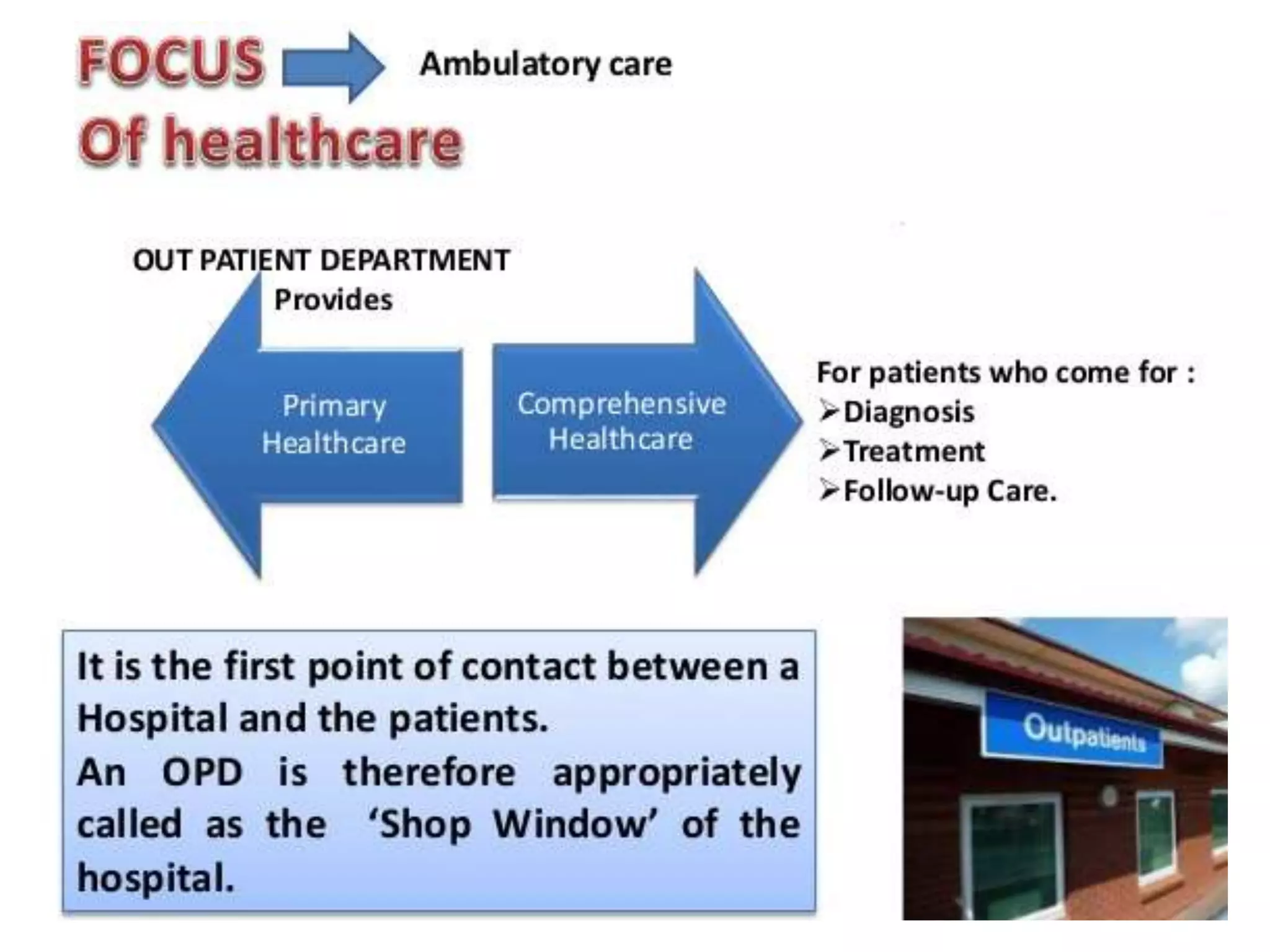
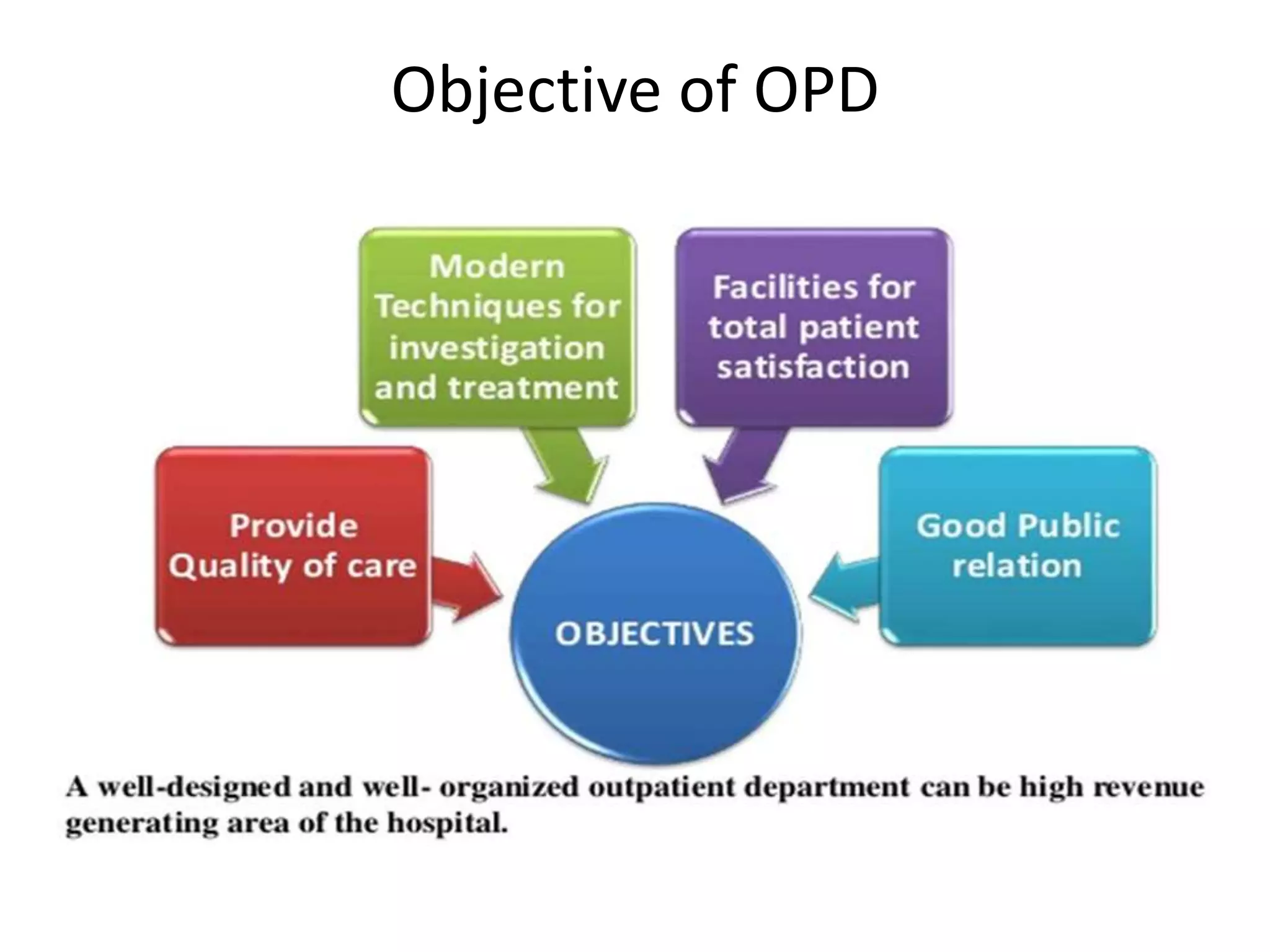
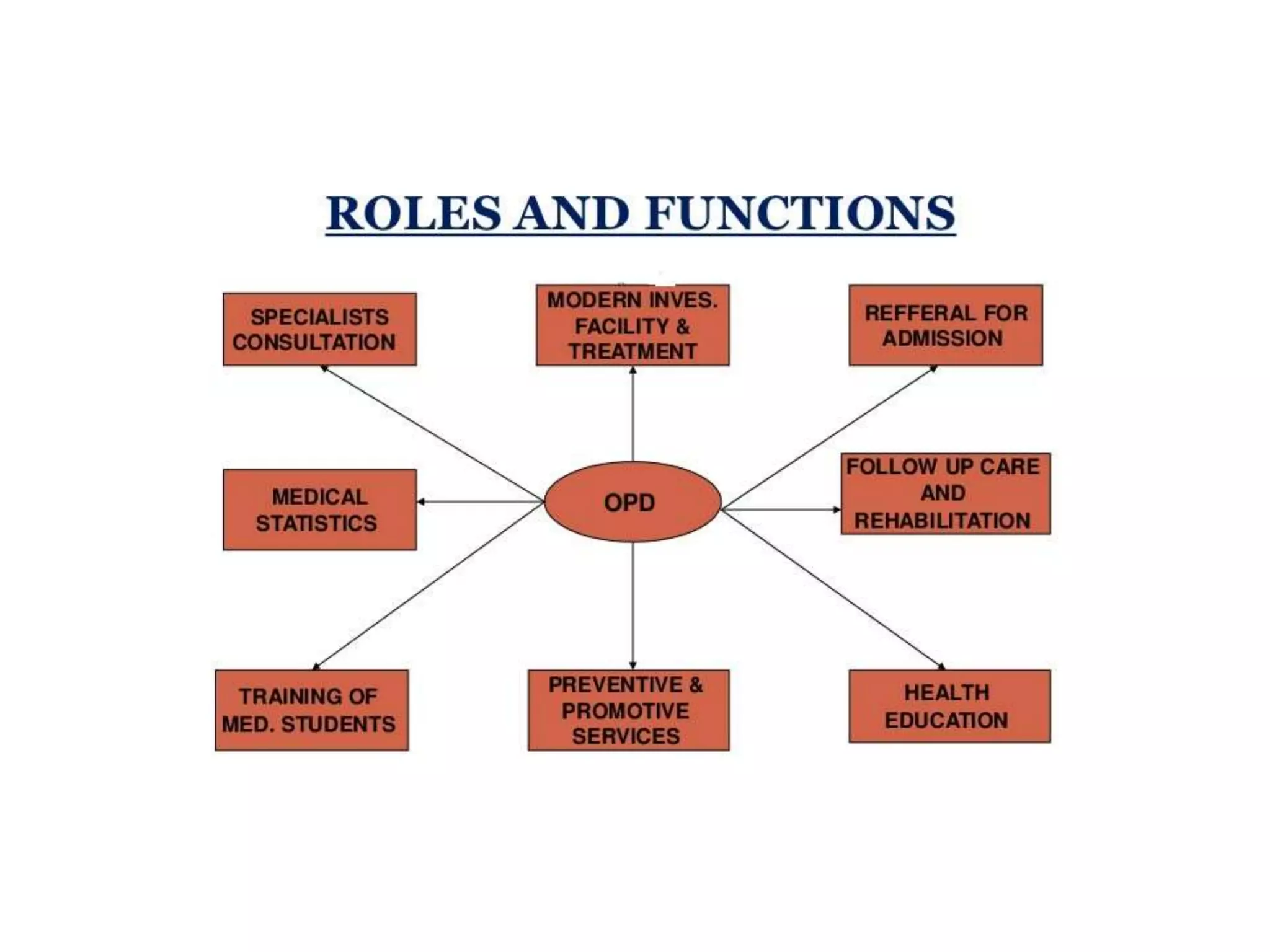
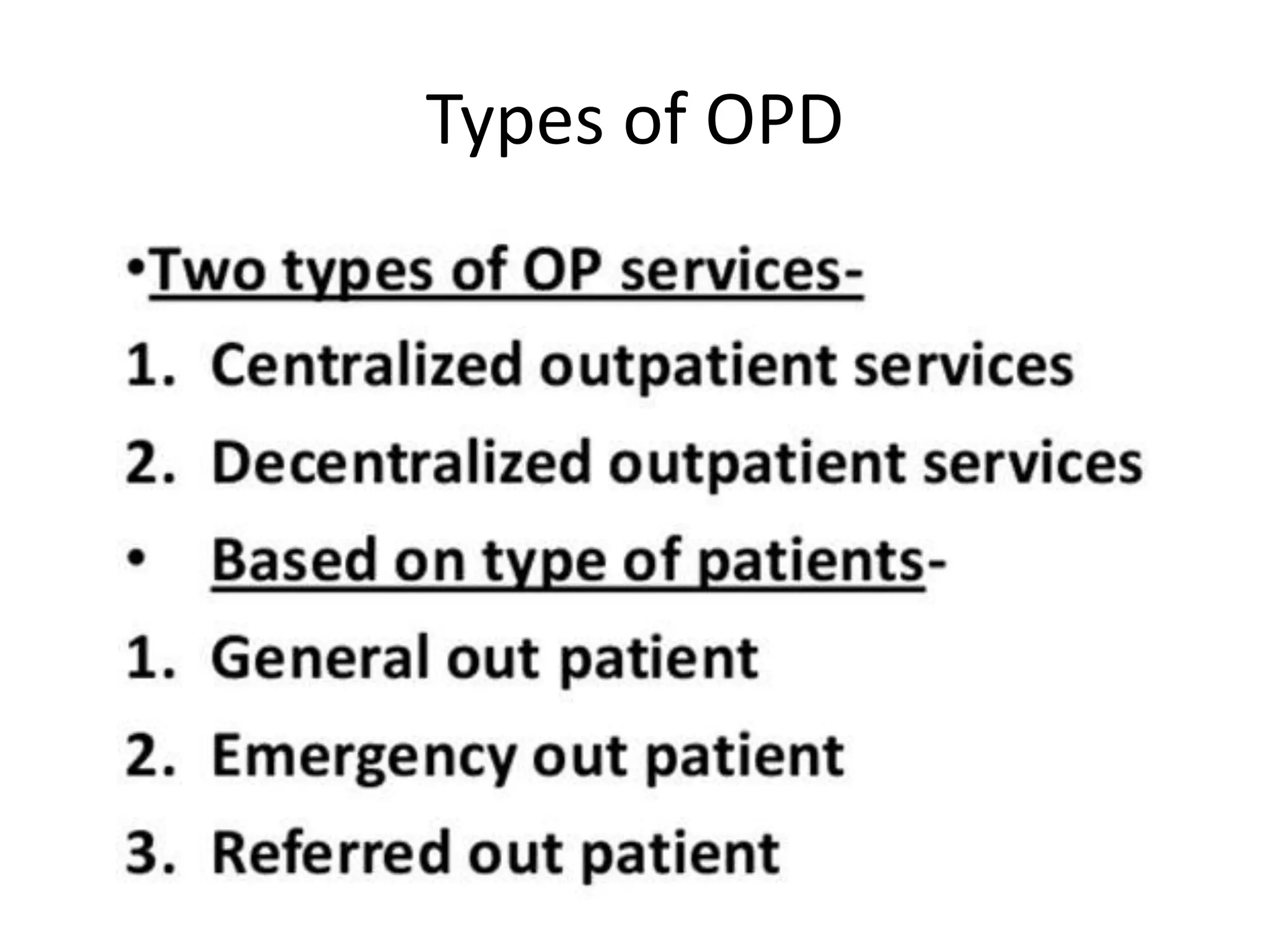
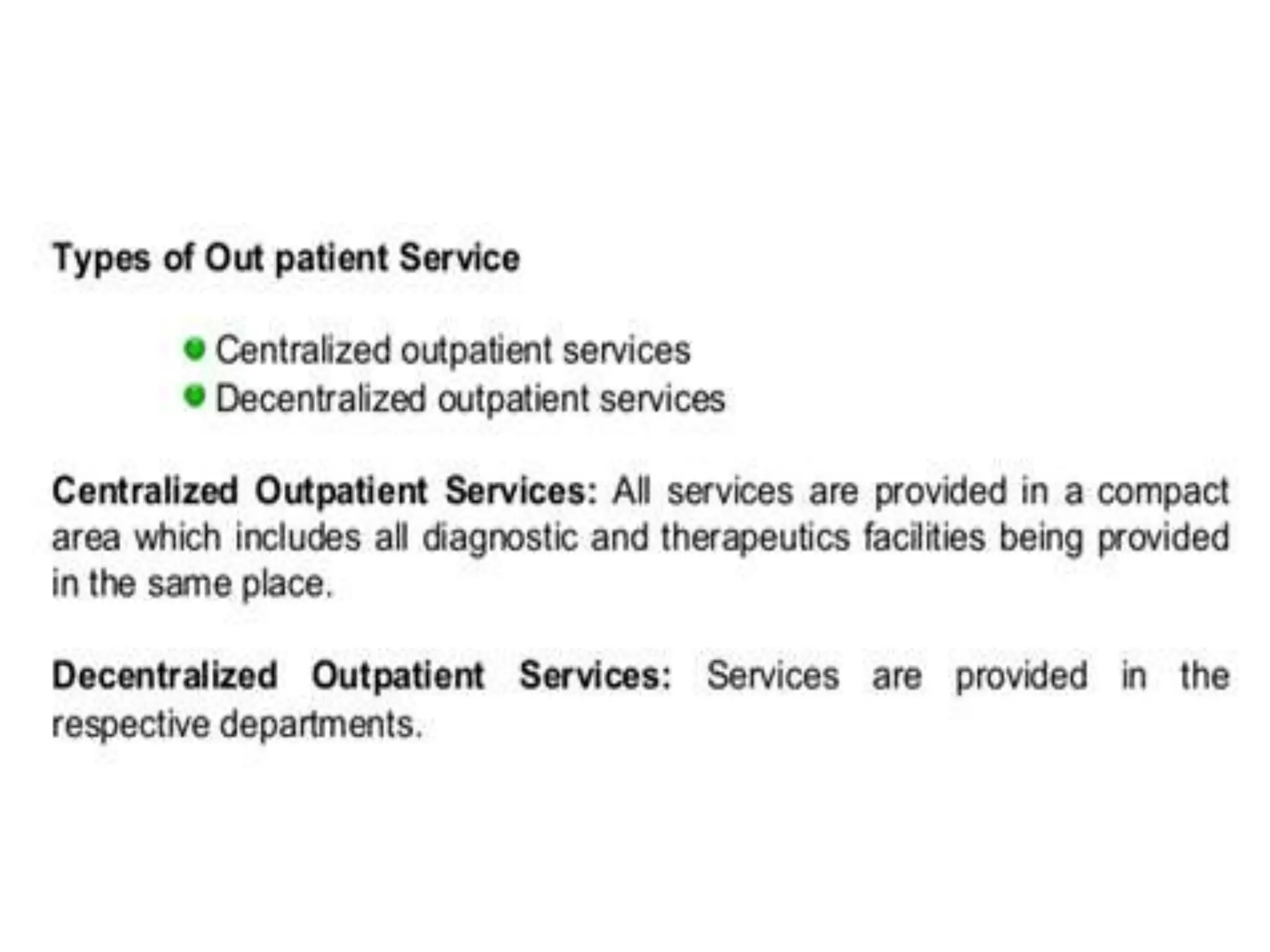
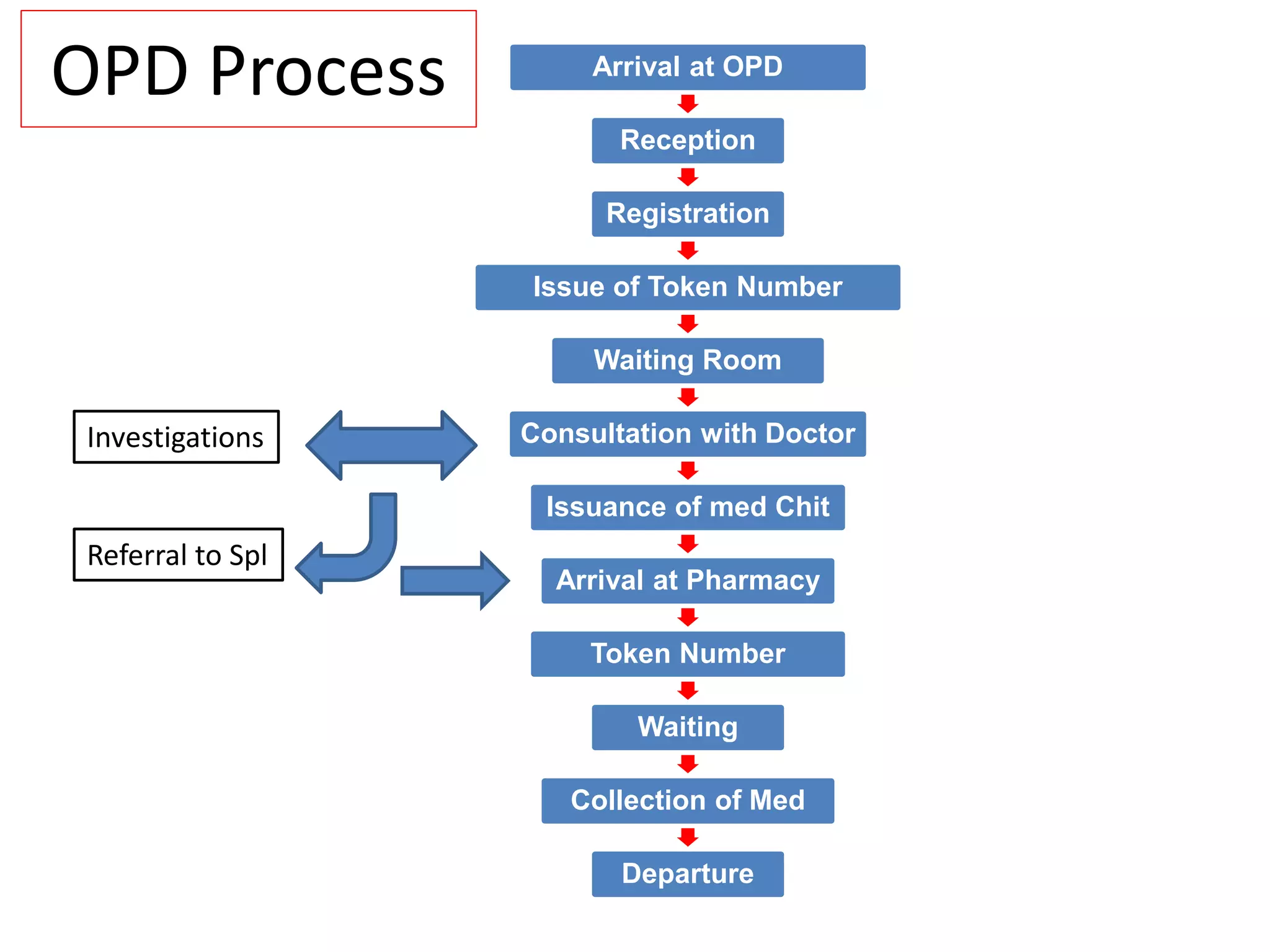
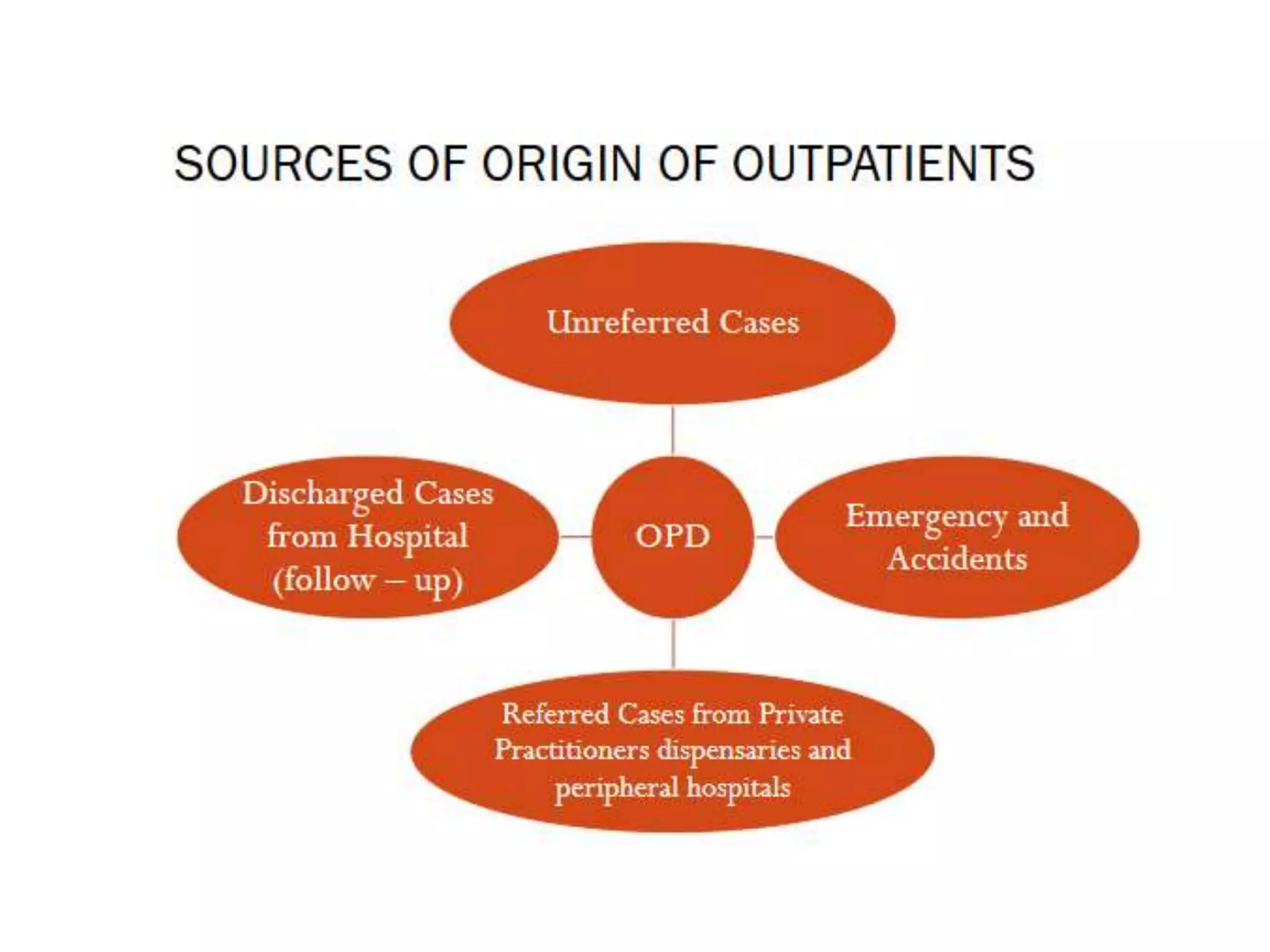
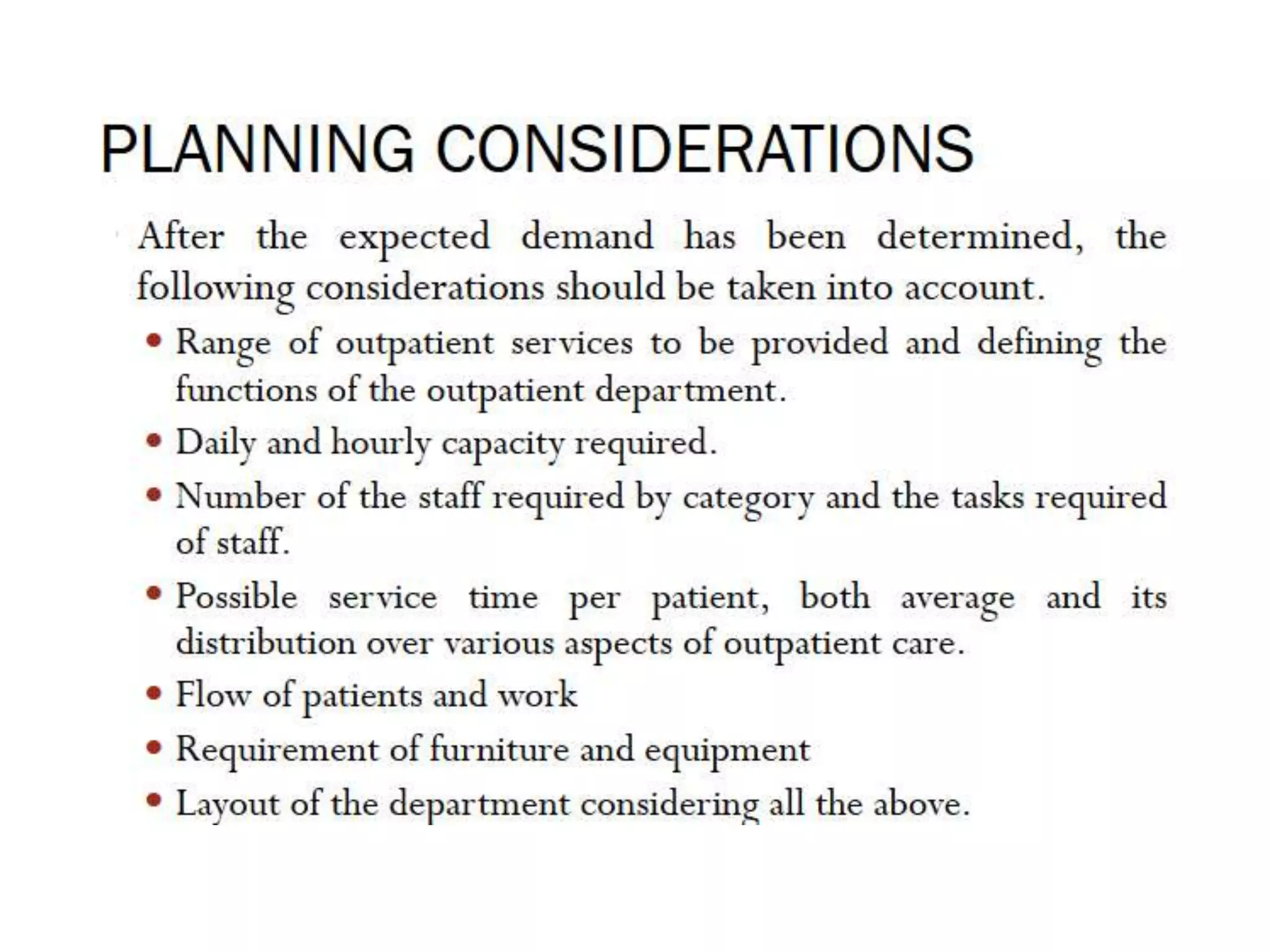
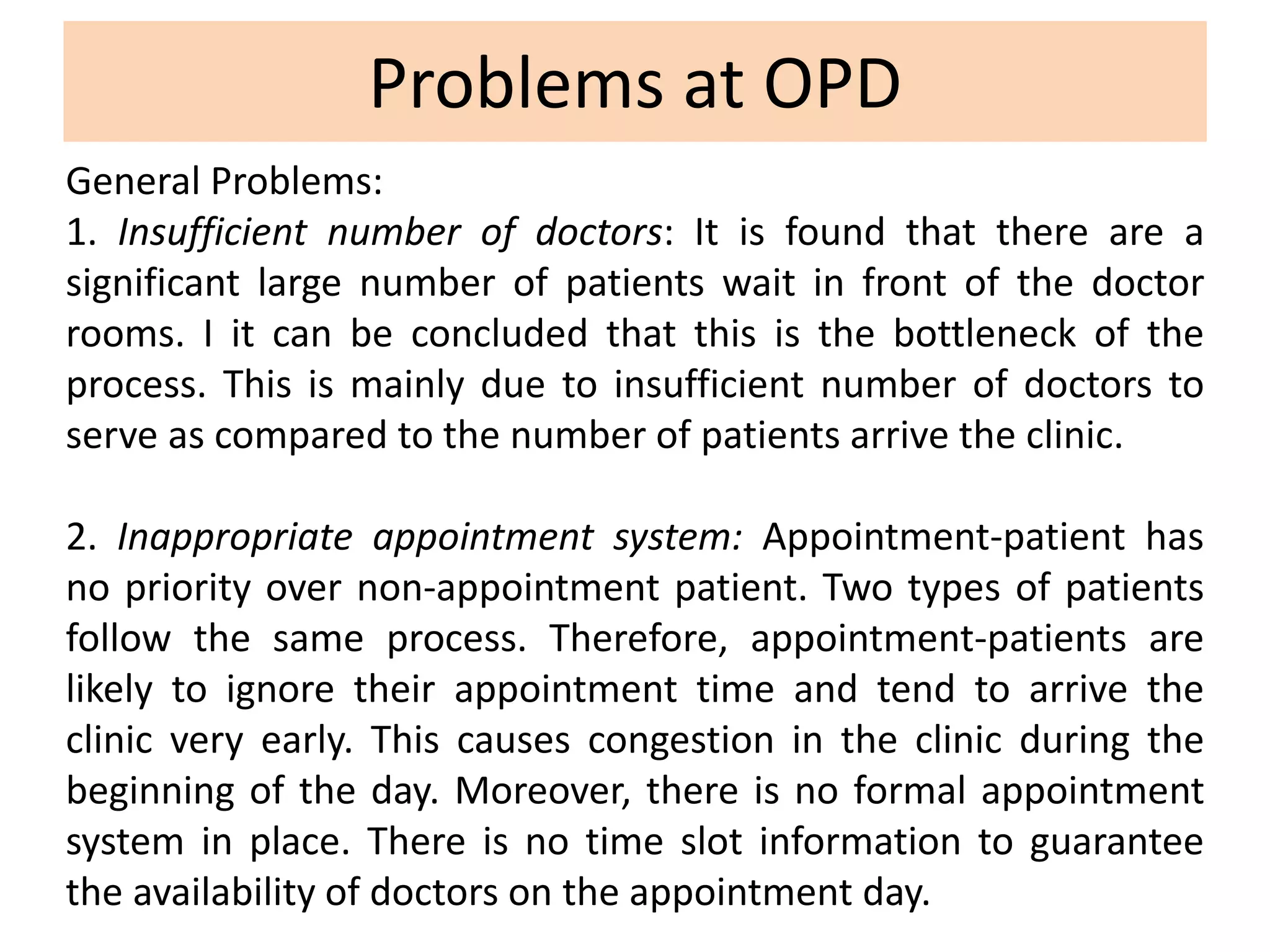
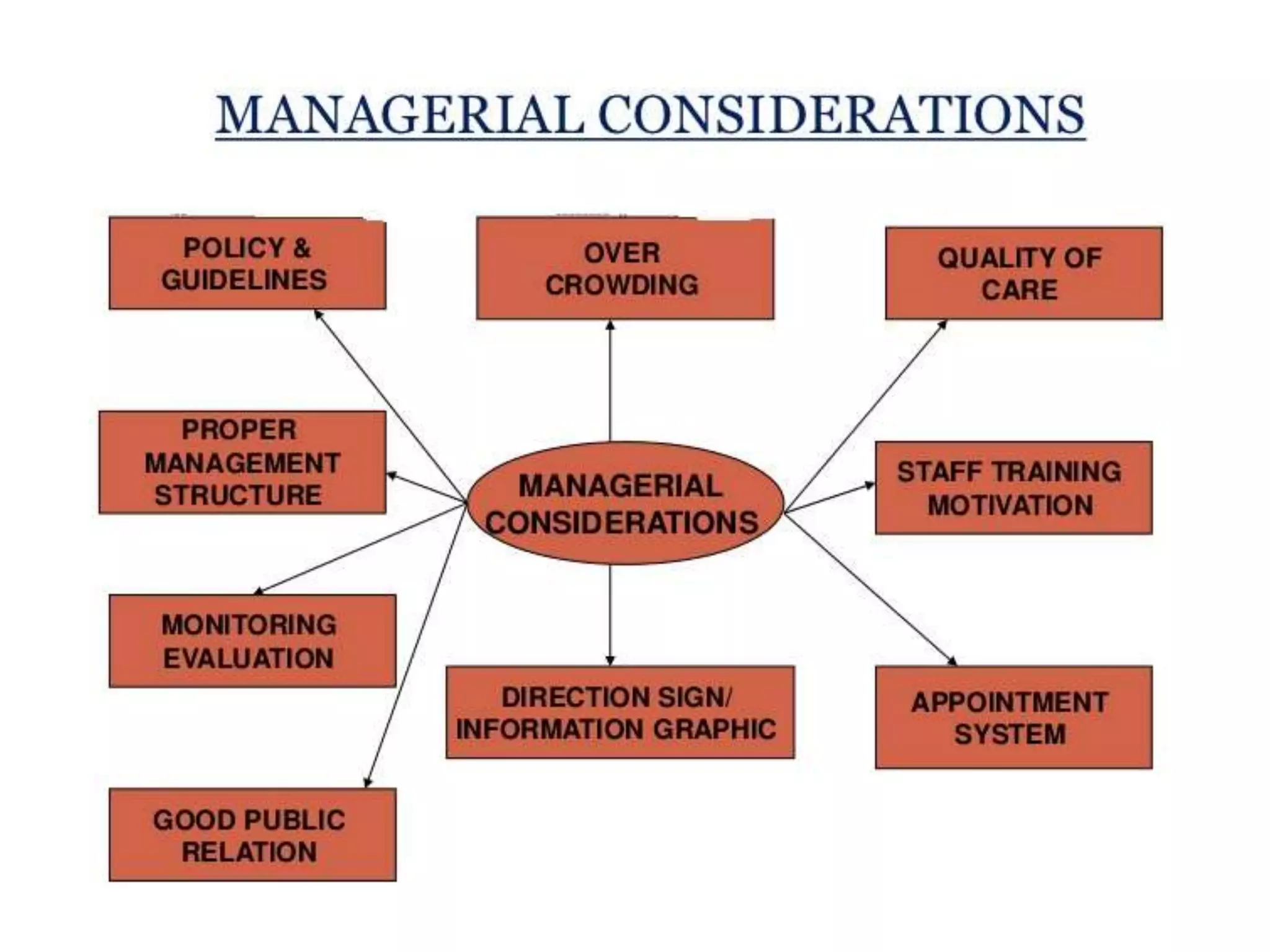
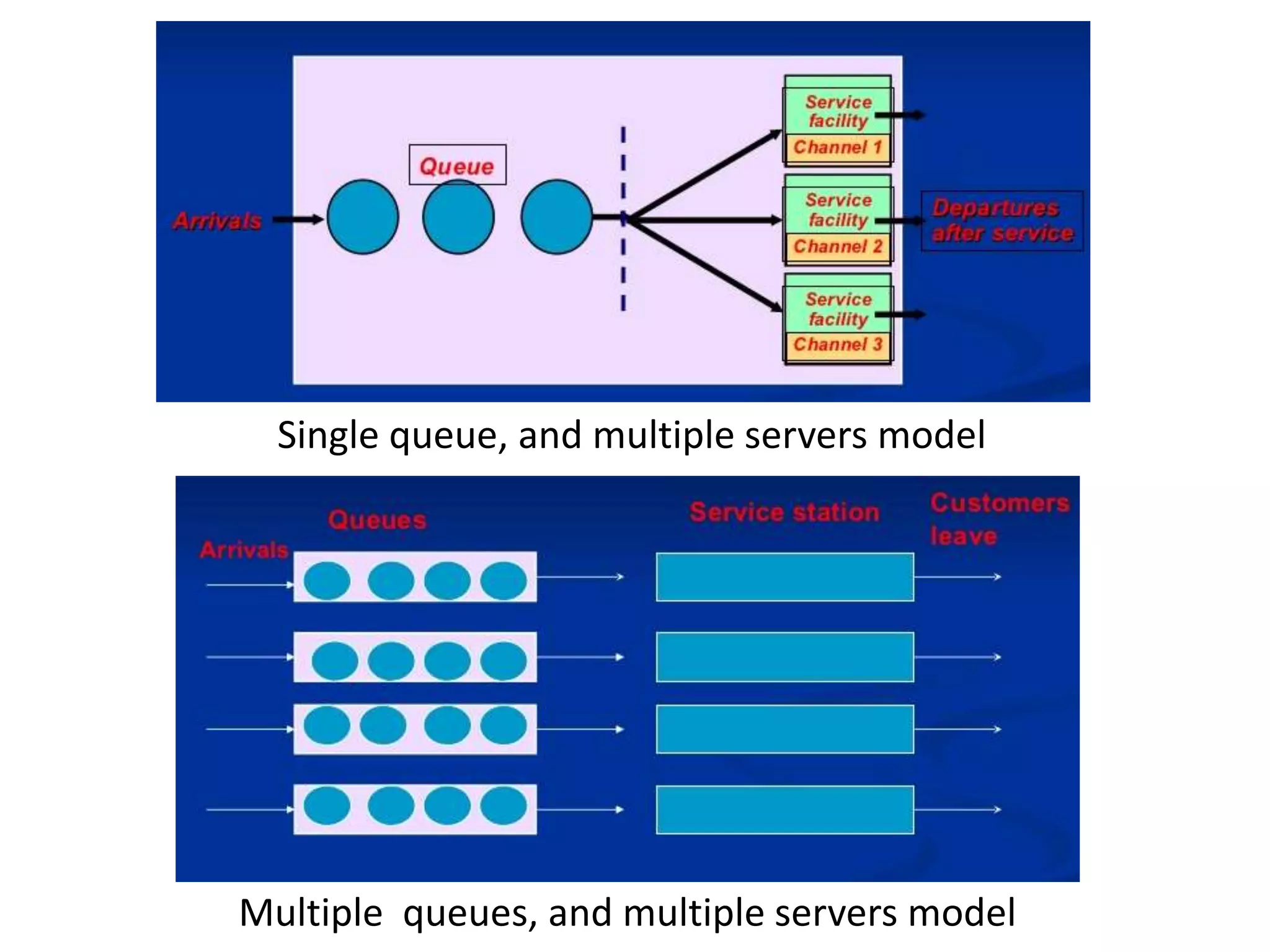
This document discusses outpatient departments (OPDs) in hospitals. It defines an OPD as the department of a hospital that provides care to non-inpatients on an outpatient basis. The document outlines the objectives, history, and types of OPDs. It describes the facilities and process of an OPD visit. Common problems at OPDs are identified such as long wait times and staffing shortages. Suggestions are provided to address issues like managing patient queues and improving record keeping.