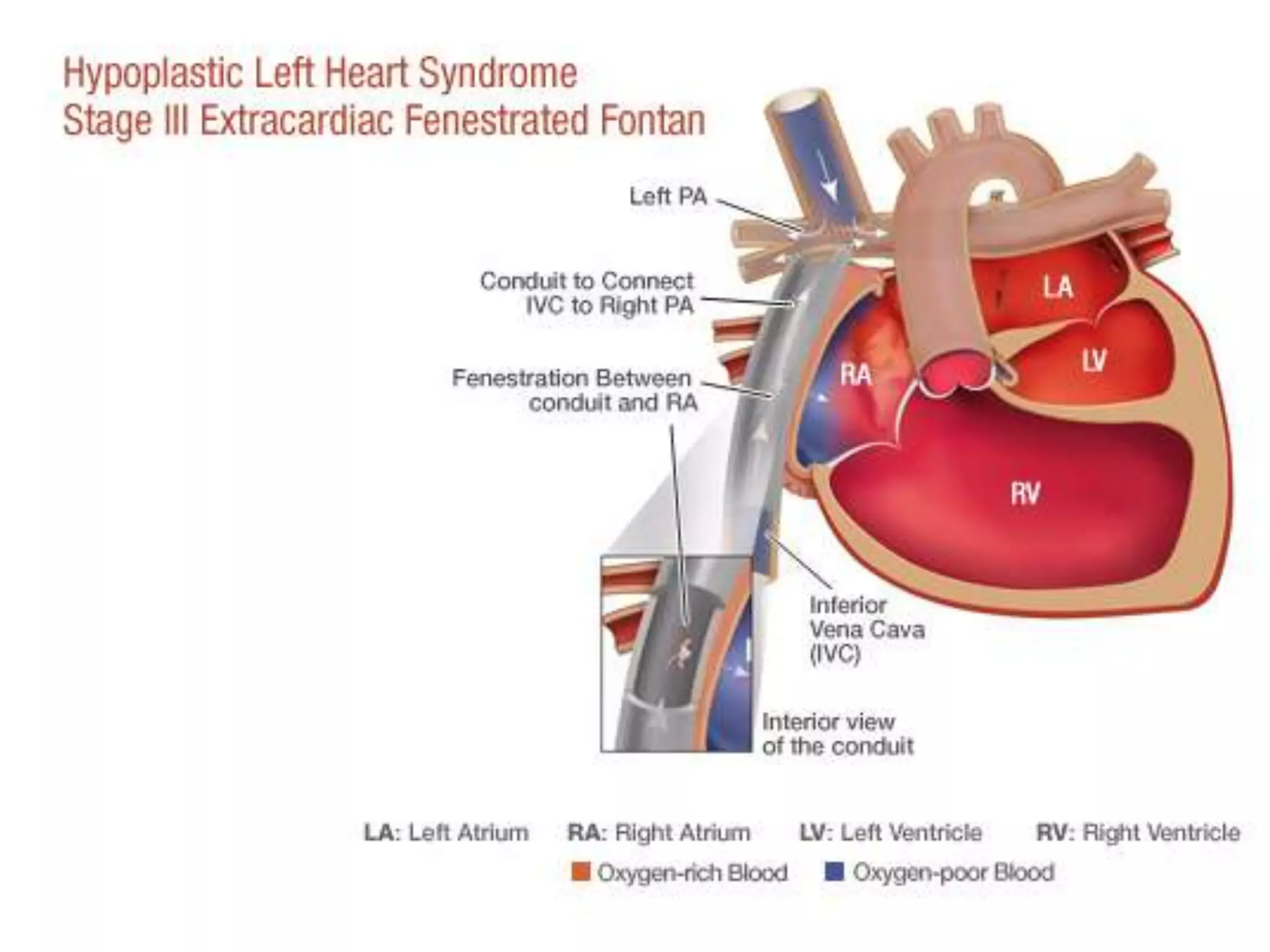
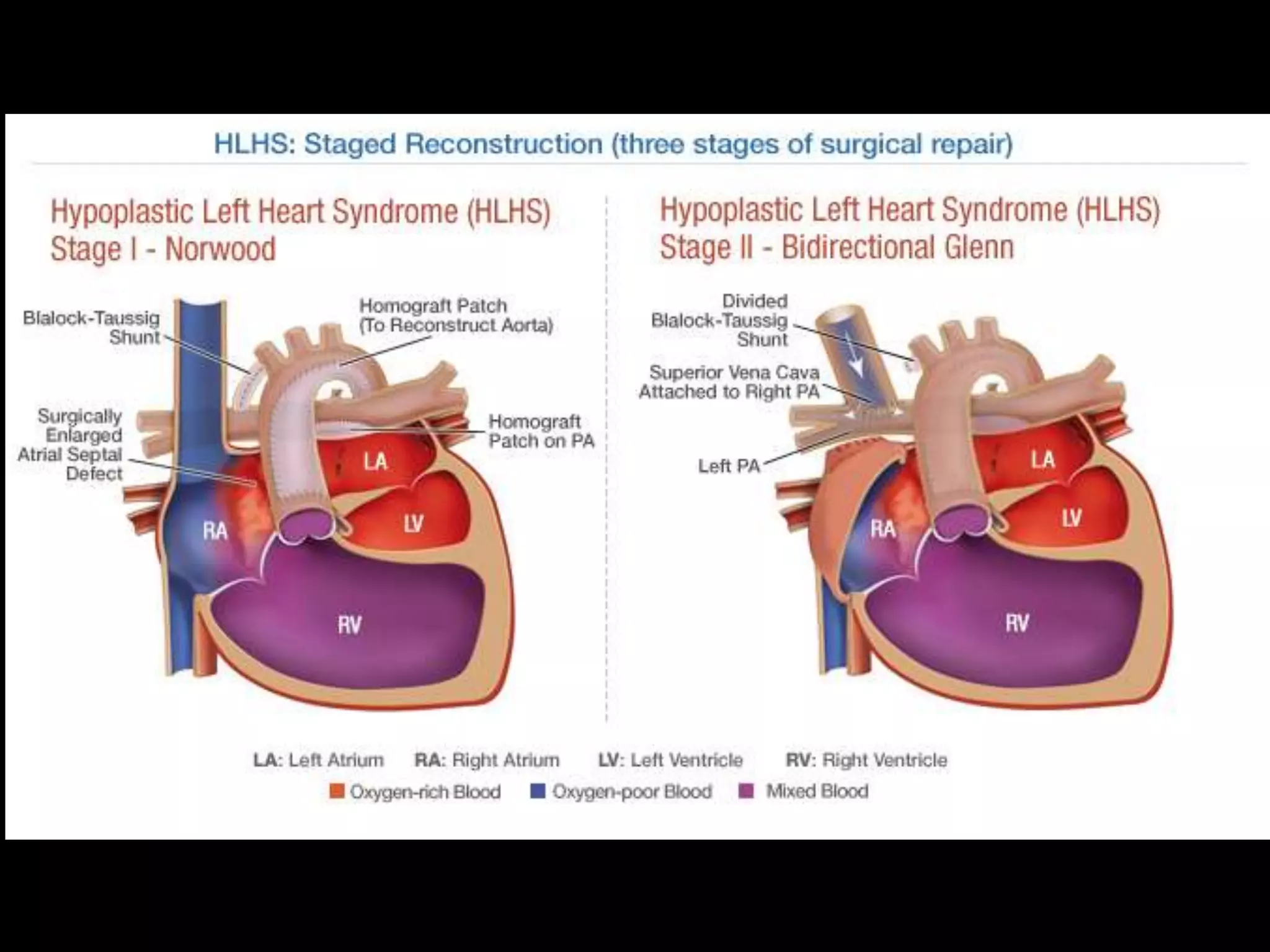
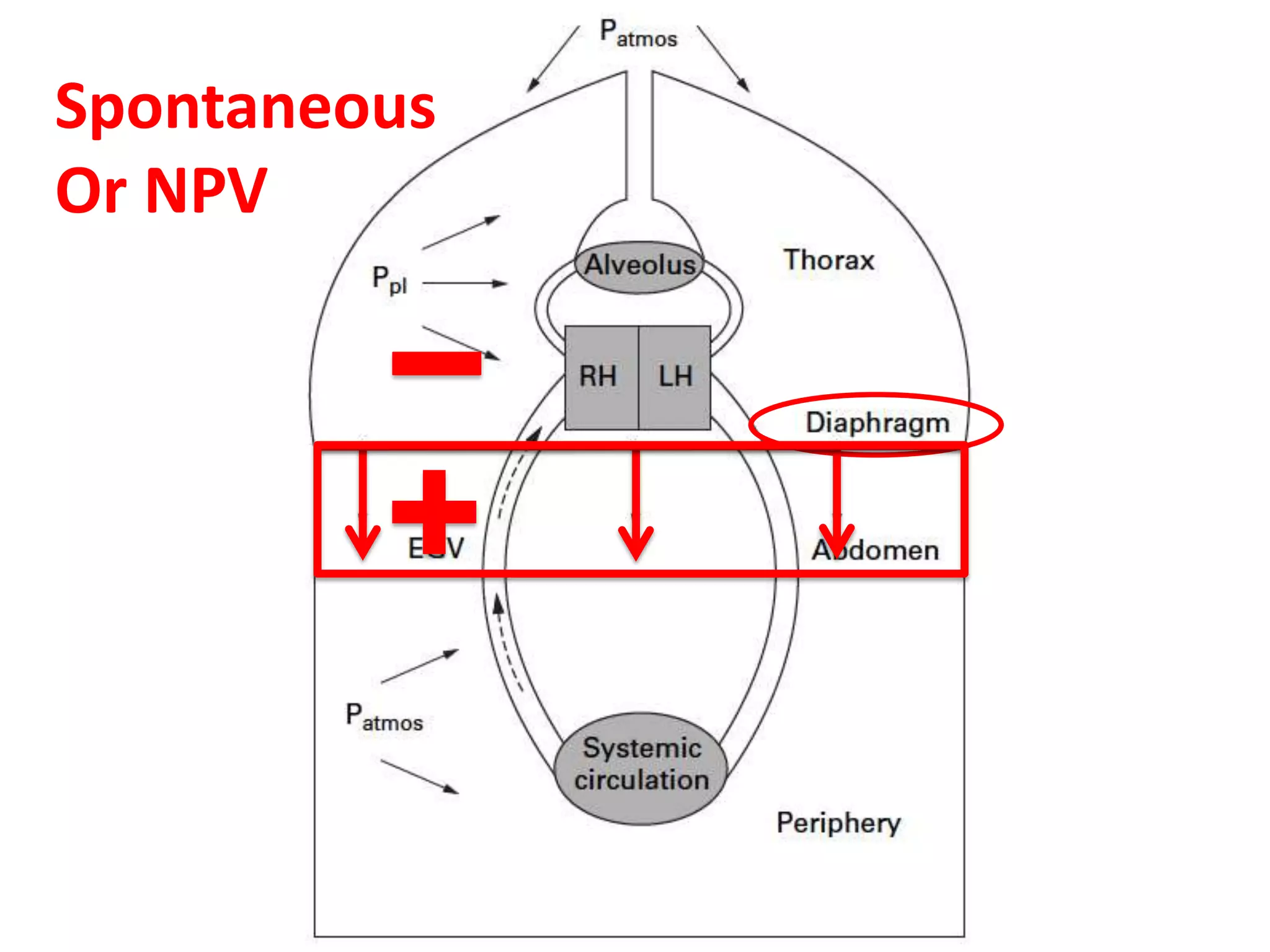
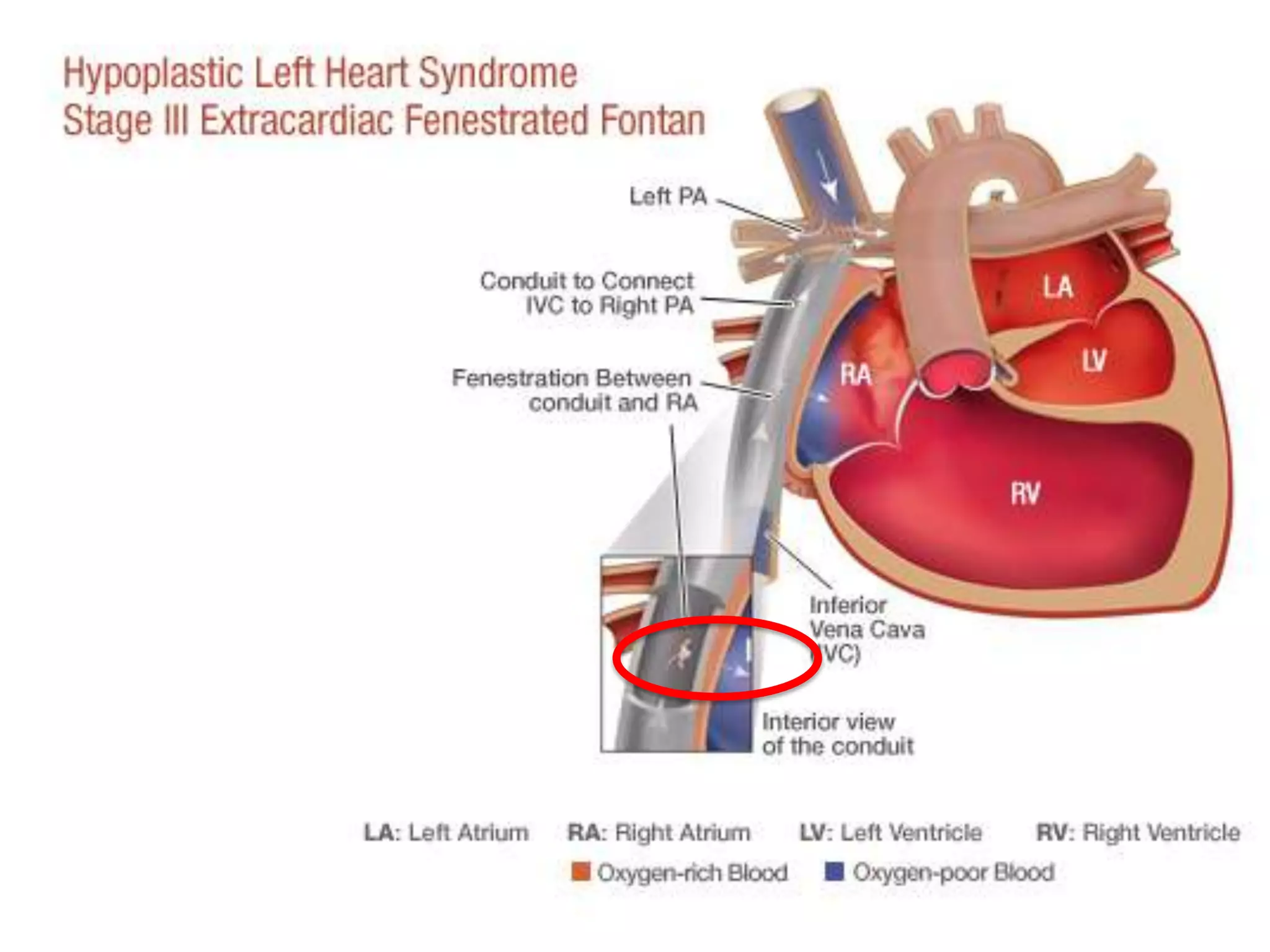
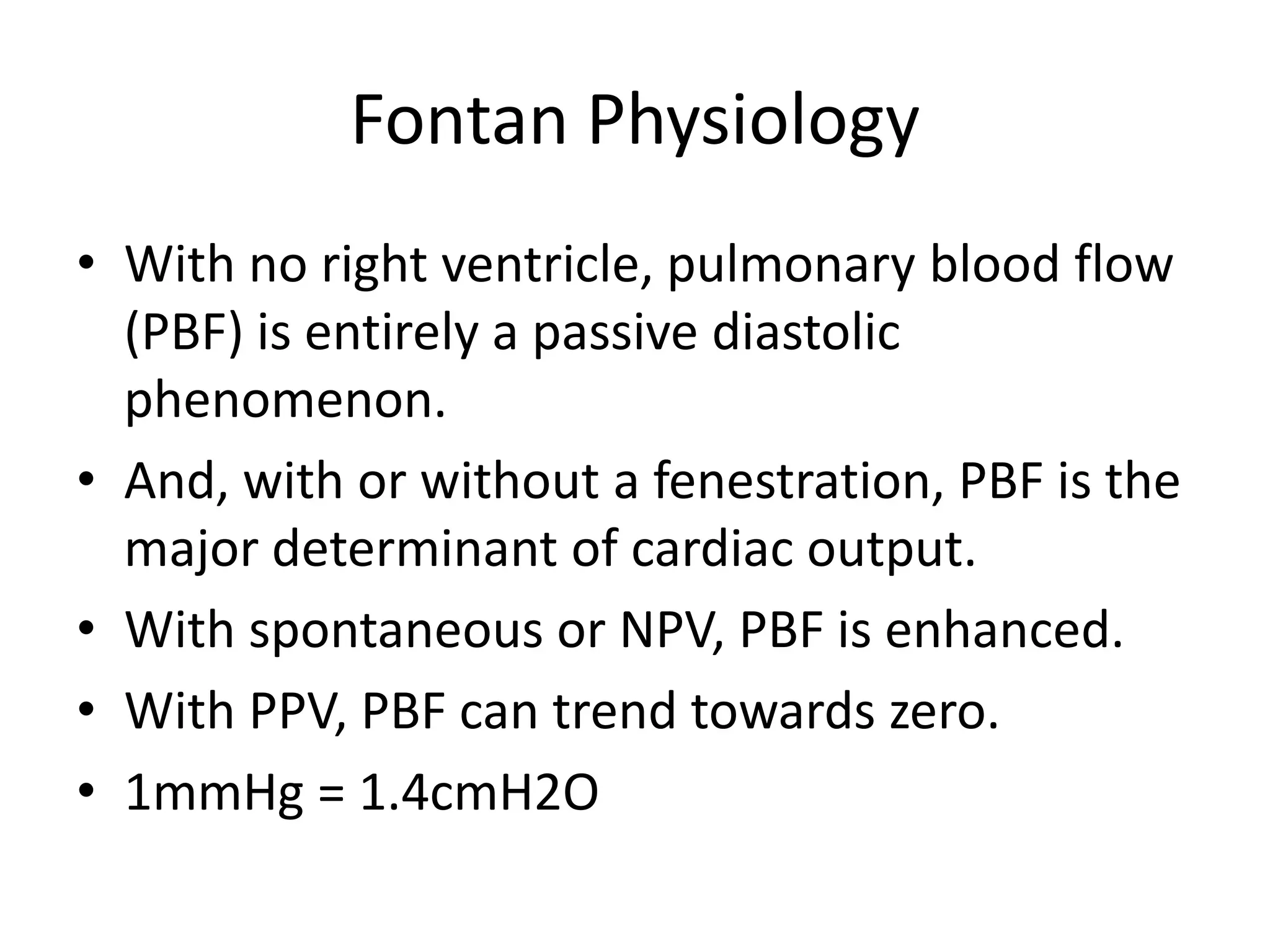
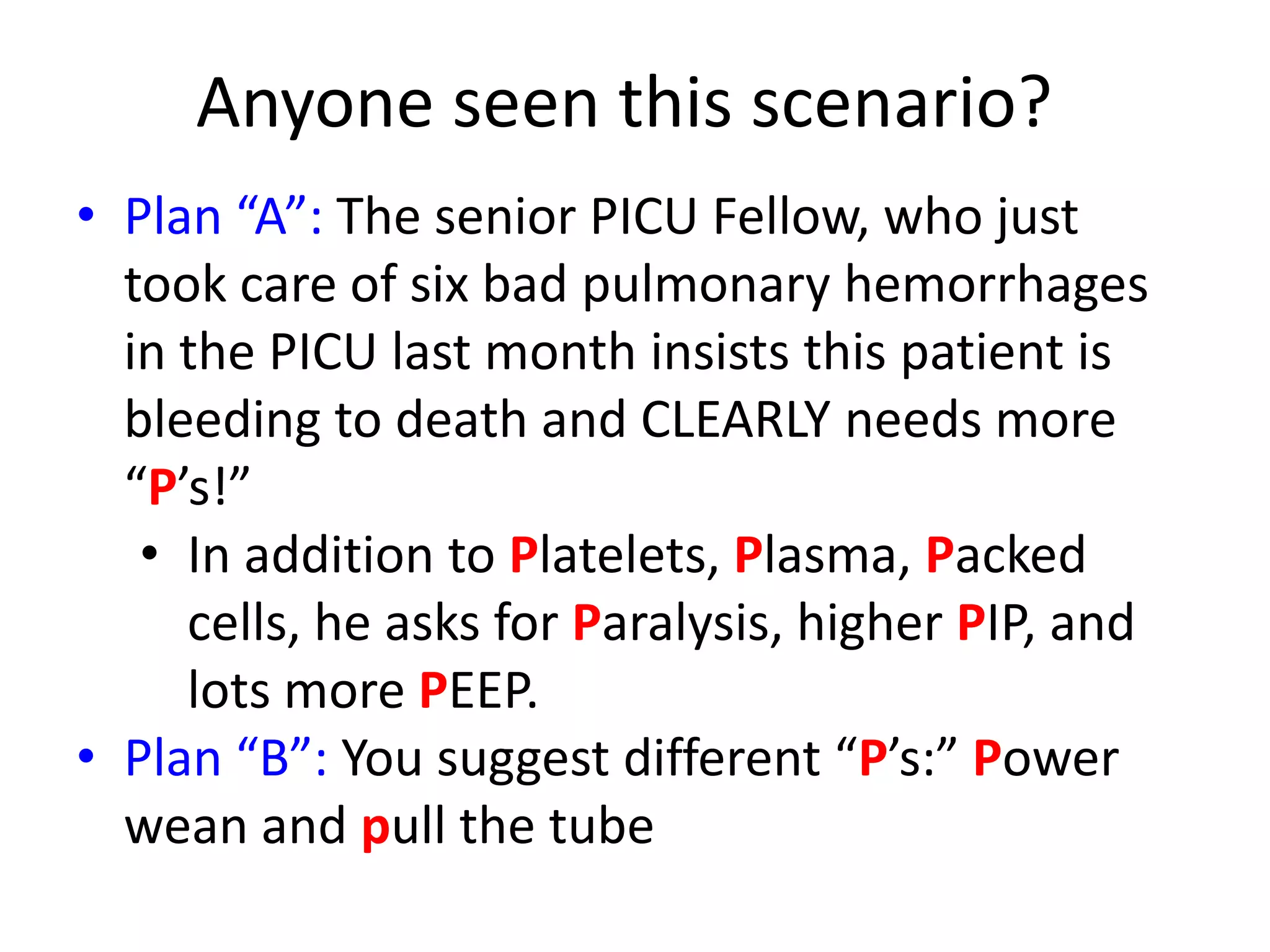
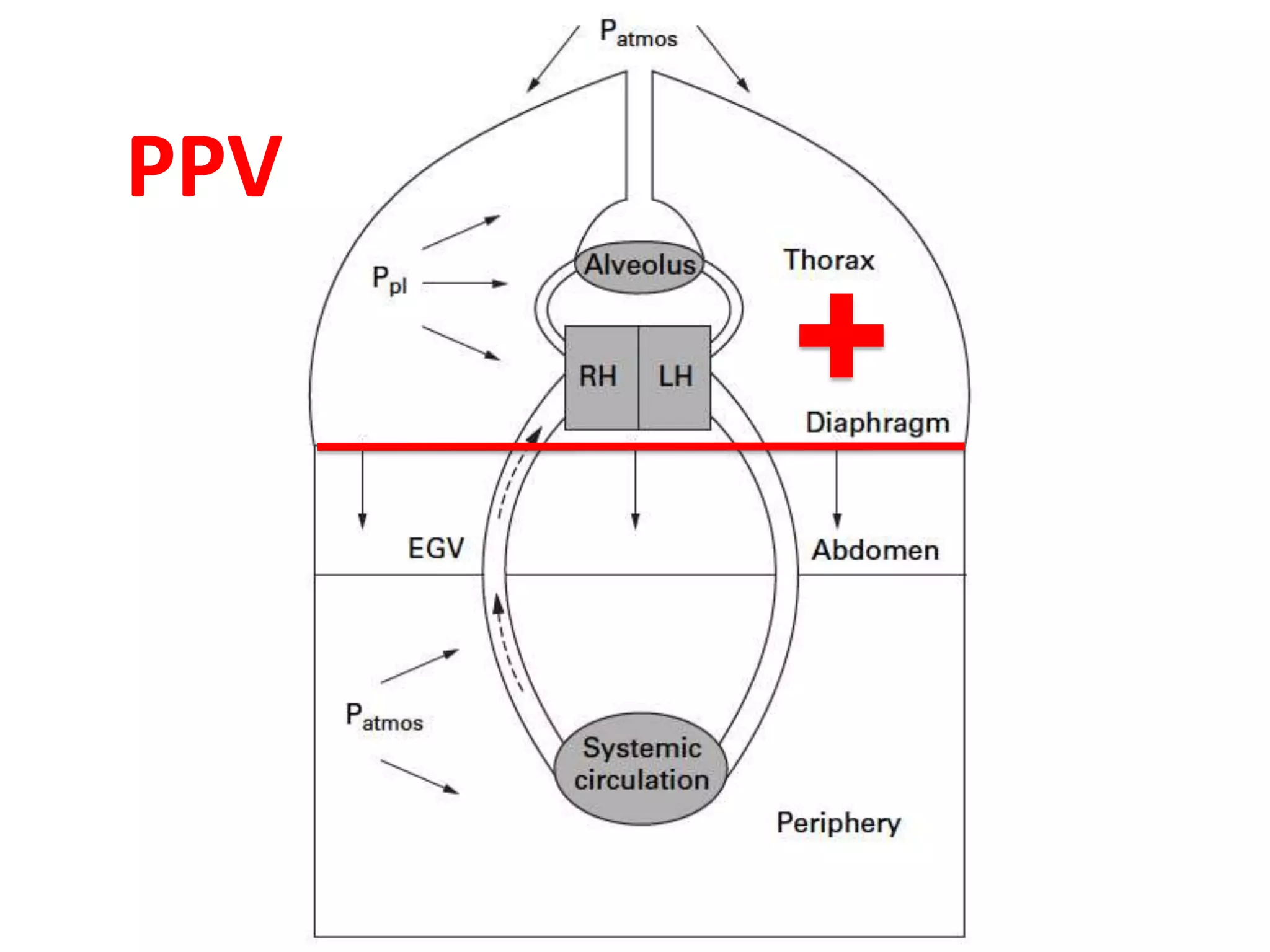
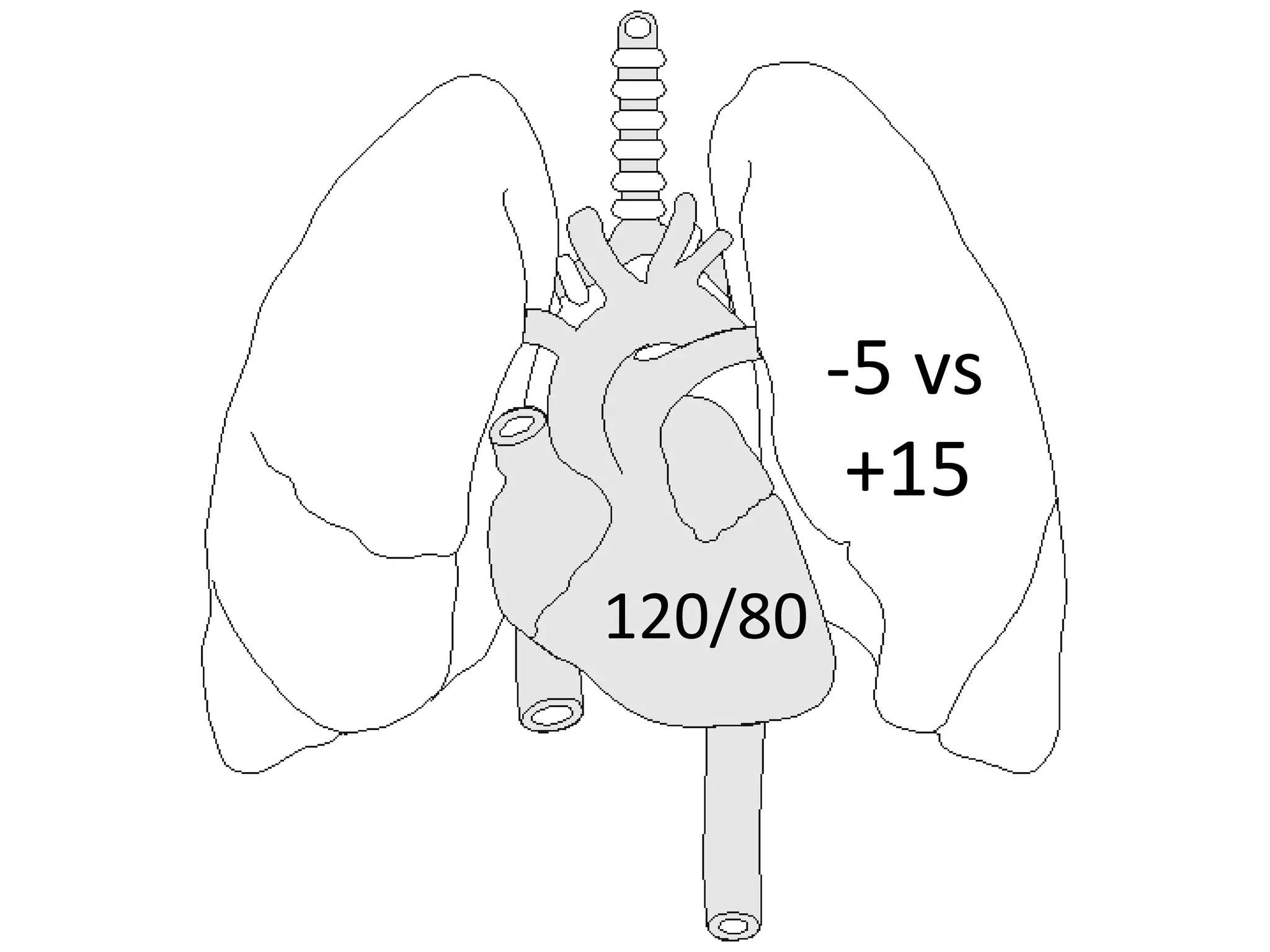
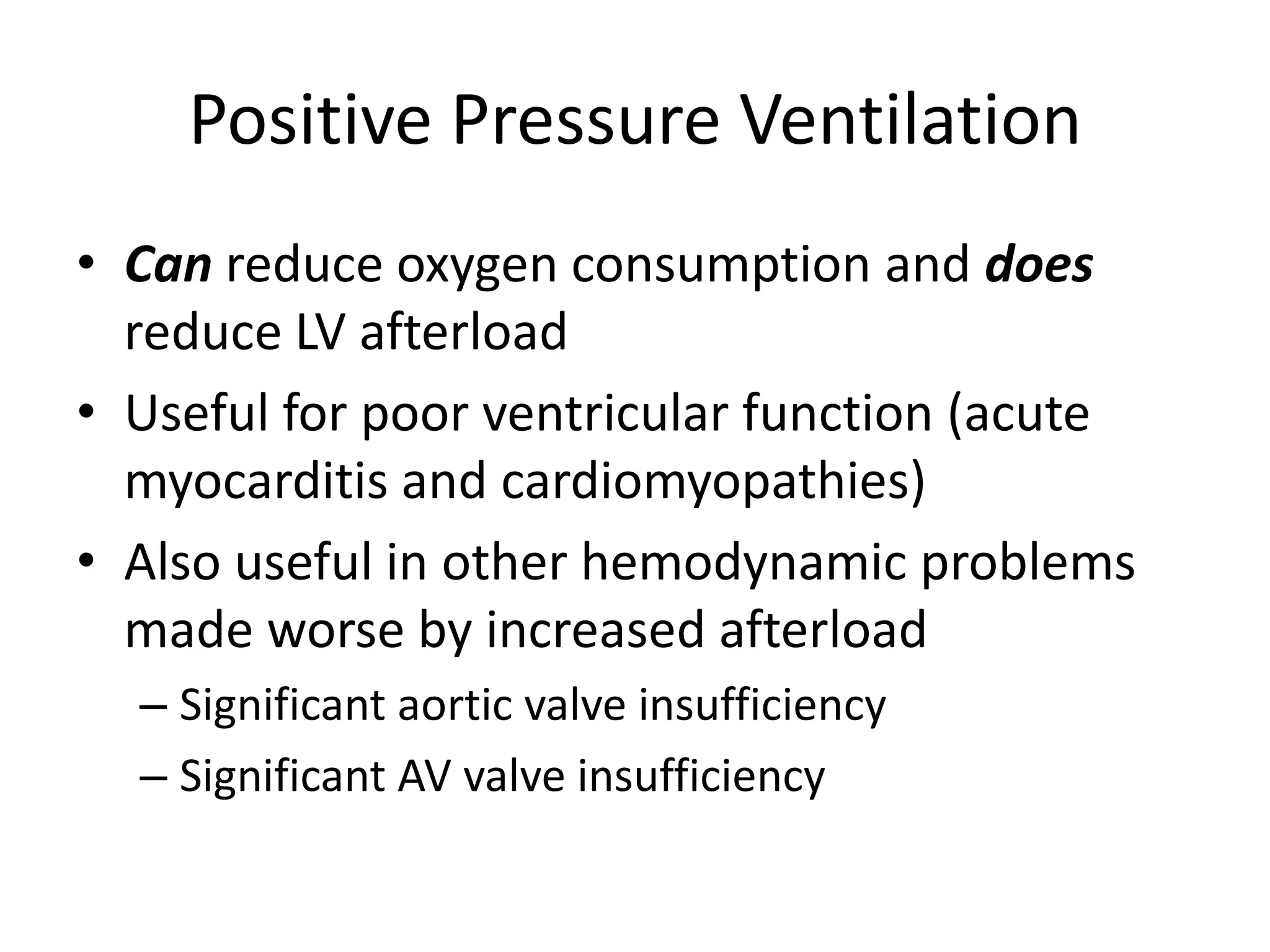
- A post-op Fontan patient is bleeding from the endotracheal tube after surgery and needs to be managed. One fellow recommends increasing ventilator support while the respiratory therapist suggests extubating.
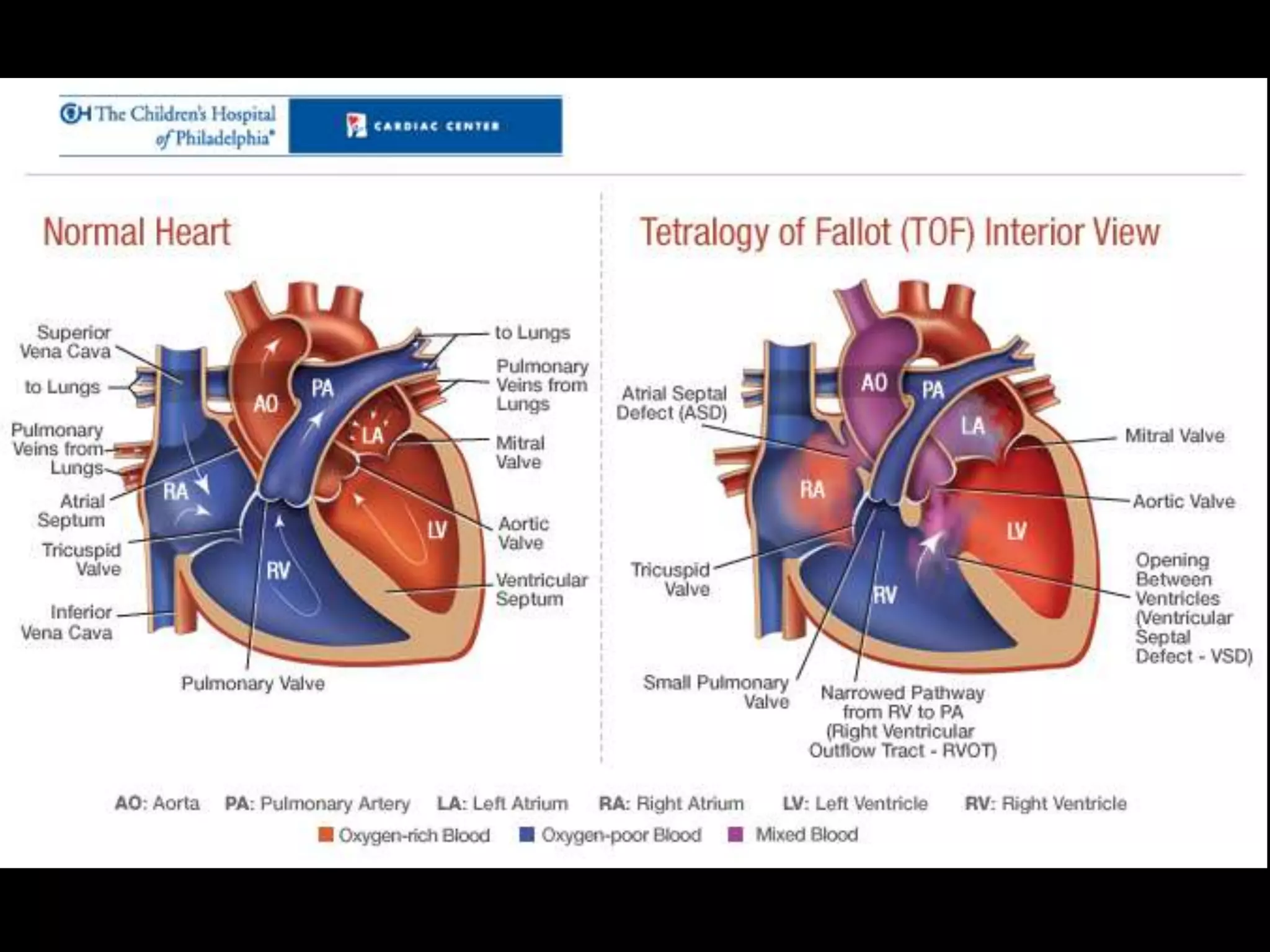
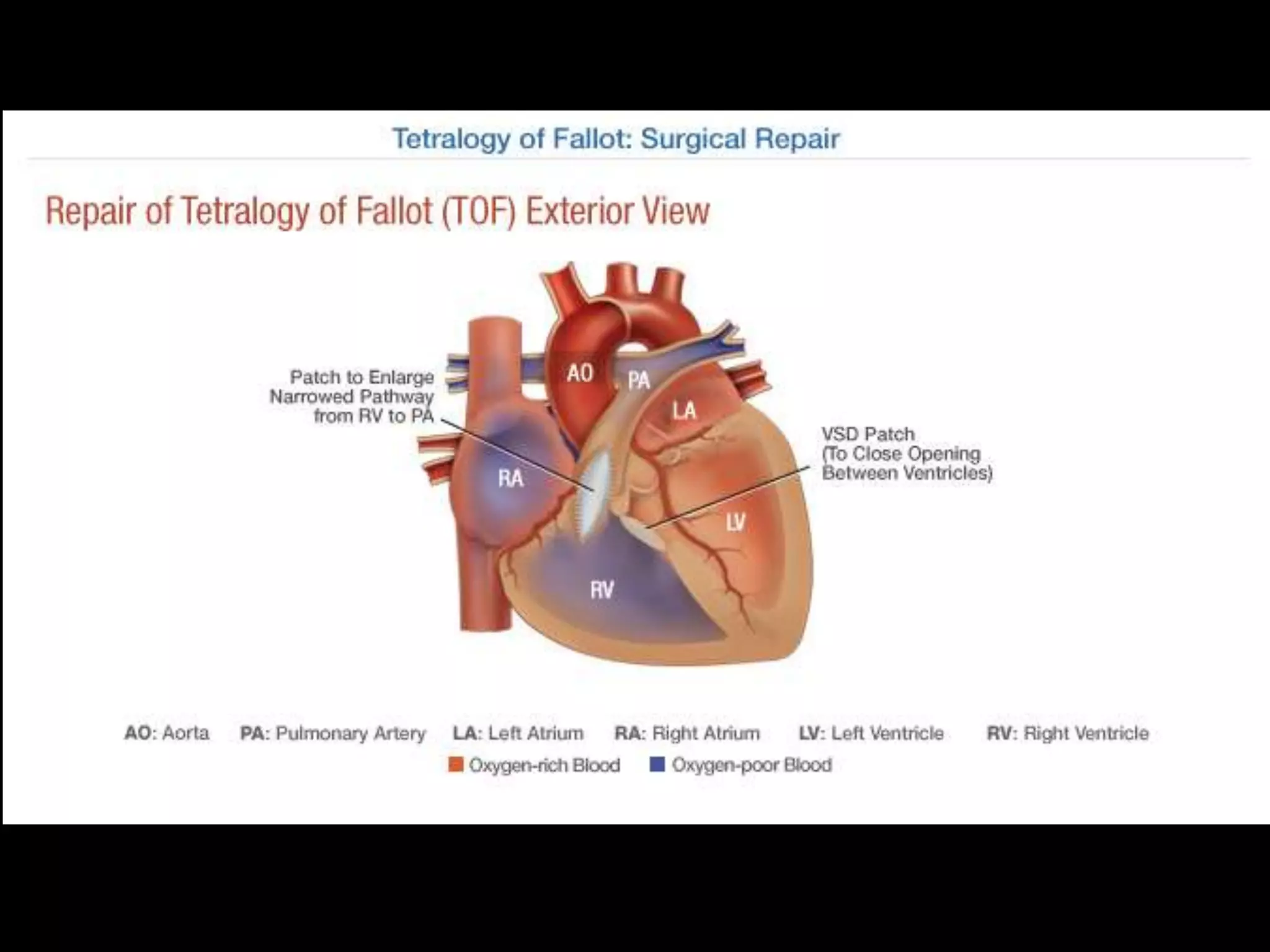
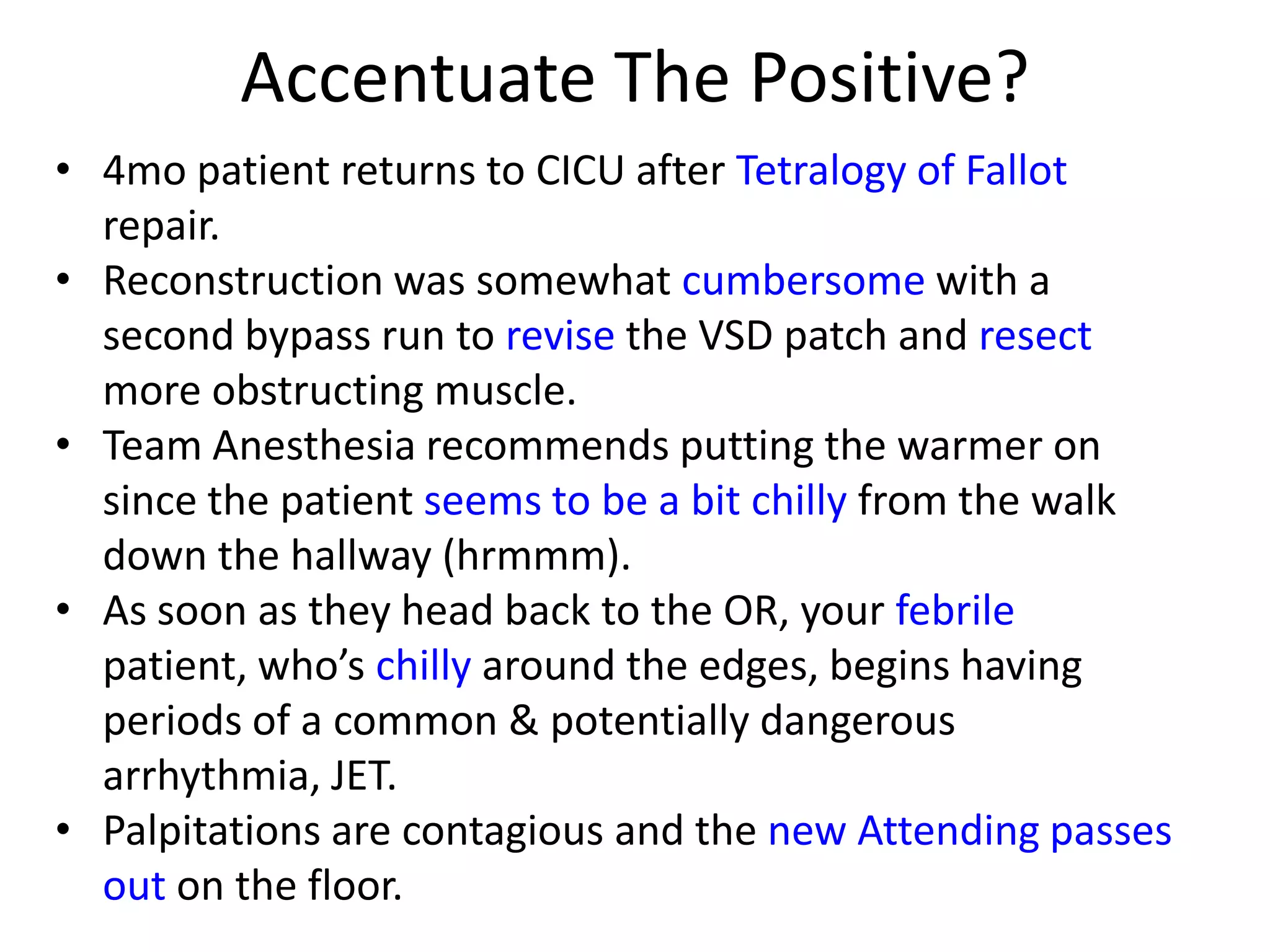
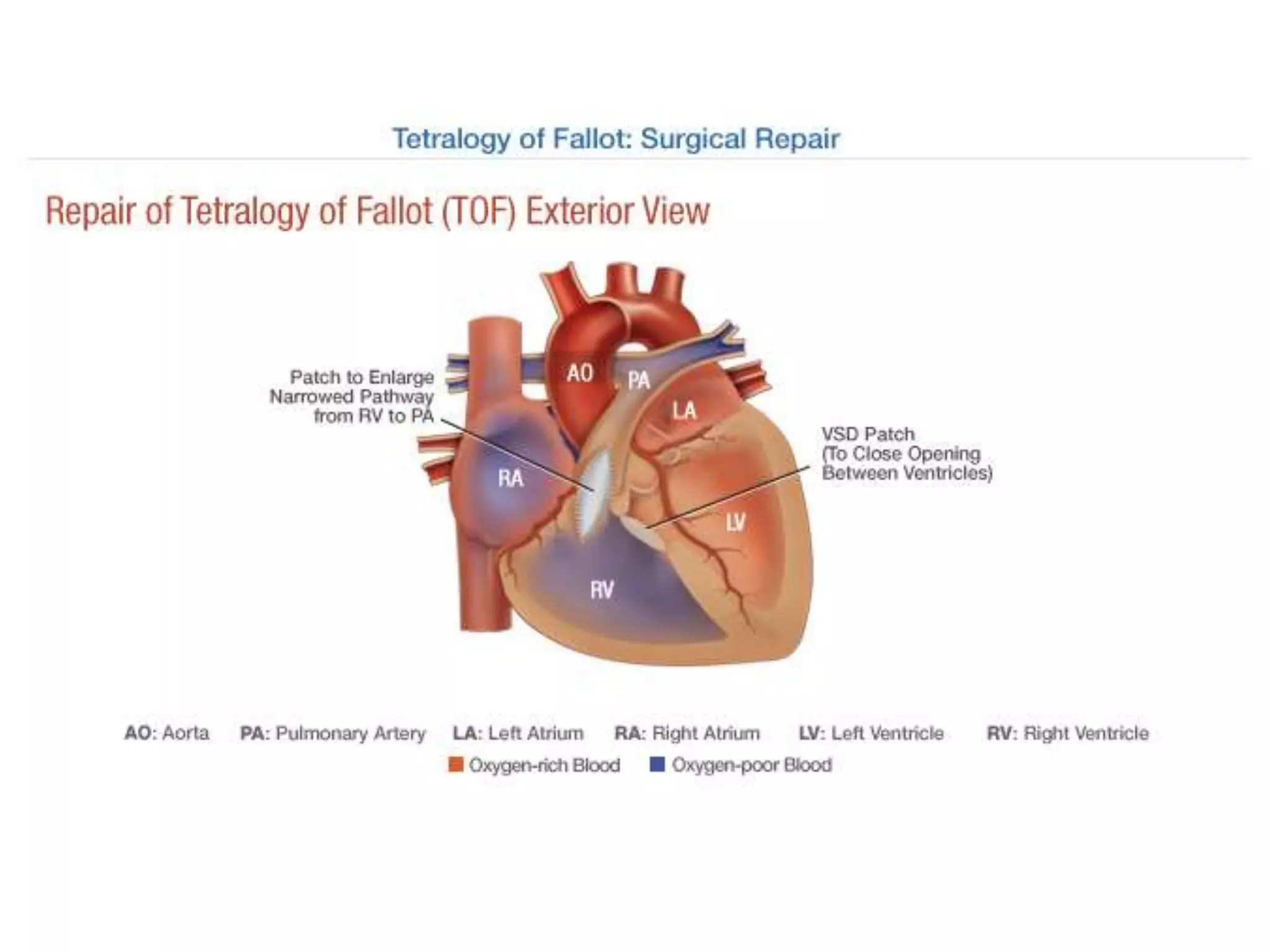
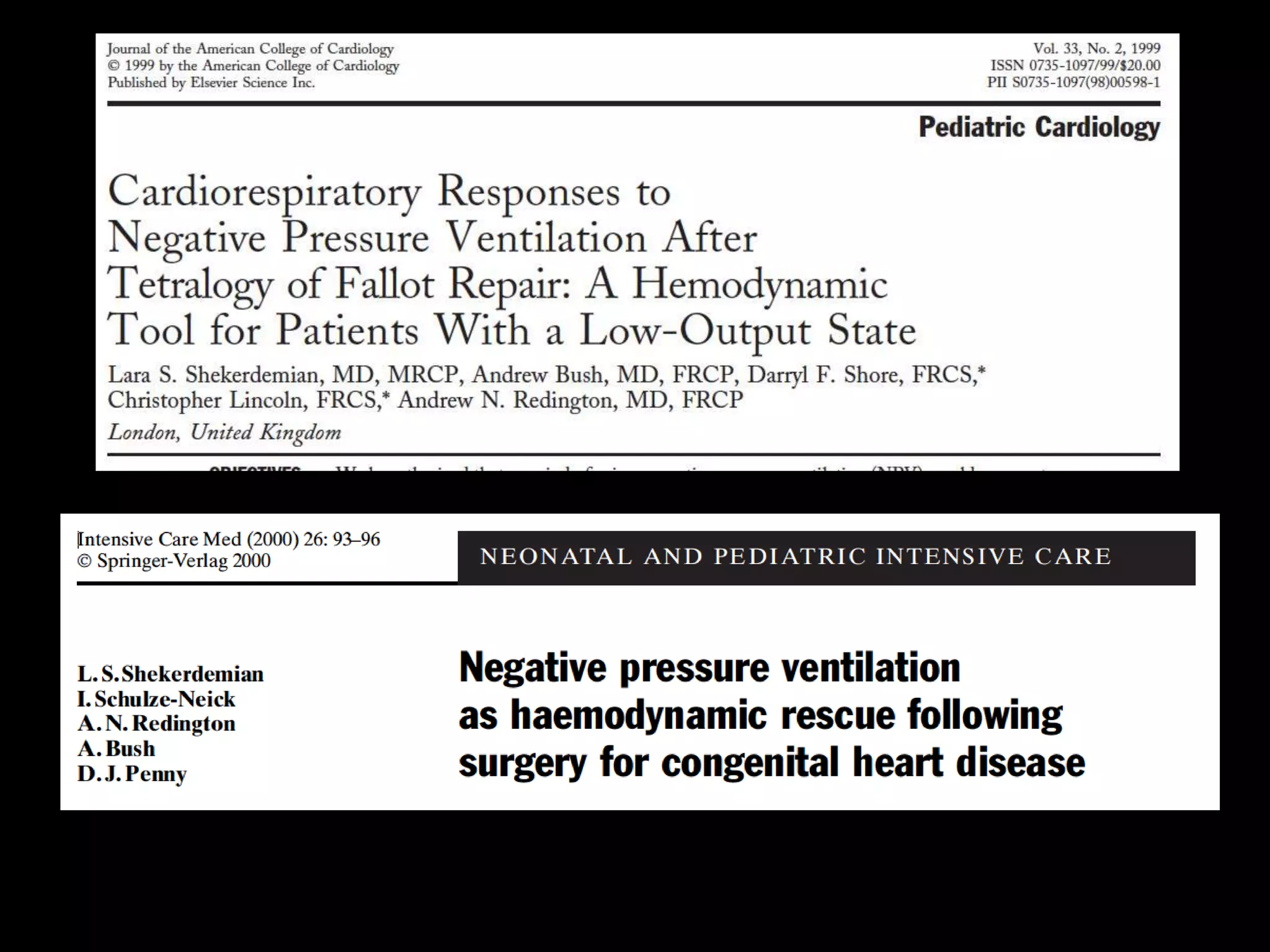
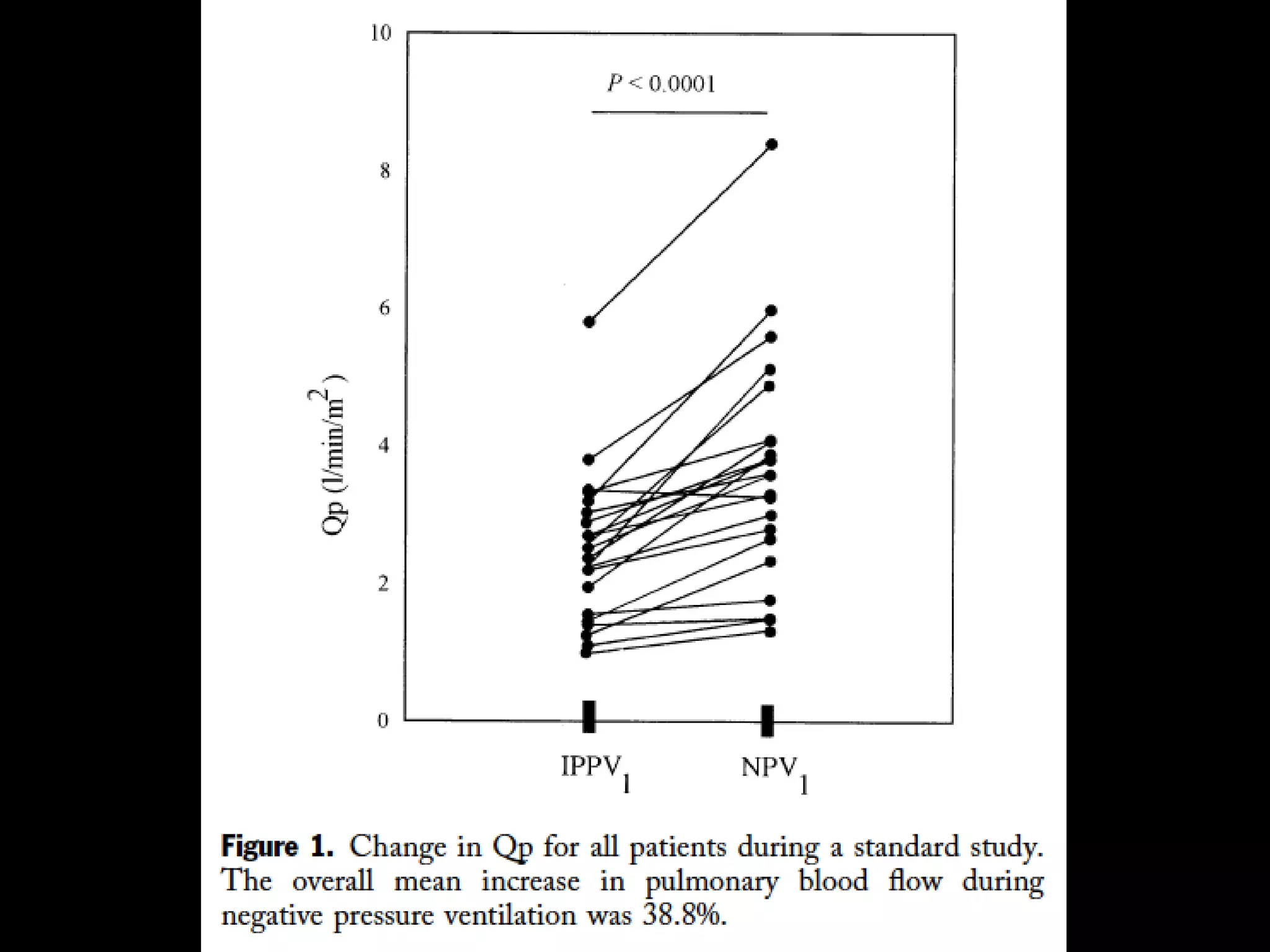
- A Tetralogy of Fallot patient becomes arrhythmic after surgery. The attending recommends interventions like fluid boluses but the respiratory therapist suggests a different approach.
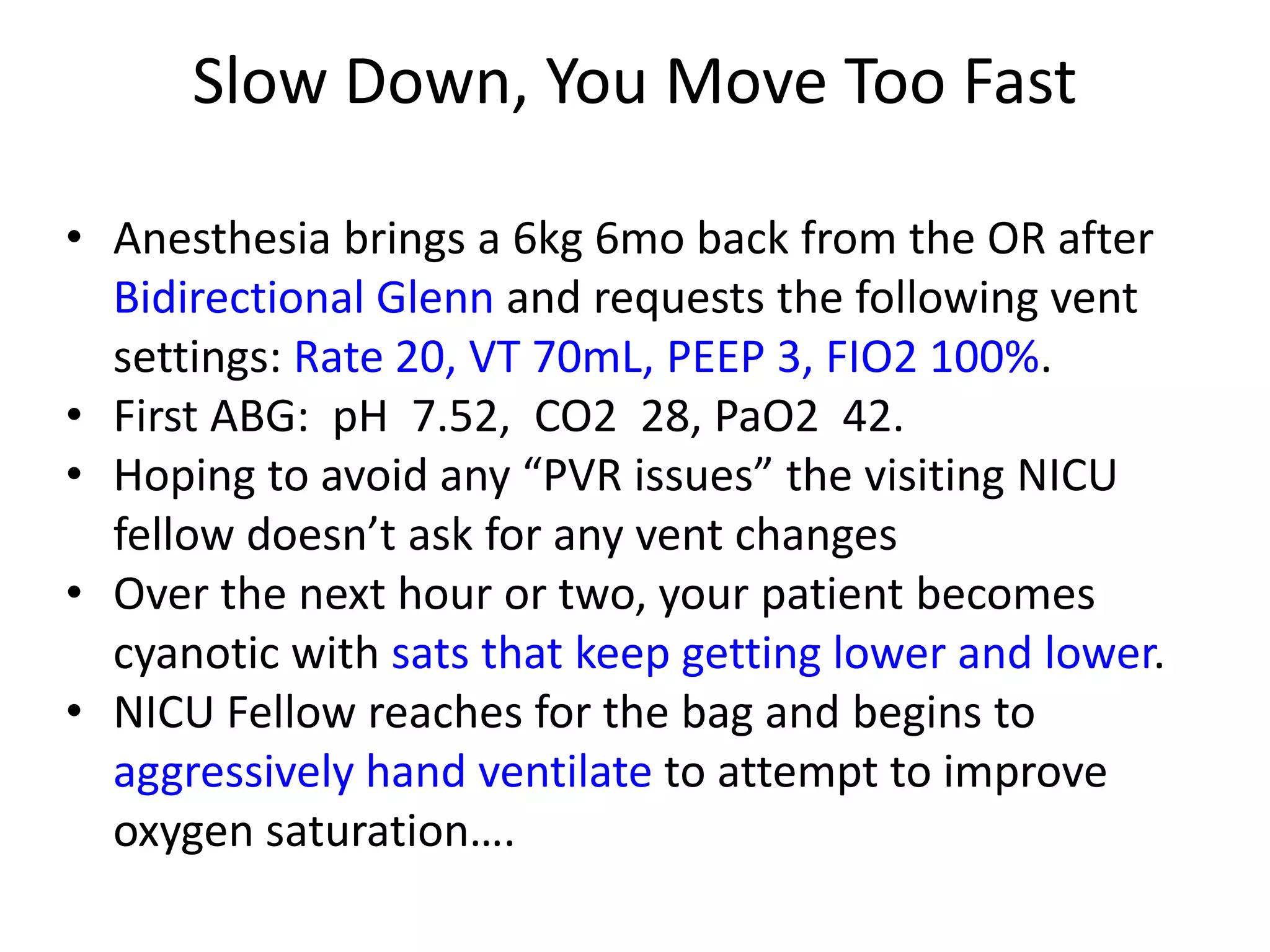
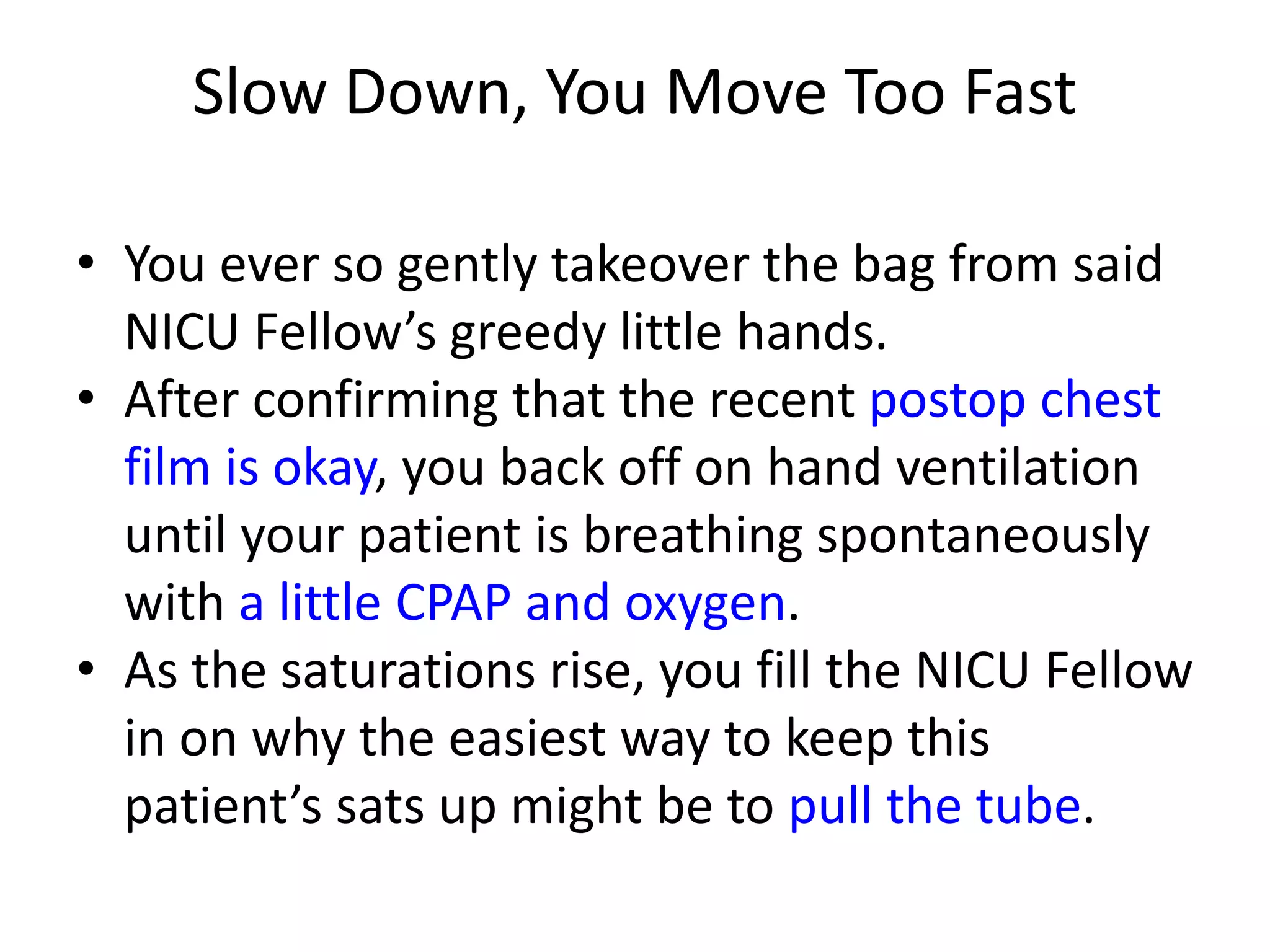
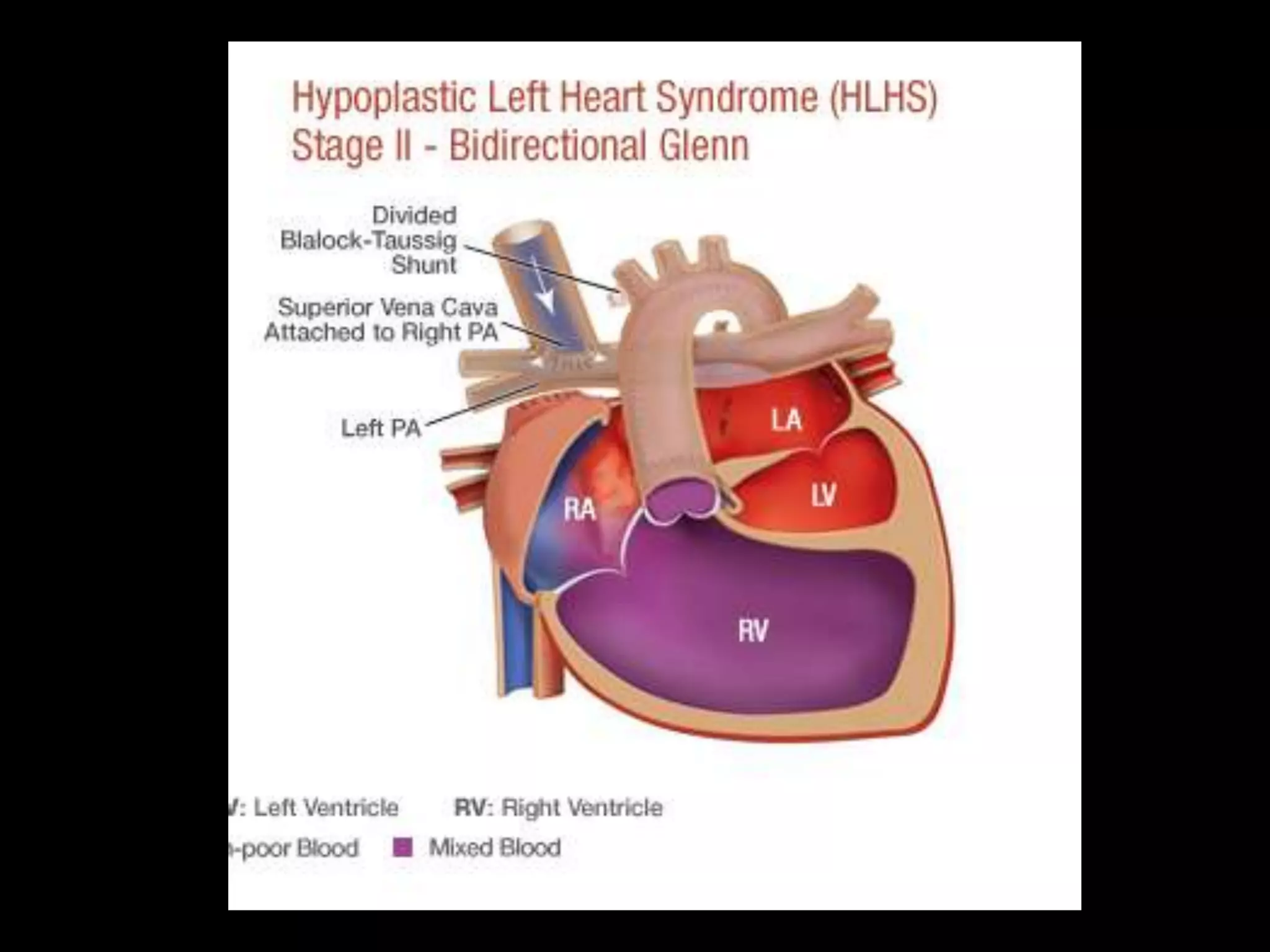
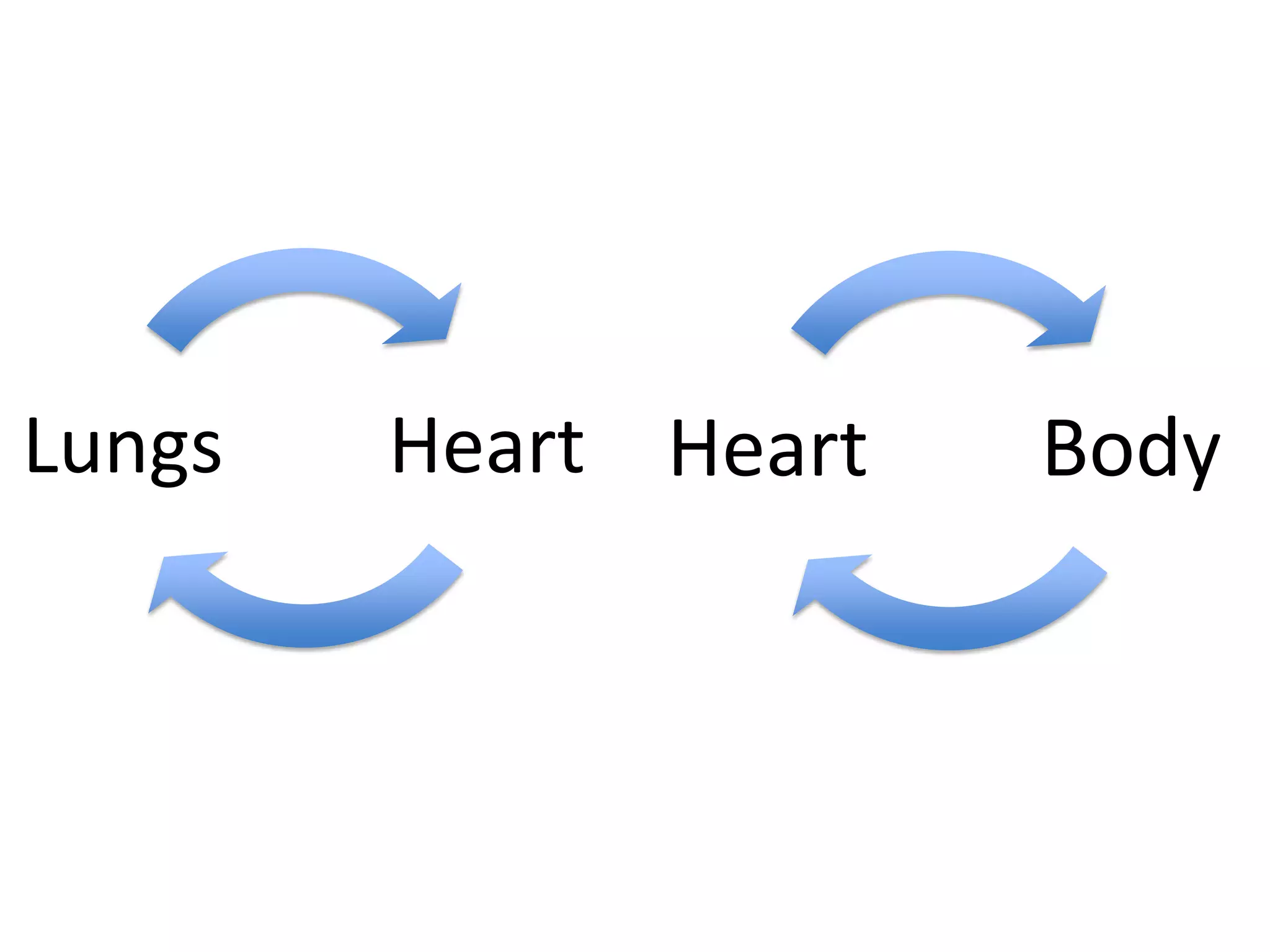
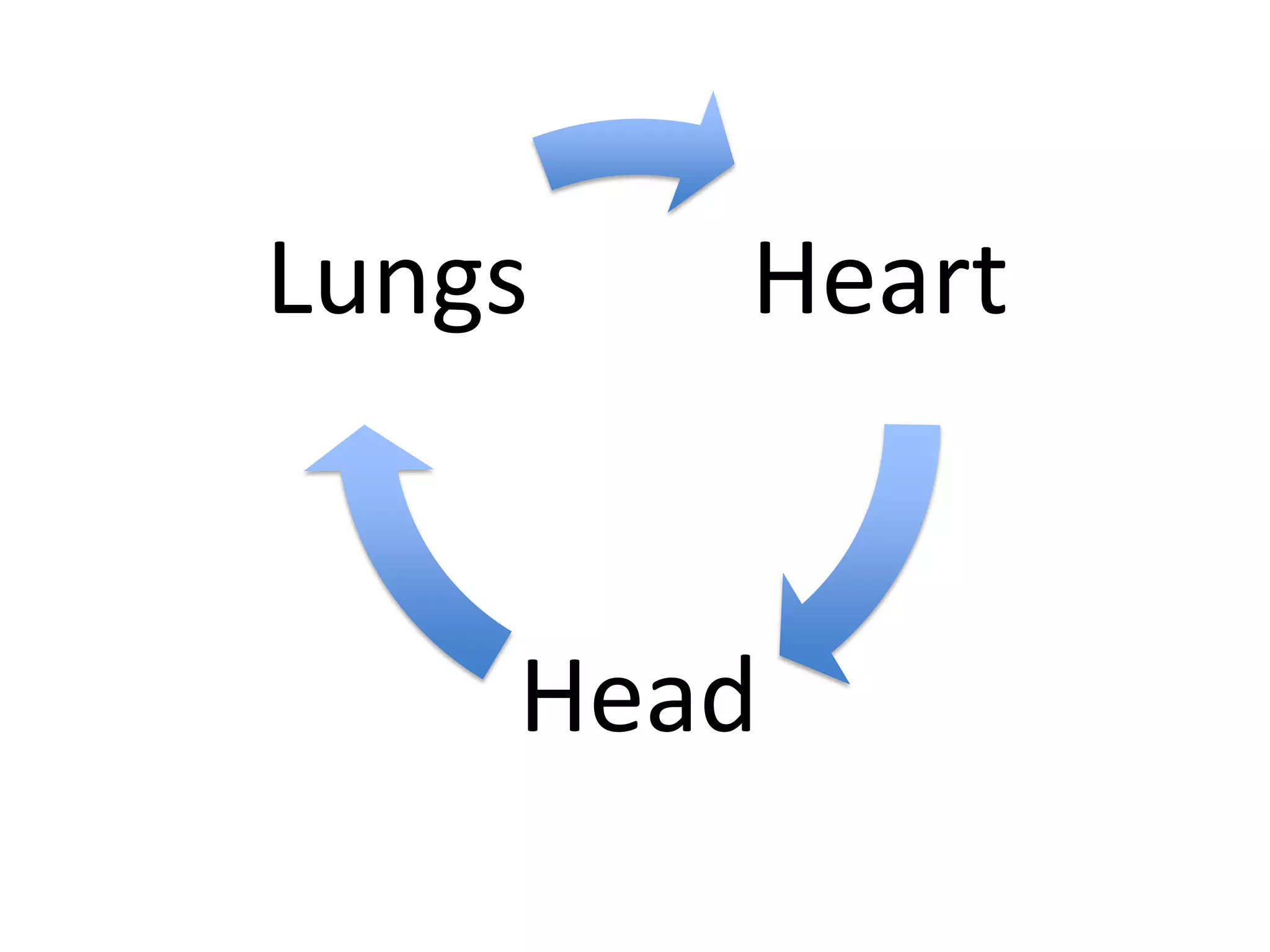
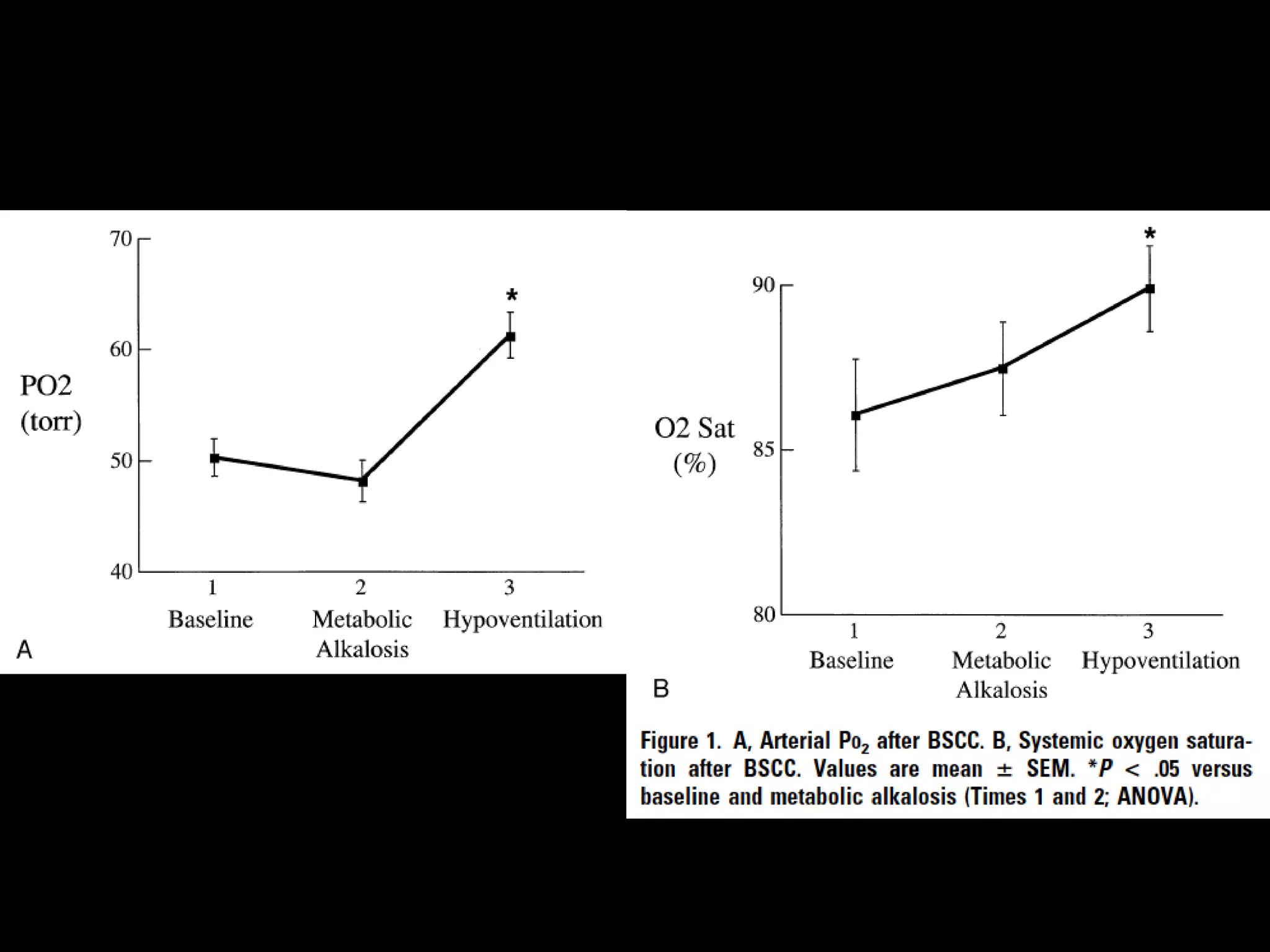
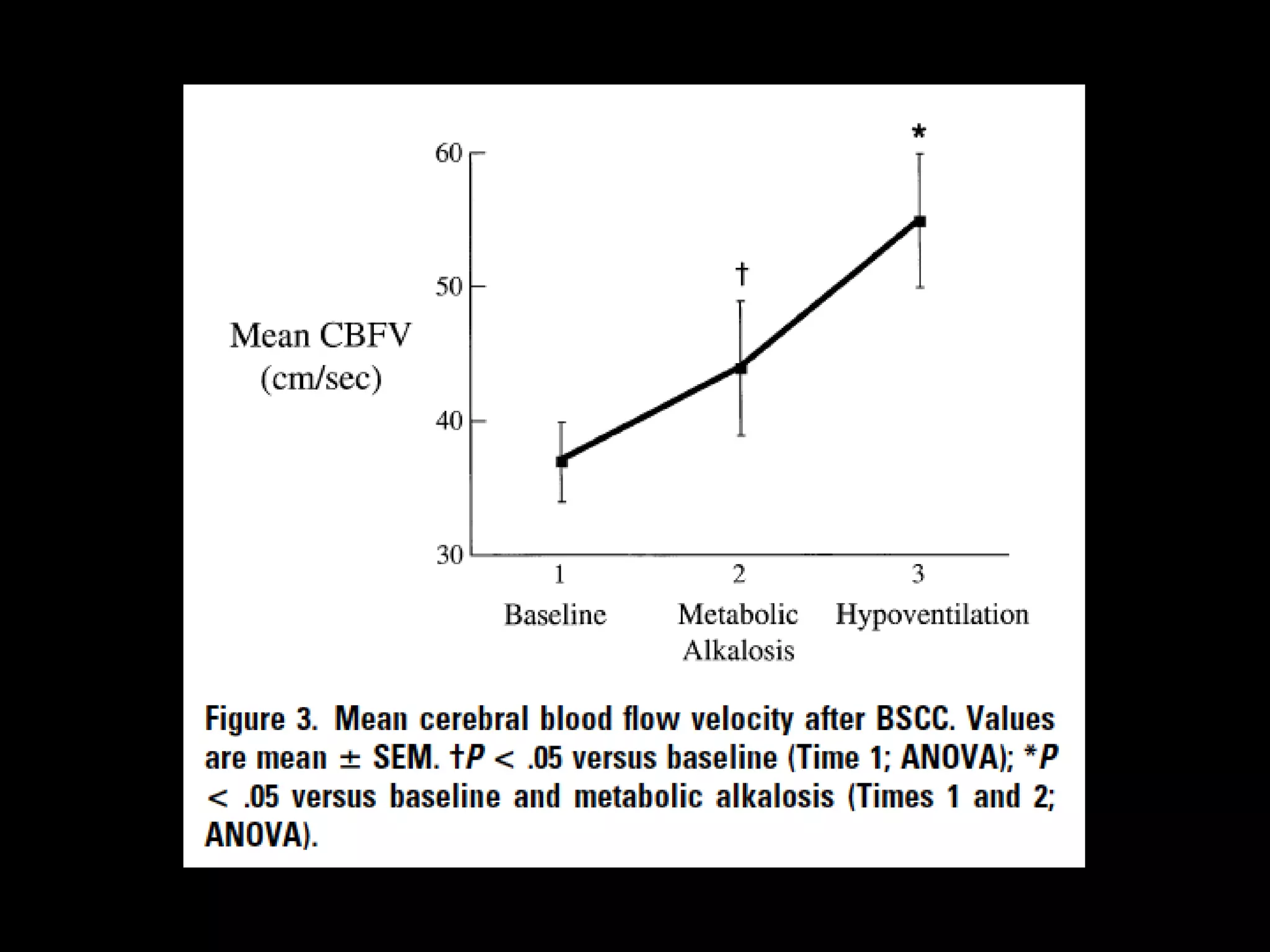
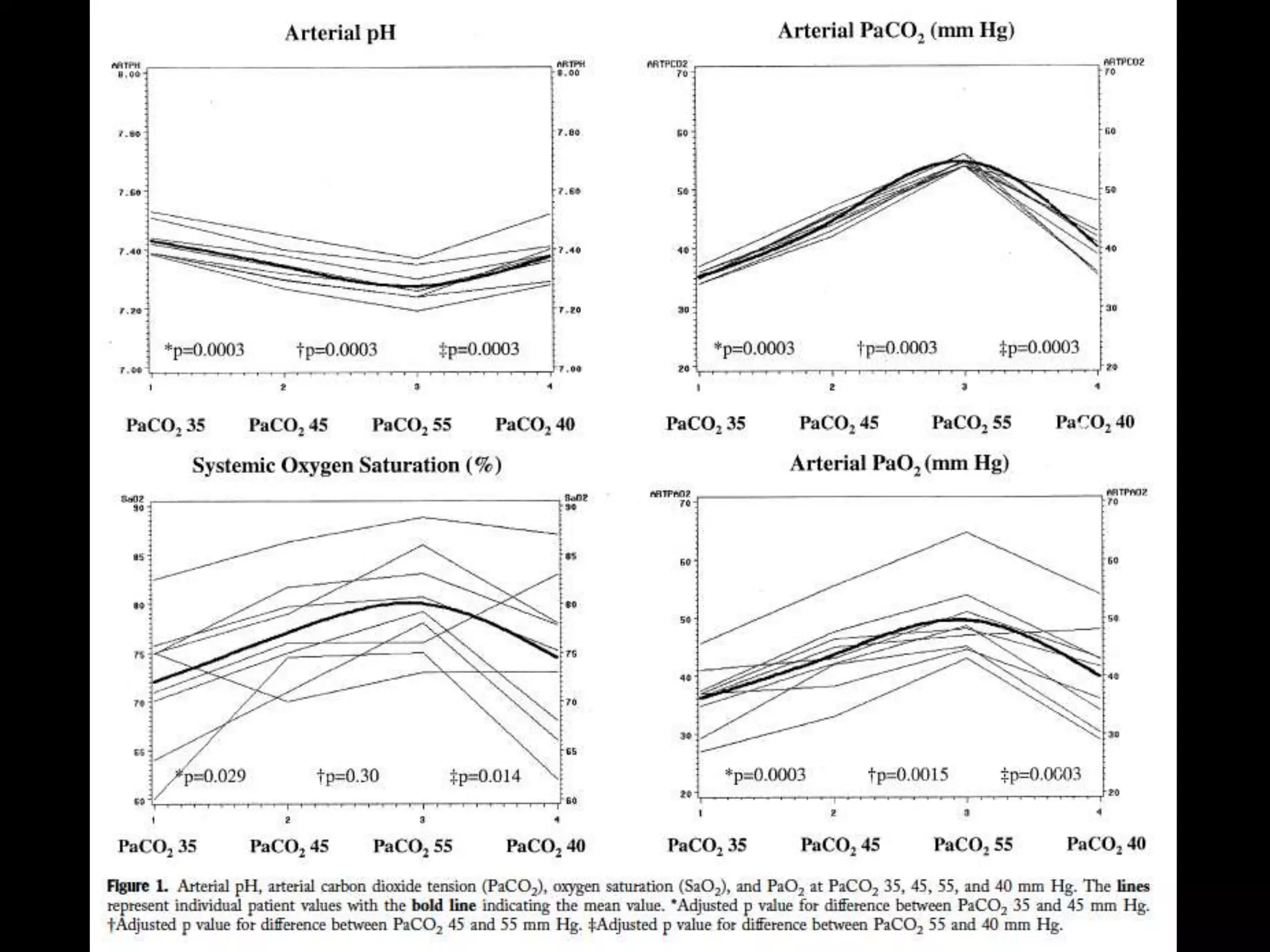
- A child returns from Glenn surgery with low oxygen levels. The fellow increases bagging but the respiratory therapist slows ventilation and suggests extubating may help.