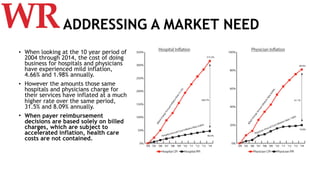
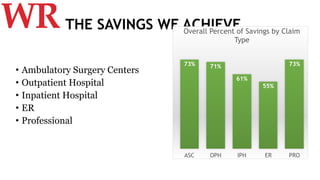
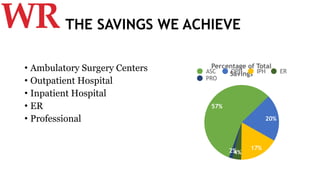
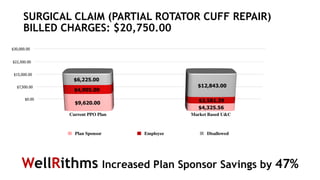
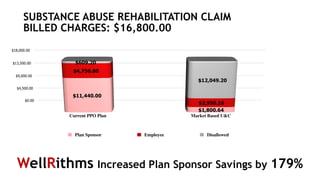
This document describes WellRithms' approach to claim review and summarizes their solution. It notes that while costs for hospitals and physicians have increased mildly in recent years, the amounts they charge have inflated much more. WellRithms develops a defensible market rate for reimbursements by analyzing cost, billed, and Medicare data specific to a geographic area in a transparent methodology. This approach results in significant savings for self-funded plans of 3% average appeal rate and savings ranging from 55-73% across different claim types, with inpatient hospital claims making up the largest portion. Examples show savings of 47-179% on individual claims compared to standard reimbursements.