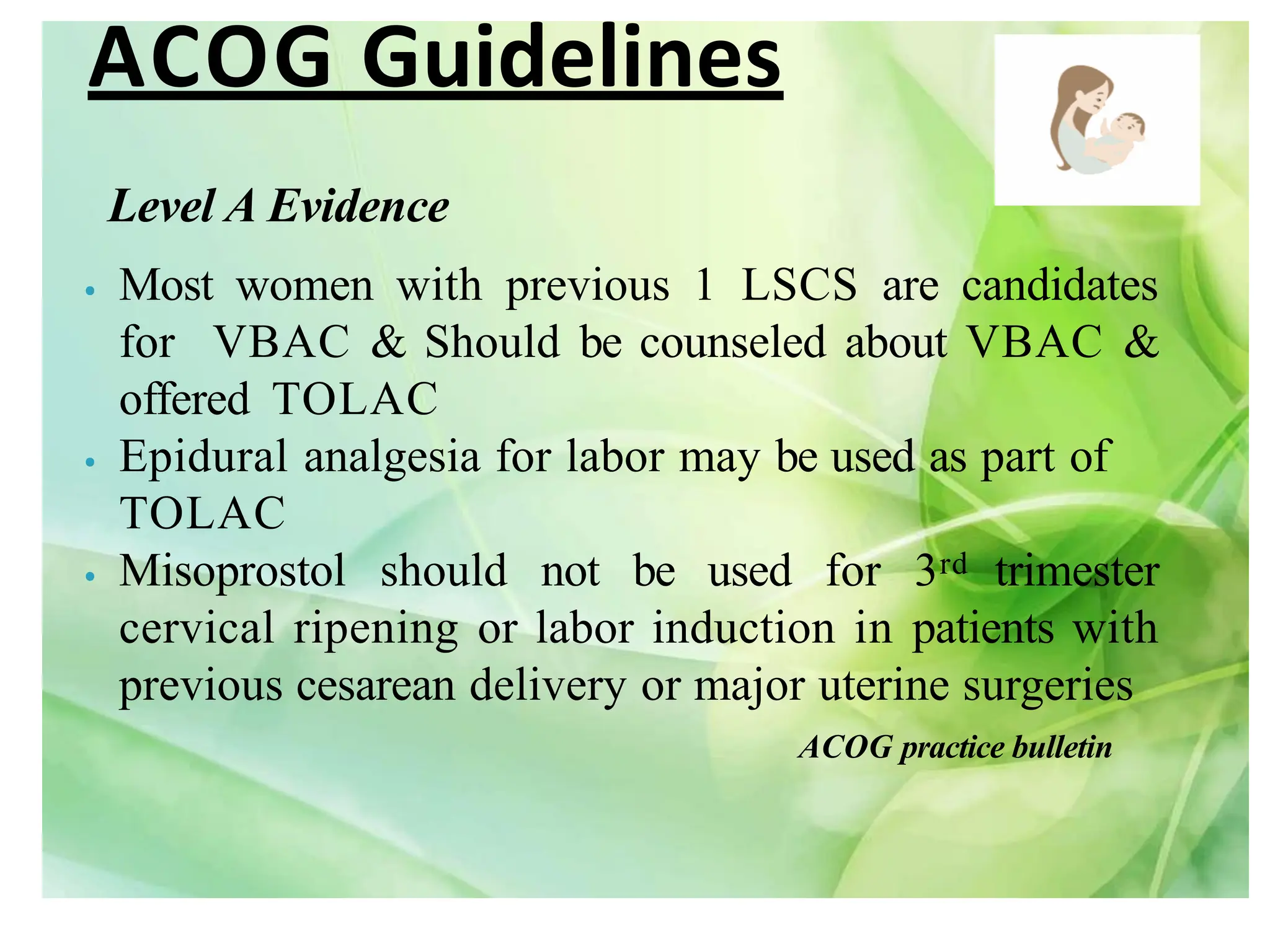
The document discusses vaginal birth after cesarean section (VBAC), emphasizing that many women with previous cesarean deliveries can safely attempt VBAC. It outlines candidate selection criteria, success rates, risks, and the importance of appropriate prenatal care and planning. Current guidelines and studies support the notion that, with proper counseling and medical support, VBAC is a viable option for most women after a prior cesarean delivery.



































![CONCLUSION
There is a consensus (National Institute for Health and Care
Excellence [NICE], Royal College of Obstetricians and
Gynaecologists [RCOG], American College of Obstetricians and
Gynecologists [ACOG]/ National Institutes of Health [NIH], that
planned VBAC is a clinically safe choice for the majority of women
with a single previous lower segment caesarean delivery. Such a
strategy will at least limit any escalation of the caesarean delivery
rate and maternal morbidity associated with multiple caesarean](https://image.slidesharecdn.com/vaginalbirthaftercesareansection-240327052733-45fa2acd/75/Vaginal-Birth-after-Cesarean-Section-pdf-41-2048.jpg)
![REFERENCES
• RCOG Birth After Previous Caesarean Birth, Green-top
Guideline No. 45 ,October 2021
• Vaginal birth After Cesarean Delivery In: The management of labor, 3rd
edition, India Universities Press.
• Varun N, Nigam A, Gupta N, Mazhari F, Kashyap V. Vaginal birth after
cesarean score for the prediction of successful vaginal birth after cesarean
section – A prospective observational study. Indian J Med Spec [serial online]
2023 Available from: http://www.ijms.in/text.asp?2023/14/1/15/360049
• Mohamed SA, Elsayed YA, Ghonemy GE, Sharaf MF. Incidence and outcome
of vaginal birth after cesarean among women receiving counseling at El
Manial University Hospital. Egypt,Available
from: http://www.enj.eg.net/text.asp?2020/17/2/107/320267](https://image.slidesharecdn.com/vaginalbirthaftercesareansection-240327052733-45fa2acd/75/Vaginal-Birth-after-Cesarean-Section-pdf-42-2048.jpg)
