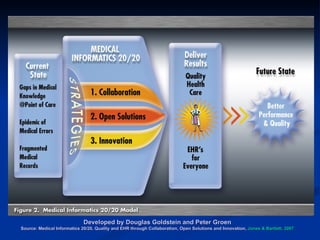
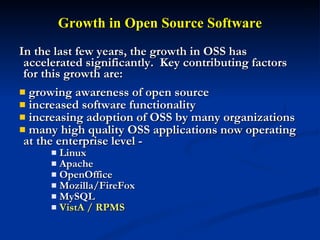
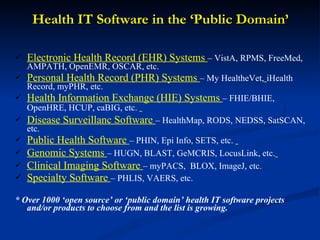
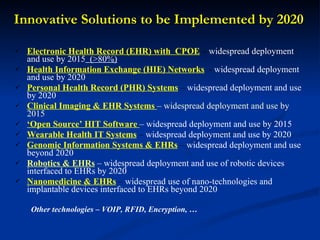
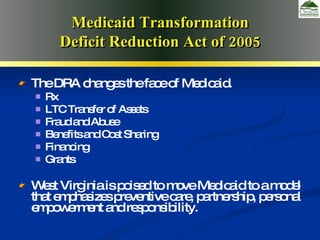
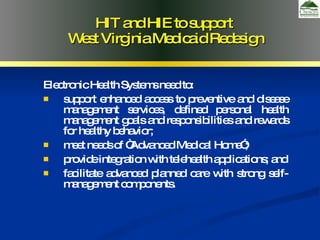
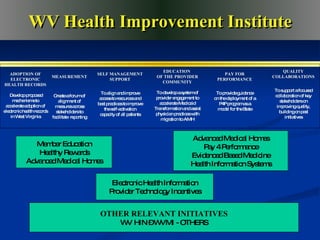
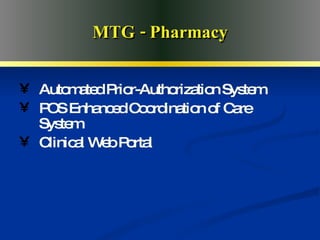
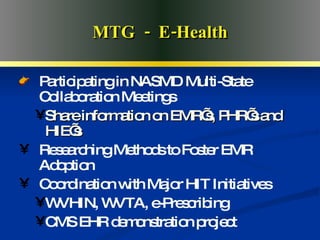
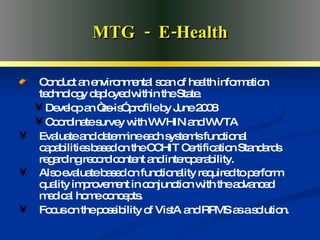
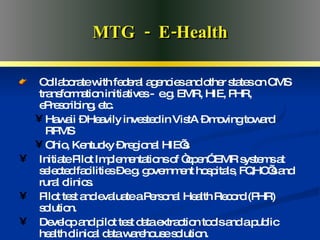
The document discusses West Virginia's vision for transforming its Medicaid program and healthcare system through the use of health information technology and electronic health records by 2020. It outlines strategies around collaboration, open solutions, and innovation to achieve an integrated system with interconnected EHRs, personal health records, telehealth, and mobile access to patient information. Key goals include widespread adoption of EHRs, health information exchange networks, and use of open-source software by 2020.