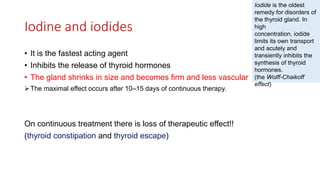
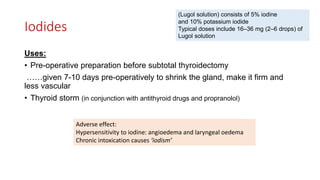
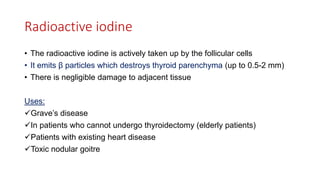
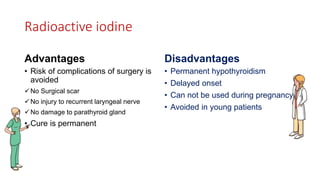
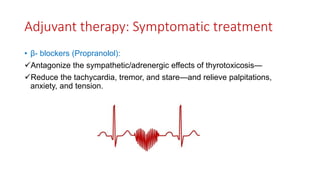
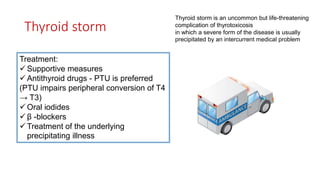
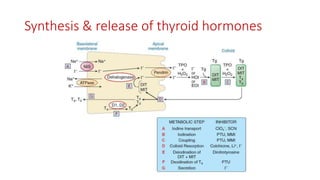
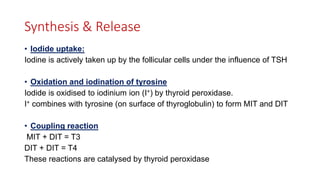
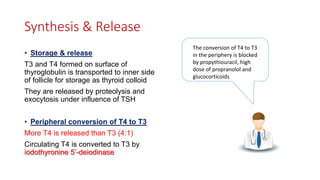
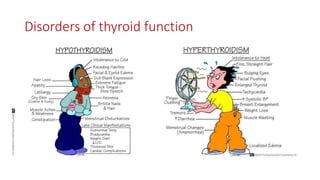
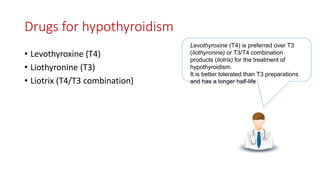
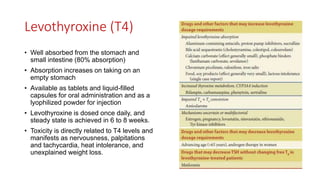
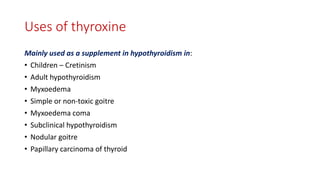
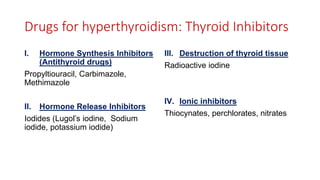
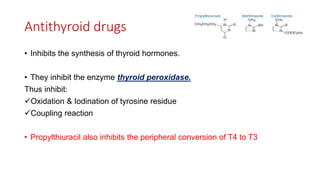
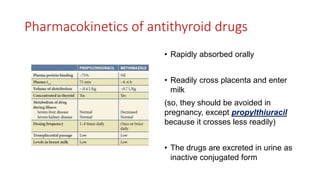
Thyroid hormones are essential for normal development and metabolic homeostasis. Their synthesis involves iodine uptake, oxidation and coupling reactions catalyzed by thyroid peroxidase. T4 and T3 are stored and released from the thyroid gland under TSH influence. Levothyroxine is the preferred treatment for hypothyroidism as it has a longer half-life. Antithyroid drugs like methimazole and propylthiouracil inhibit thyroid peroxidase to treat hyperthyroidism. Radioactive iodine is also used which is taken up and destroys the thyroid gland. Symptomatic treatments include beta blockers.



![Uses of antithyroid drugs
• To achieve spontaneous remission and control in:
Grave’s disease
Toxic nodular goitre
• Used prior to radioactive iodine
• Pre-operative control of hyperthyroidism
• Thyroid storm
(PTU is preferred because it can
inhibit peripheral conversion)
Methimazole is
preferred over PTU
because of
once daily dosing
(longer t ½ )
Lower incidence of
adverse effects
[Except in pregnancy: PTU
is preferred]](https://image.slidesharecdn.com/thyroidantithyroiddrugs-201011191918/85/Thyroid-amp-antithyroid-drugs-15-320.jpg)