1) Thoracic outlet syndrome occurs when the space through which the neurovascular bundle passes from the neck to the armpit is too narrow, compressing the structures.
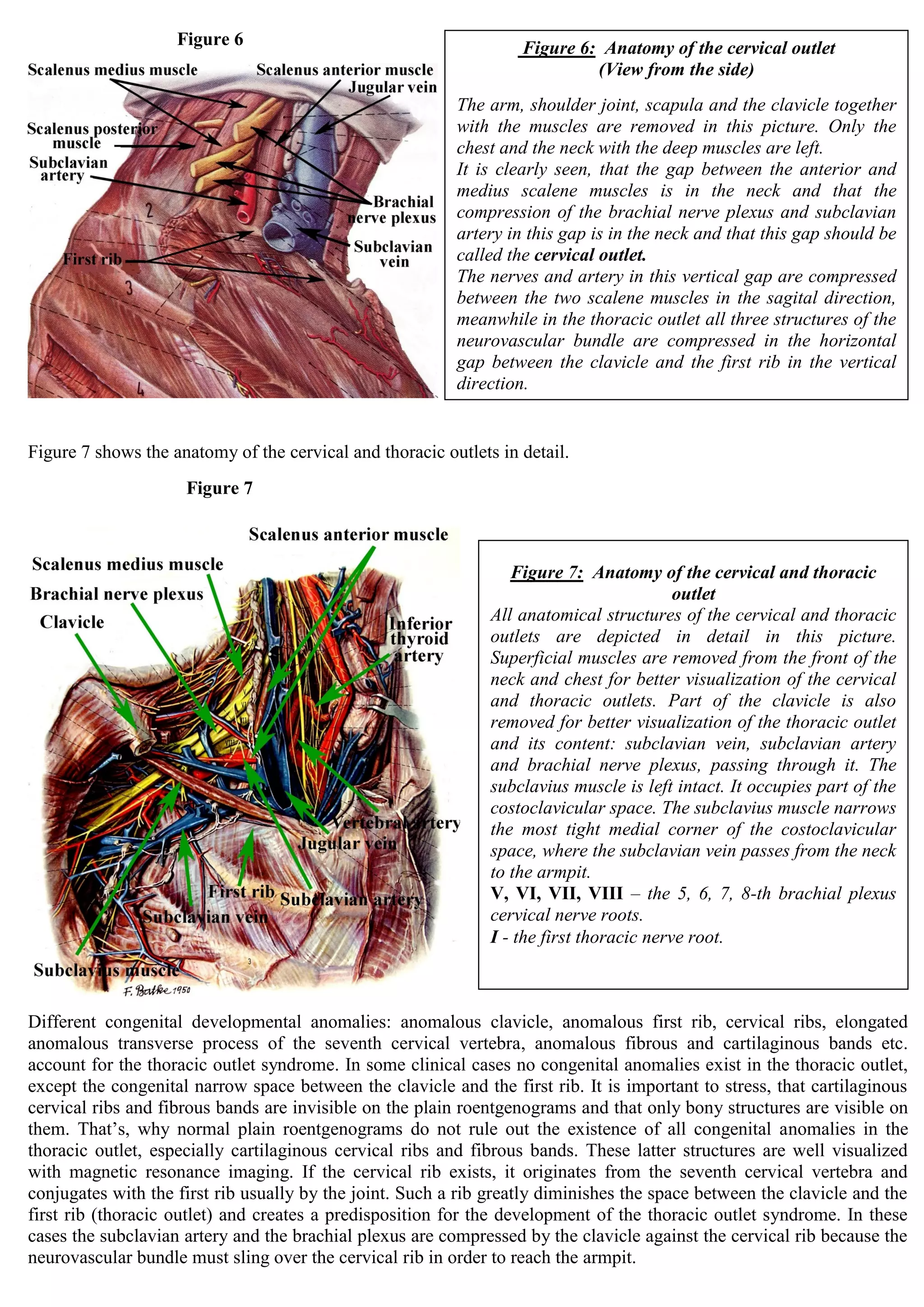
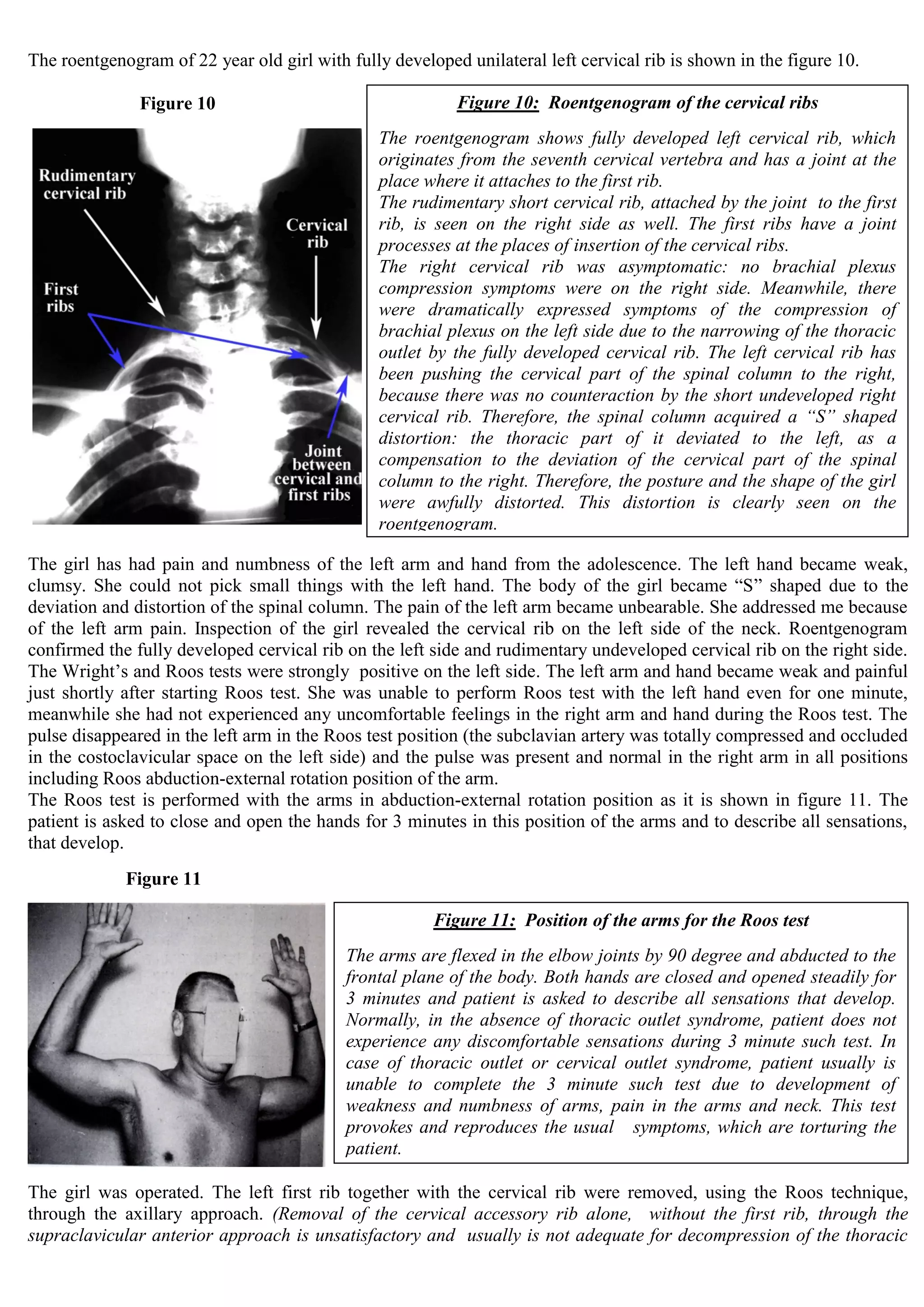
2) The main anatomical structures limiting this space are the clavicle, first rib, and scalene muscles. Compression can occur in the costoclavicular space or cervical outlet.
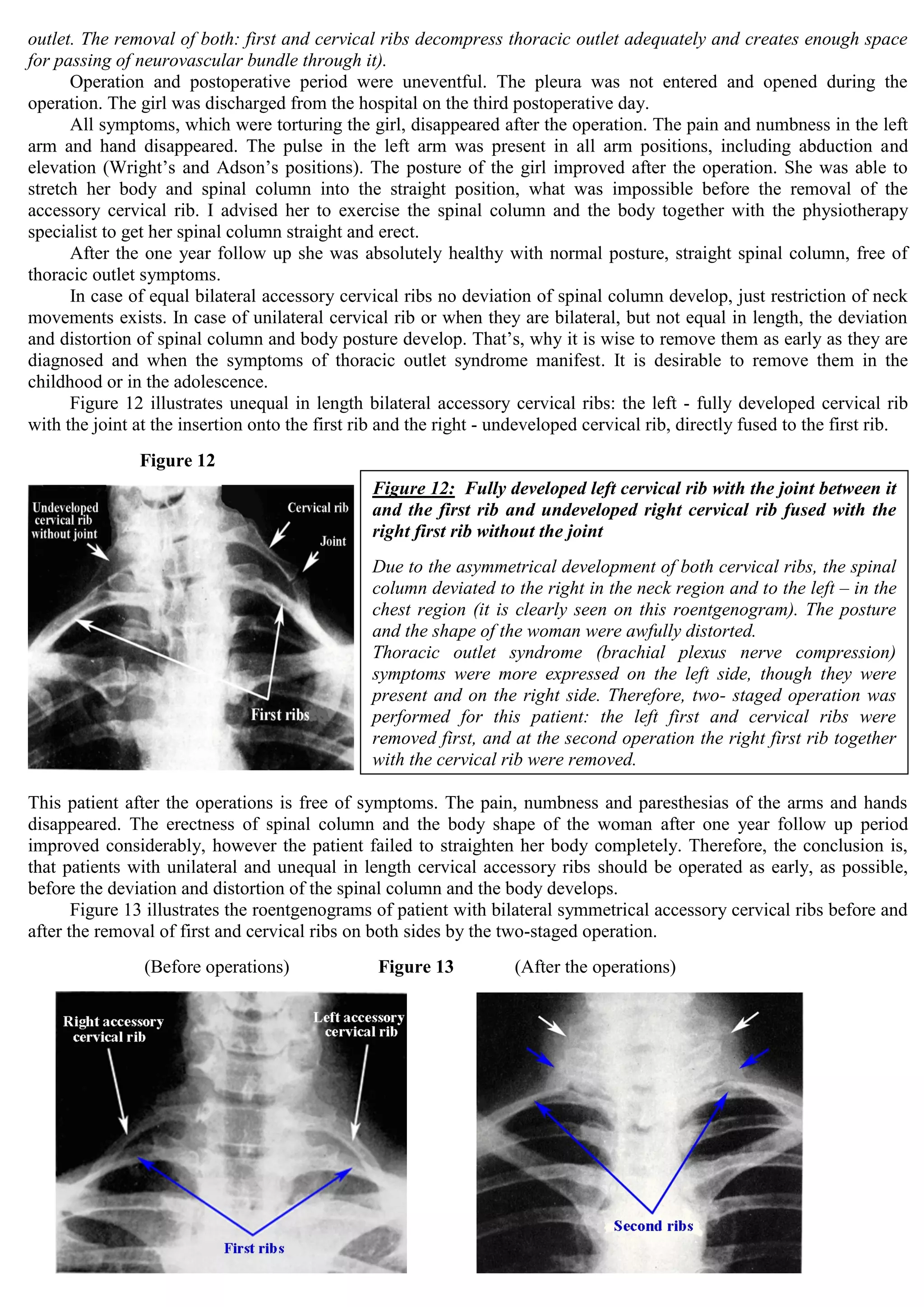
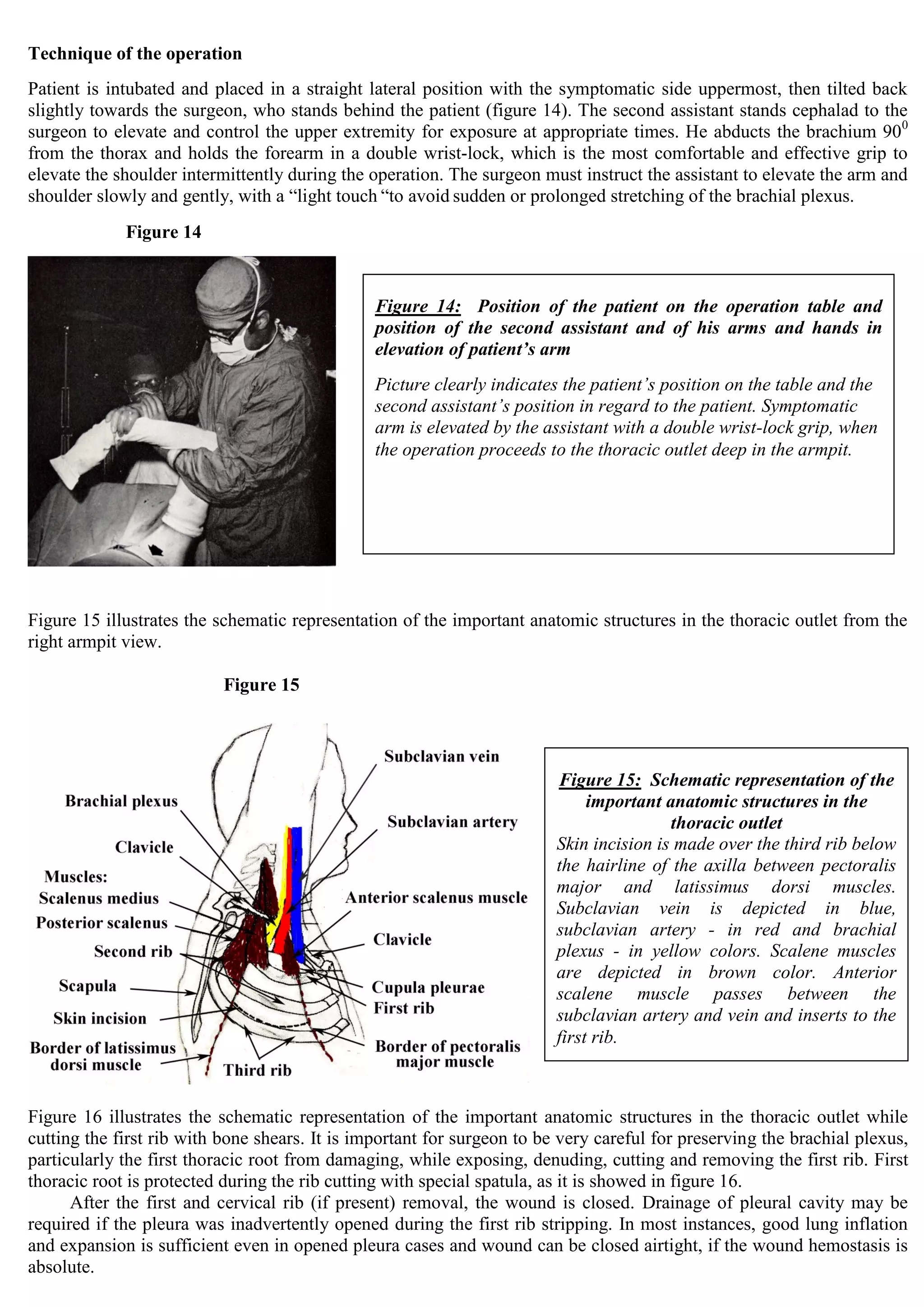
3) Symptoms vary depending on the location of compression but may include pain, numbness, and neurological deficits in the arm as well as vertebrobasilar insufficiency. Surgical treatment by scalenectomy can provide relief.