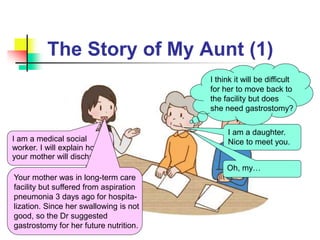
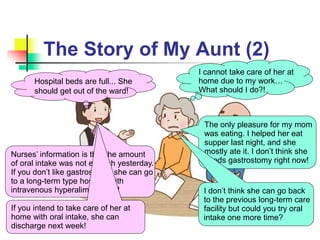
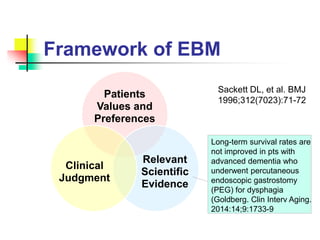
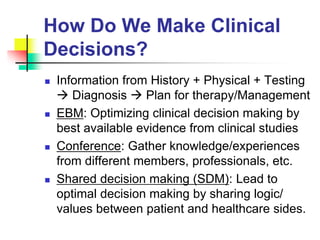
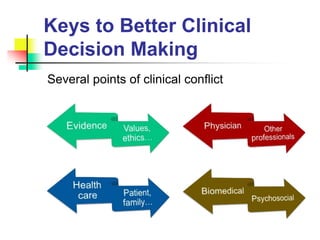
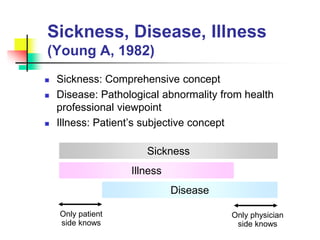
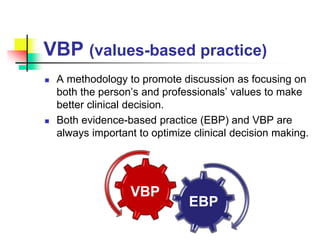
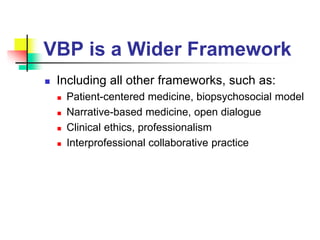
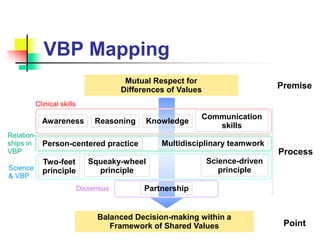
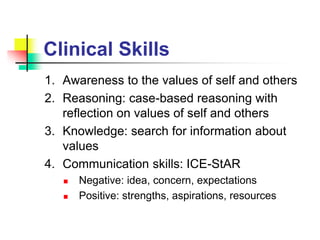
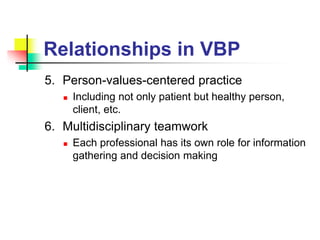
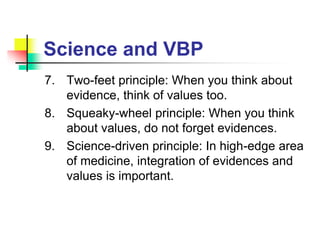
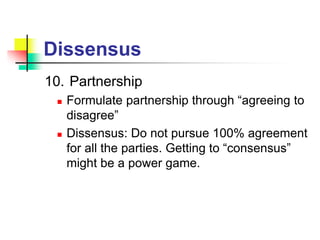
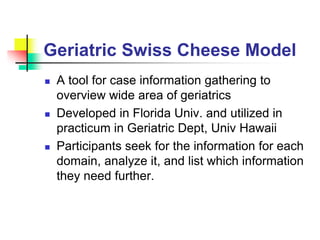
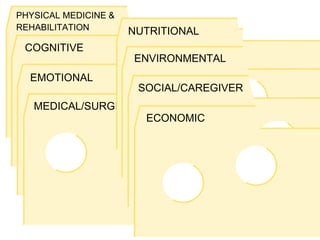
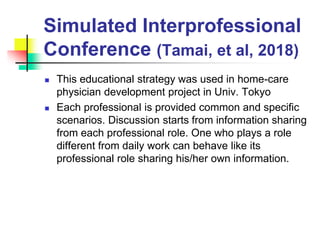
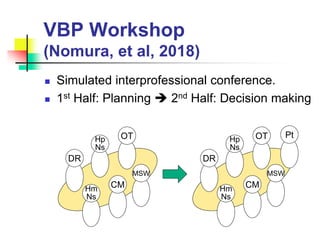
This document discusses values-based practice (VBP) in clinical decision making. It provides an overview of VBP, explaining that VBP focuses on both the patient's values and the professionals' values to make optimal decisions. It also discusses how VBP integrates with evidence-based practice and relates to concepts like patient-centered care. The document outlines several skills needed for VBP, such as awareness of values, reasoning that incorporates values, and communication skills. It proposes some principles for integrating science and values in clinical practice. Finally, it presents some models for teaching VBP, such as using case discussions and simulated interprofessional conferences.