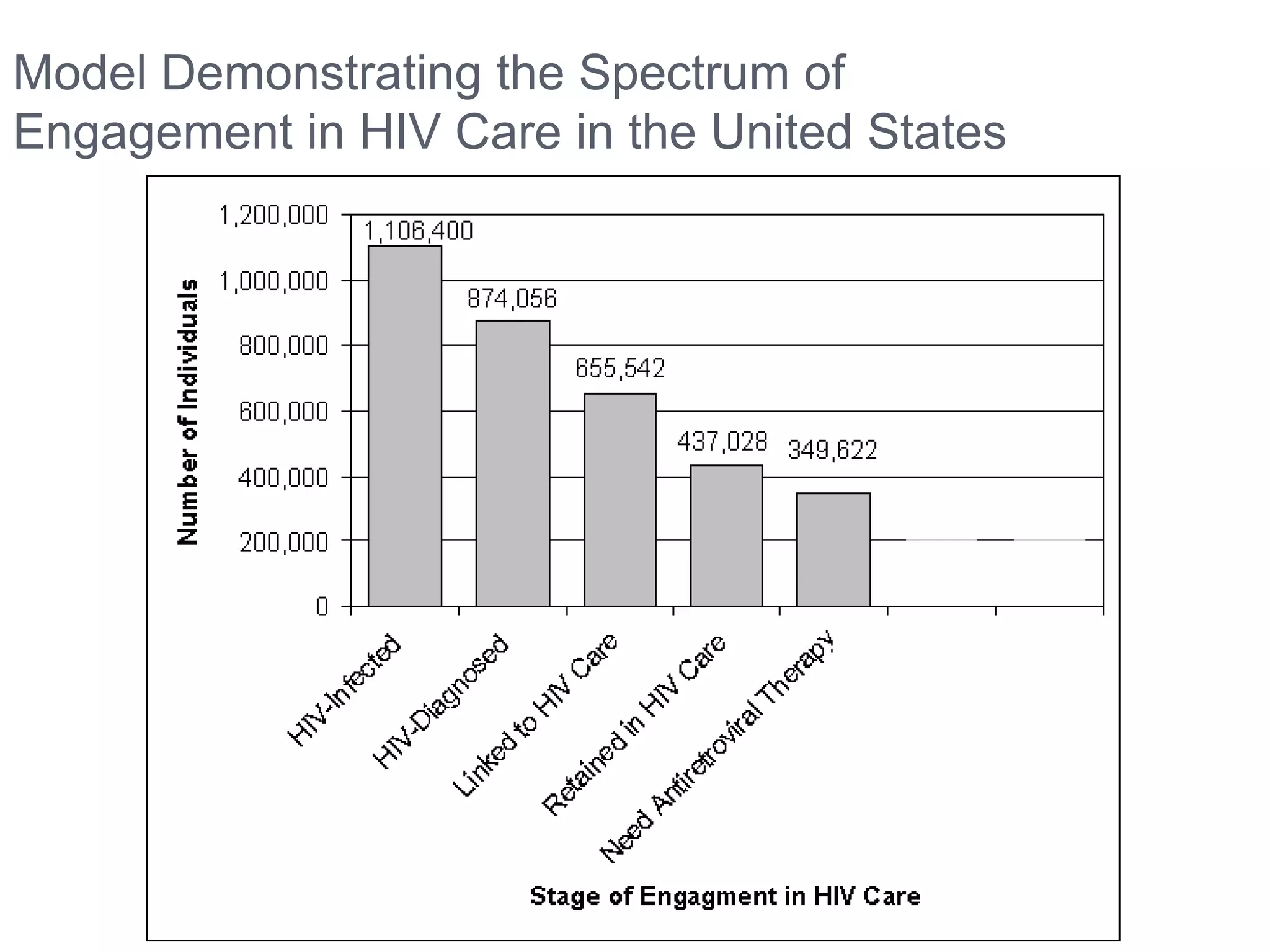
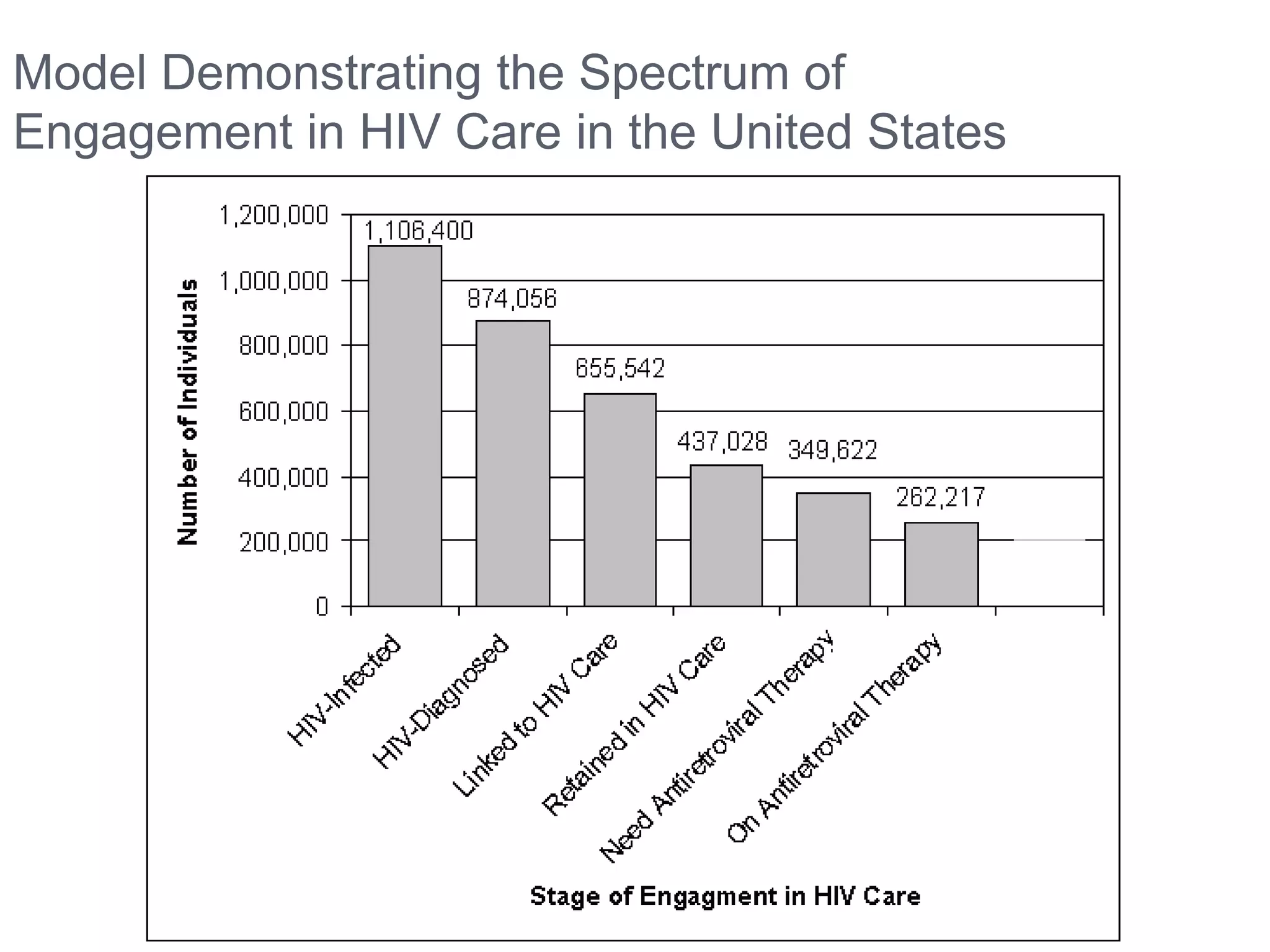
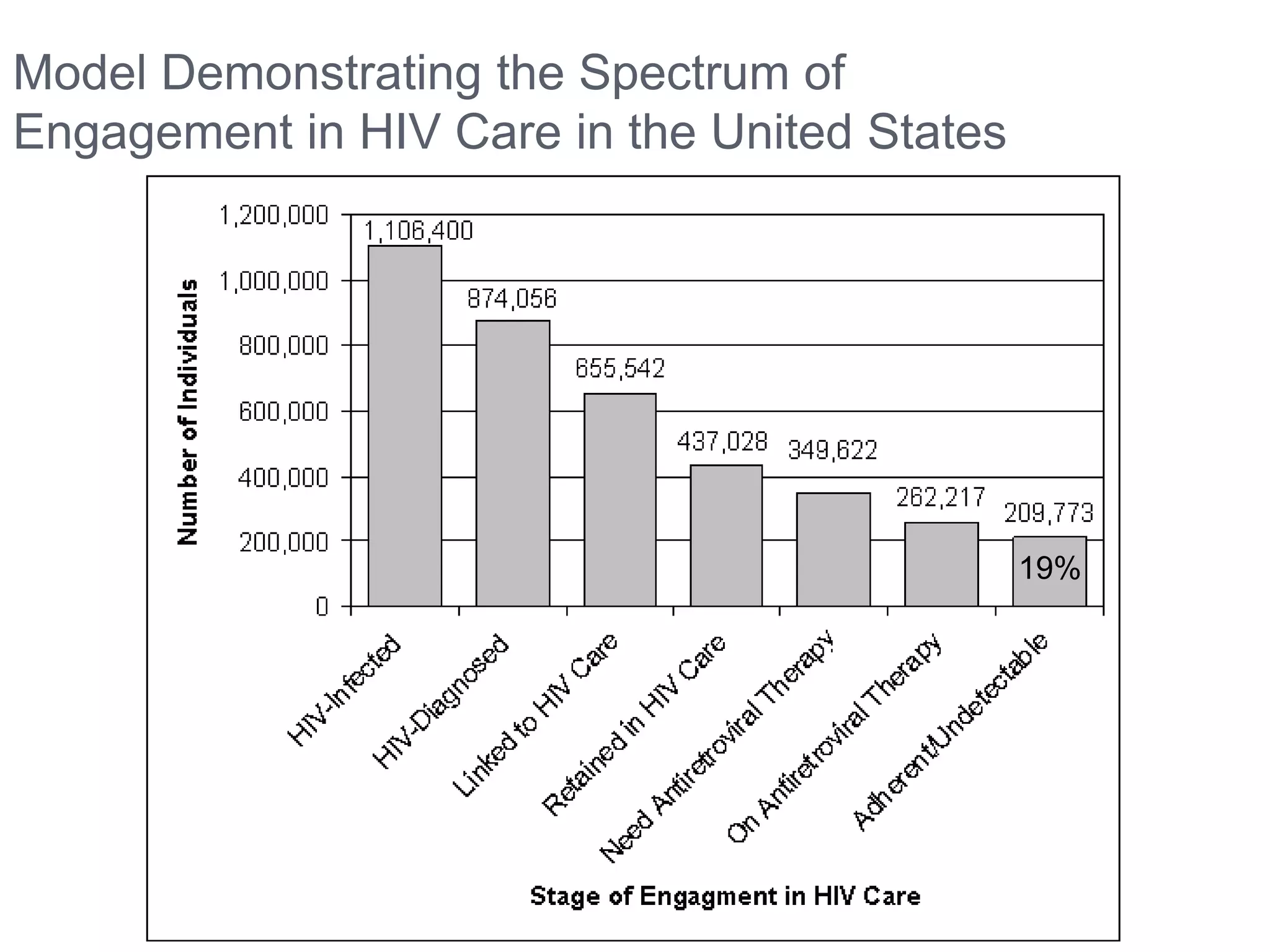
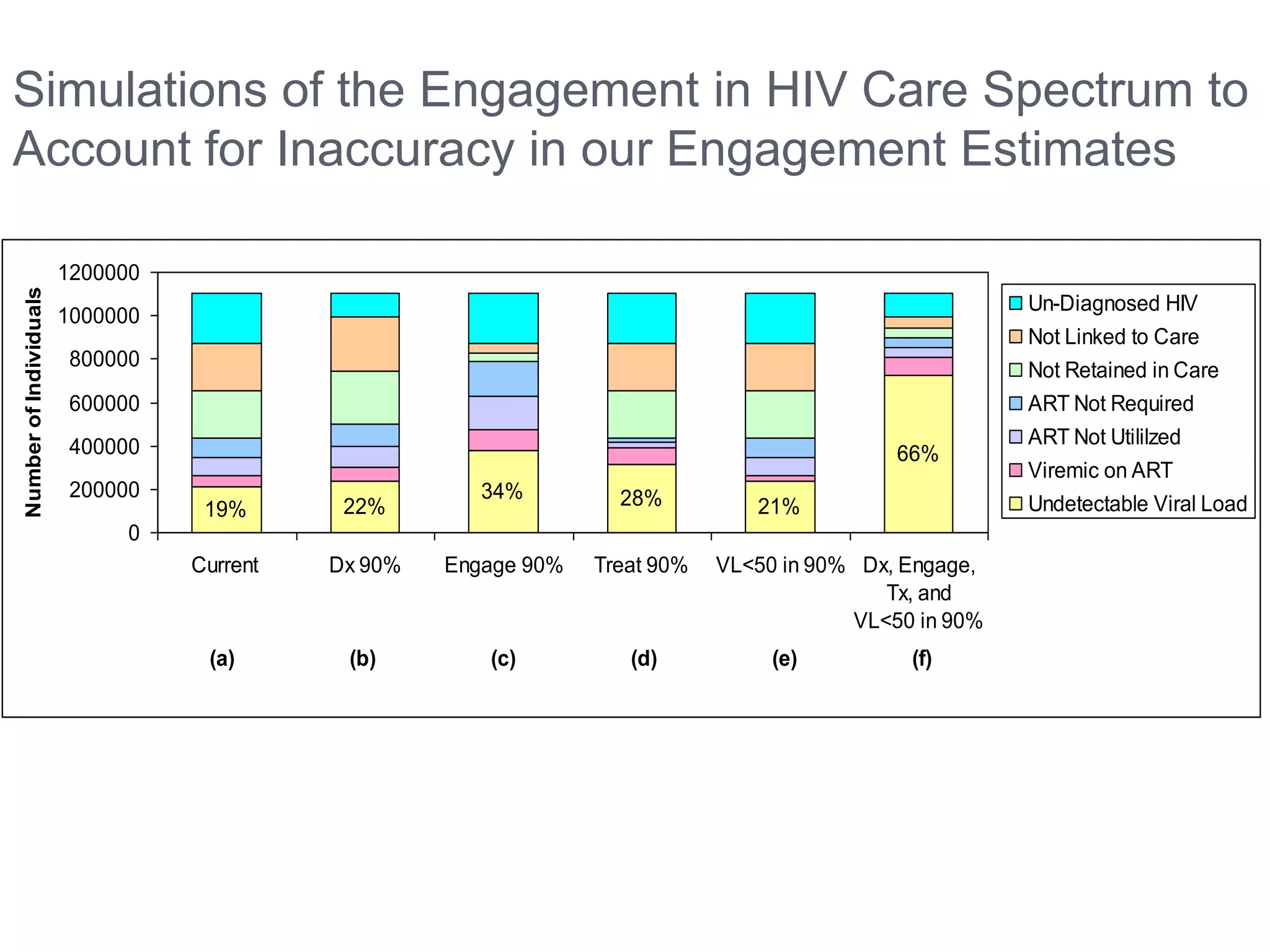
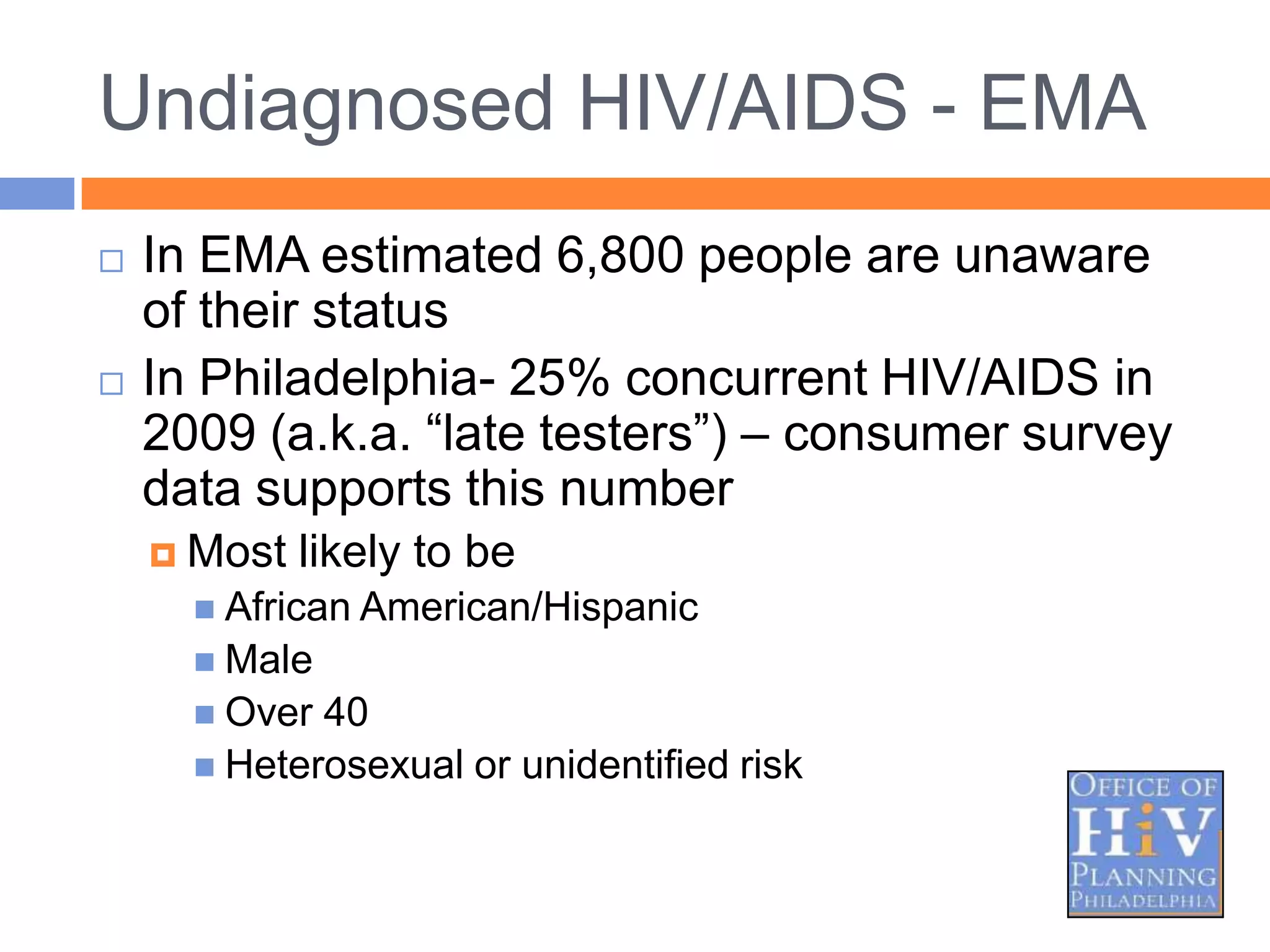
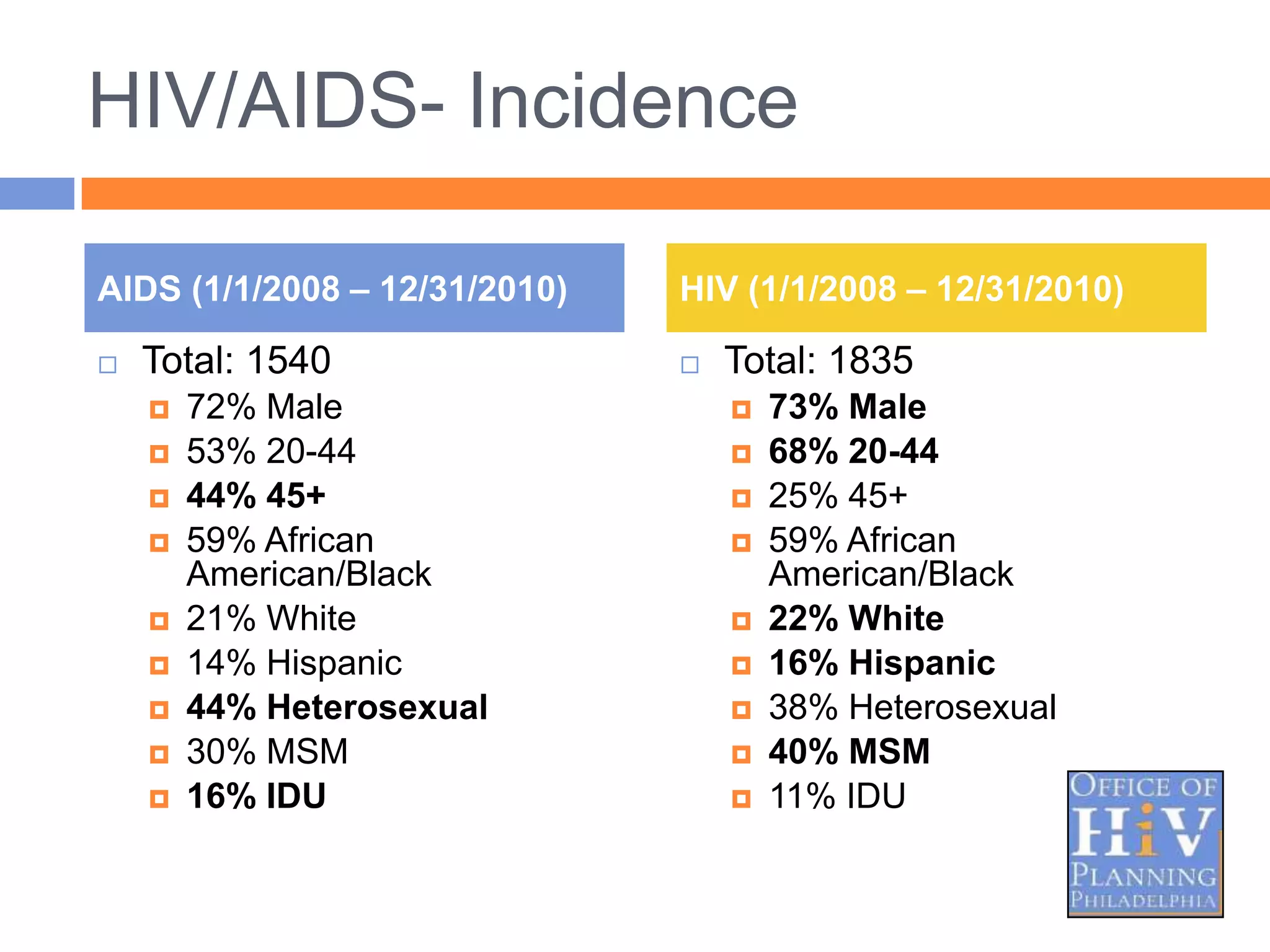
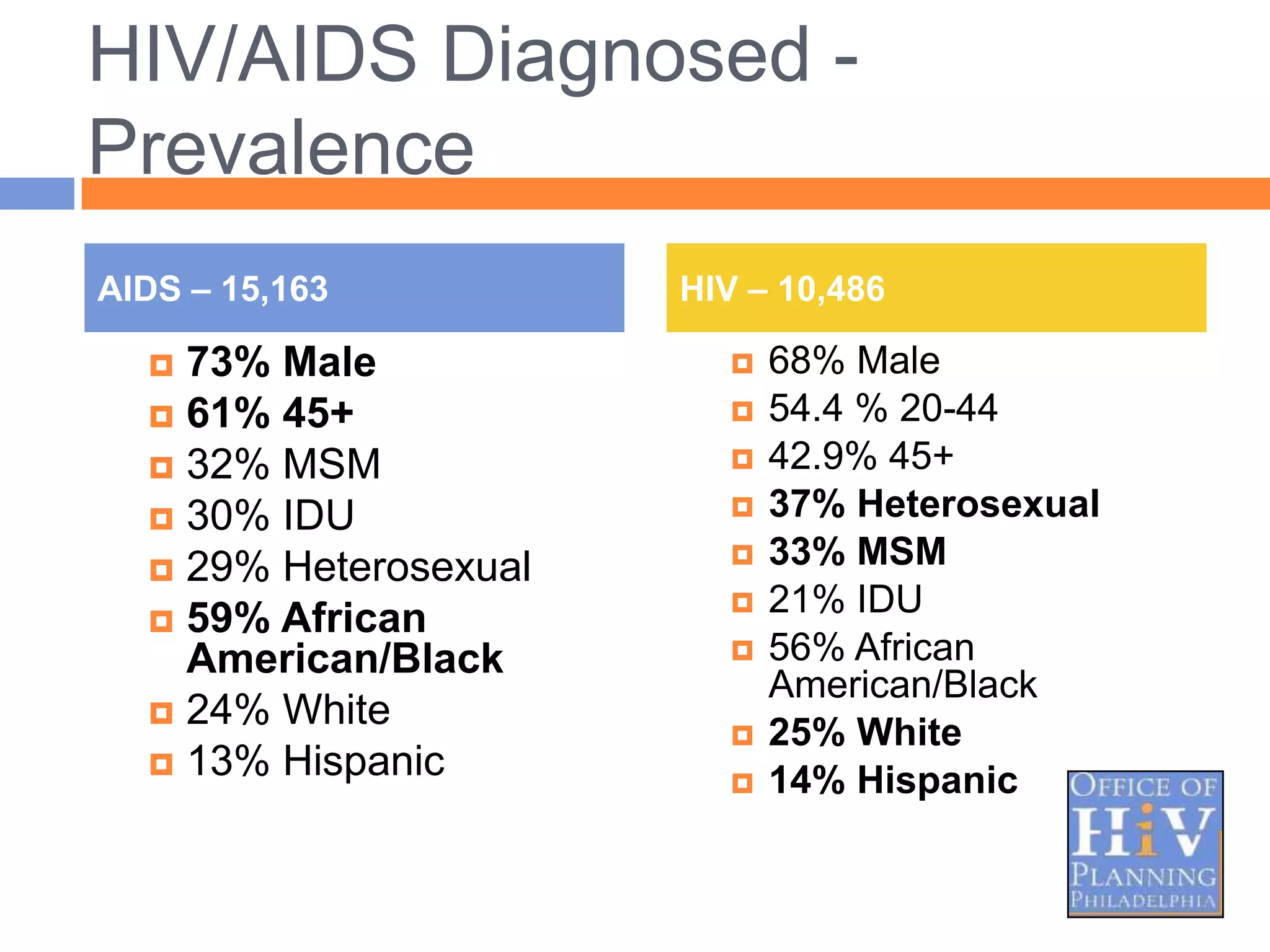
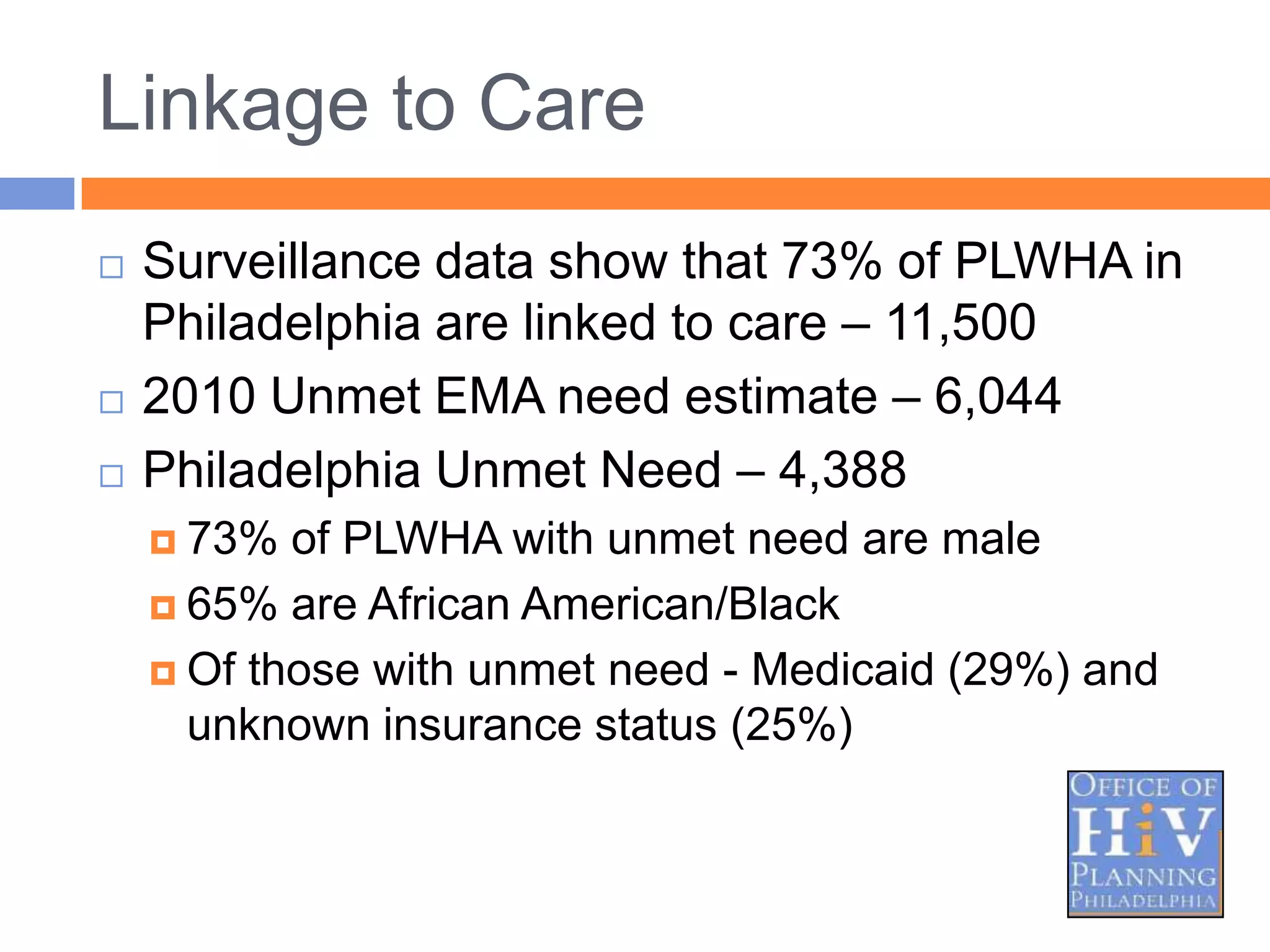
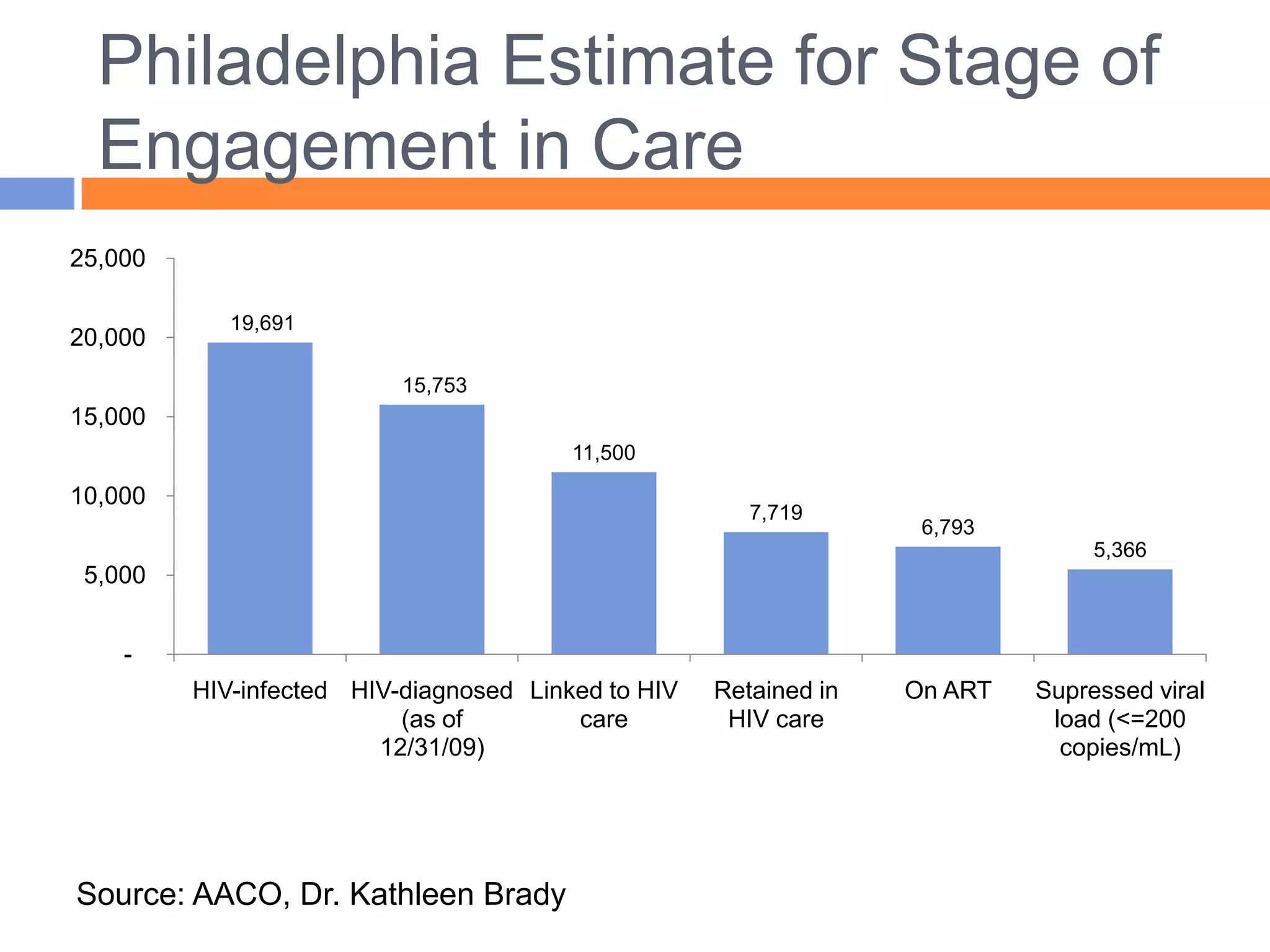
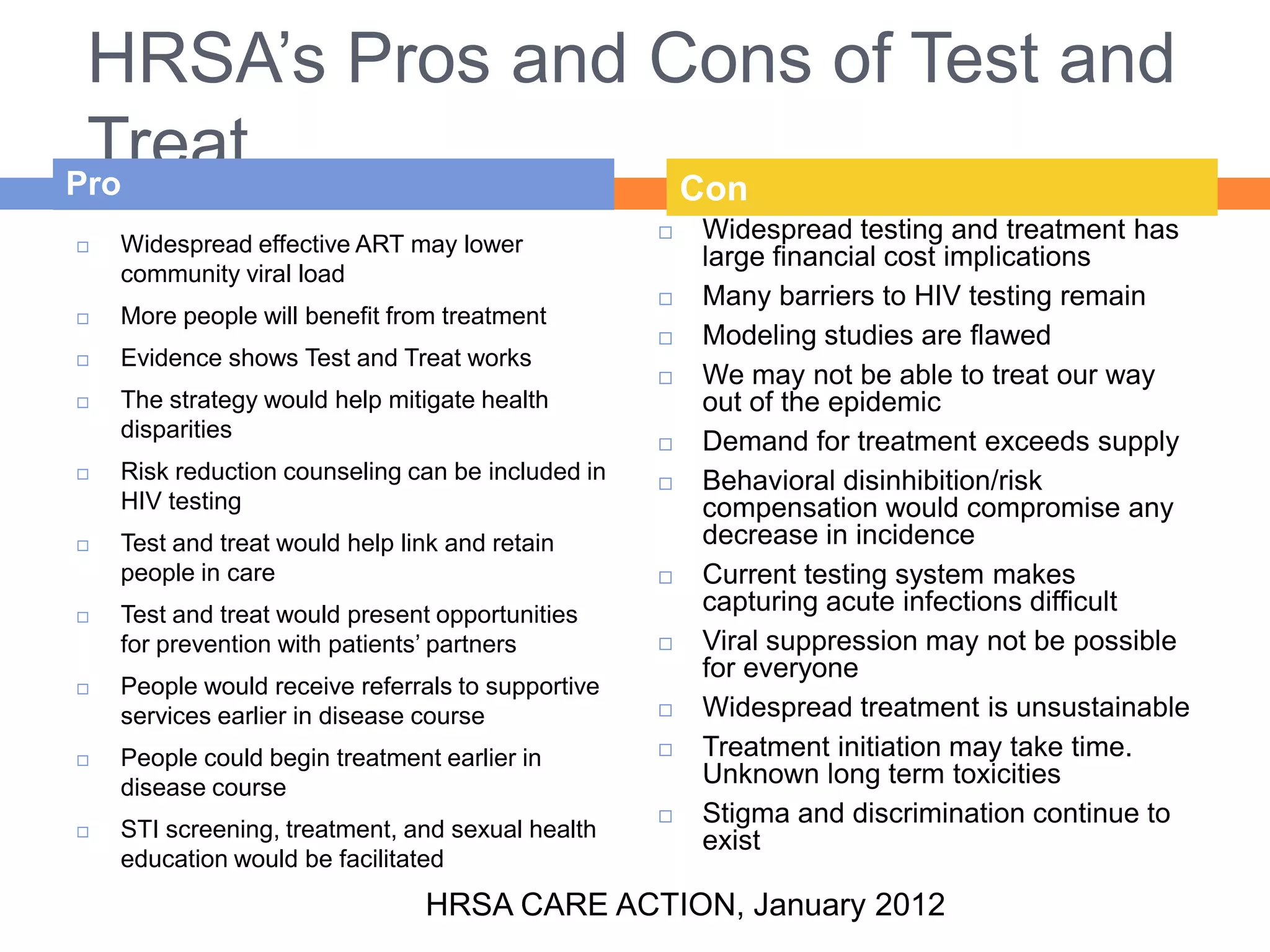
The document discusses the 'test and treat' strategy for HIV management, emphasizing the importance of early diagnosis, linkage to care, and adherence to antiretroviral therapy for successful outcomes. It highlights barriers to effective care in the U.S., including late diagnosis and inadequate retention in care, which impede community viral load reduction and increase transmission risk. The findings from Gardner's review stress the need for improved engagement in the HIV care continuum to enhance treatment efficacy and public health outcomes.