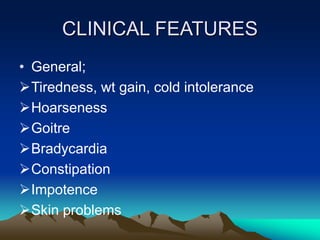
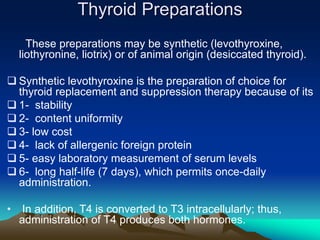
Hyperthyroidism is caused by excess thyroid hormones due to conditions like Graves' disease. It causes symptoms like weight loss, rapid heart rate, nervousness, and eye changes. Treatment options include antithyroid drugs which suppress hormone production, radioactive iodine which destroys the gland, and surgery. Hypothyroidism is caused by insufficient hormone levels and results in fatigue, weight gain, constipation, and intolerance to cold. Levothyroxine replacement is the standard treatment.