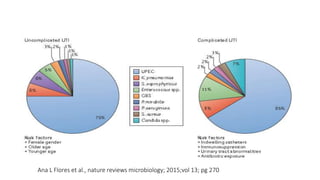
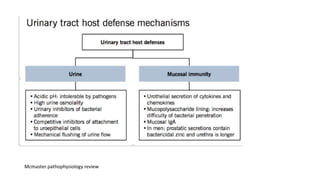
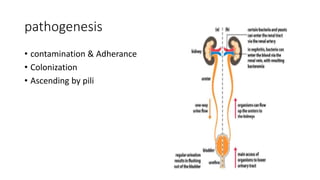
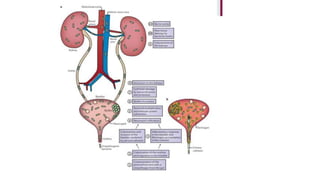
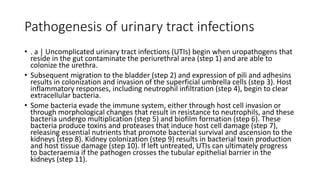
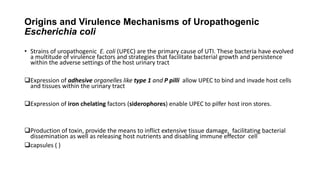
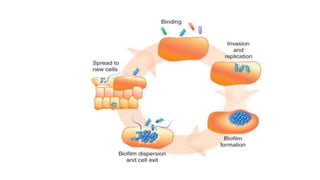
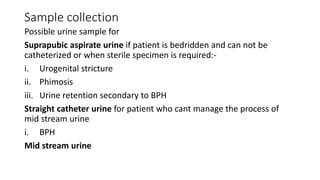
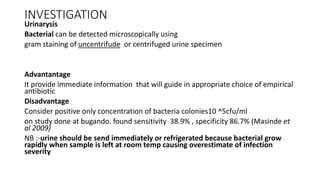
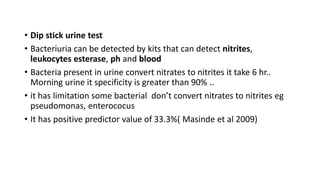
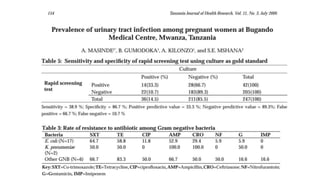
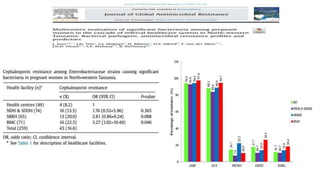
The document provides a comprehensive overview of urinary tract infections (UTIs), including their anatomy, epidemiology, risk factors, classification, clinical presentation, and treatment. It highlights common pathogens, especially Escherichia coli, and discusses the significant impact of UTIs on pregnant women, along with prevention strategies. Additionally, the document emphasizes the challenge of multidrug resistance and the importance of improved management approaches in clinical settings.