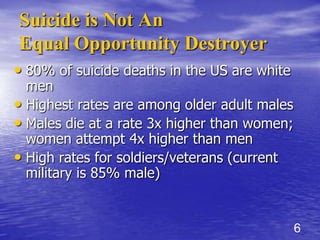
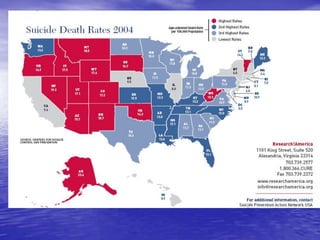
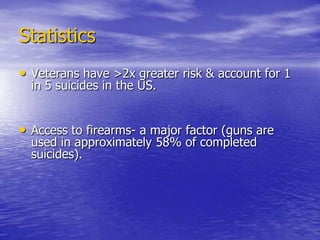
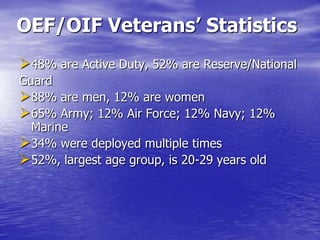
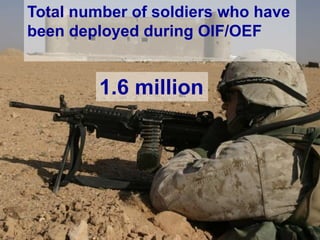
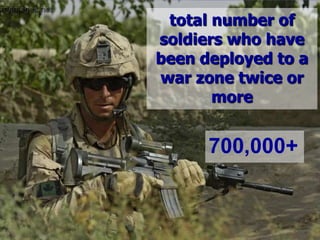
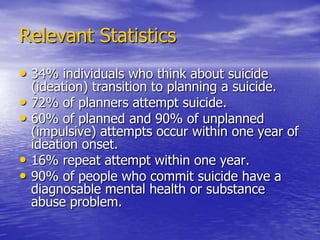
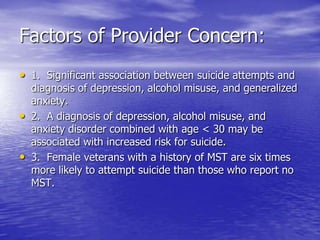
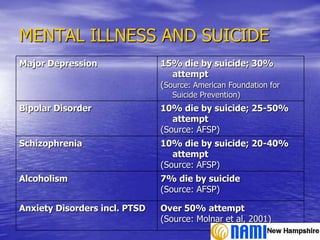
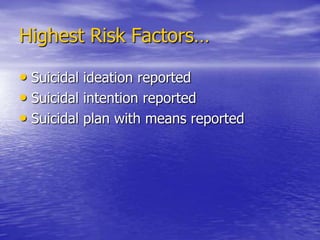
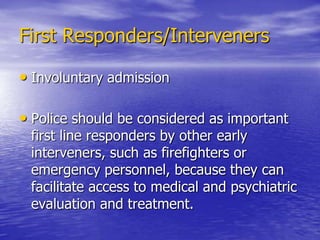
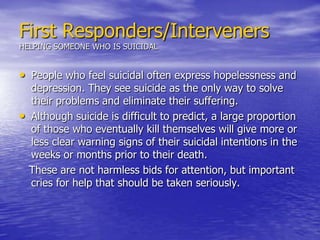
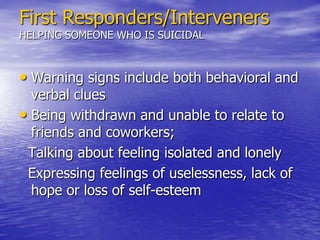
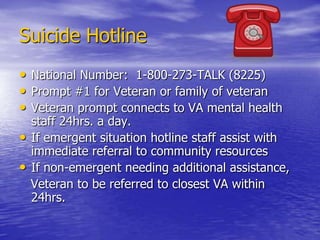
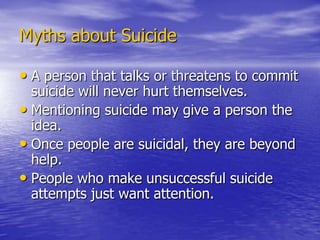
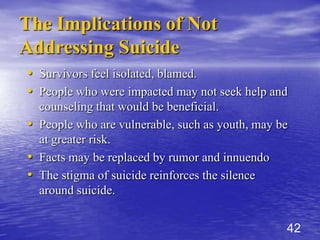
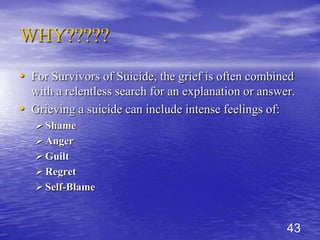
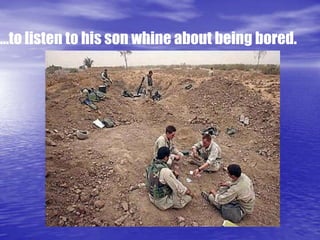
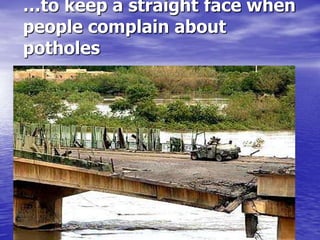
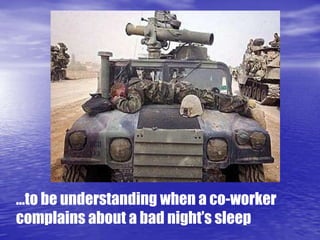
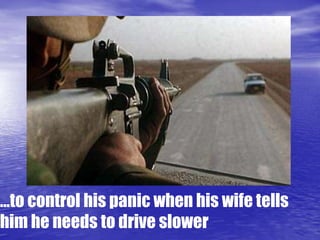
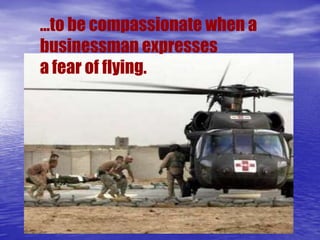
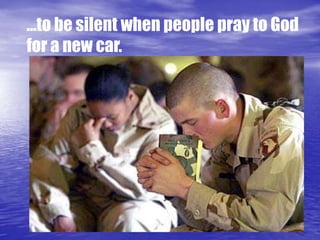
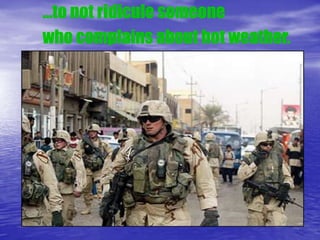
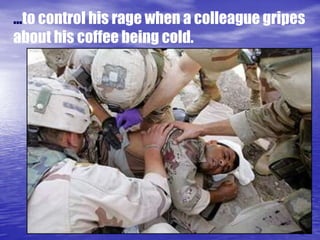
This document discusses suicide prevention, providing statistics on suicide rates, risk factors, and warning signs. It identifies veterans as being at higher risk of suicide due to factors like access to firearms and mental health issues. Warning signs of suicide include expressions of hopelessness, feelings of isolation, and talking about tidying up affairs. The document advises that if someone is suicidal, one should engage them, remove means of suicide if possible, connect them to mental health services, and not leave them alone.