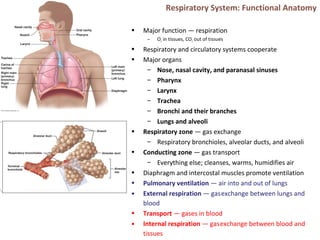
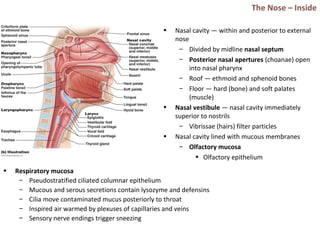
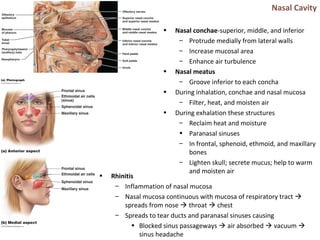
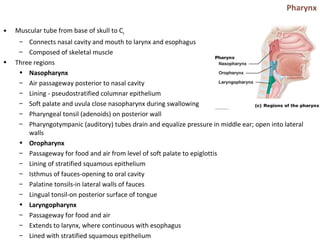
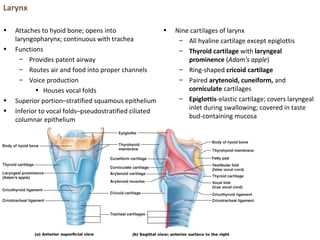
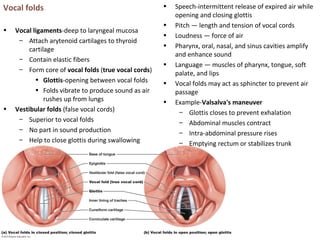
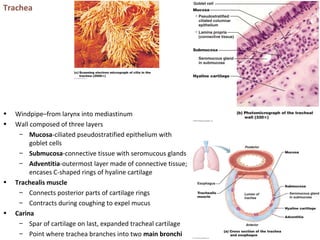
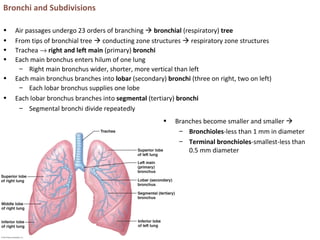
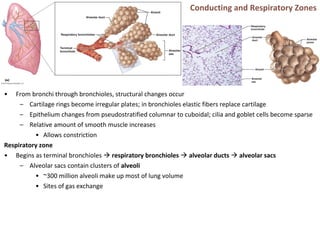
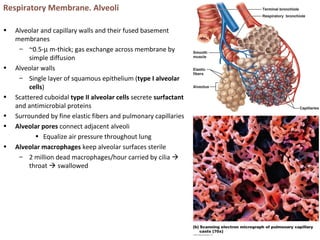
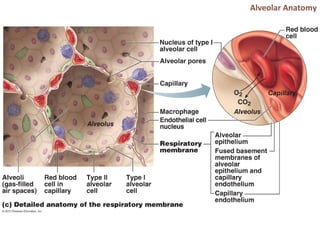
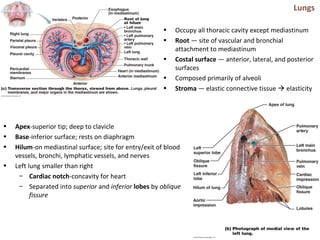
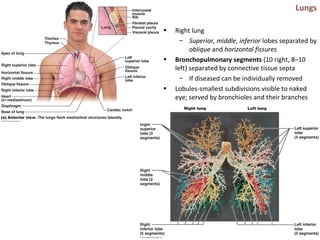
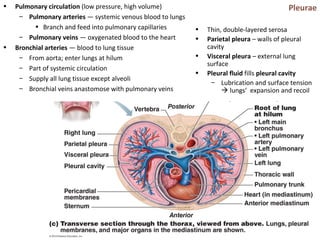
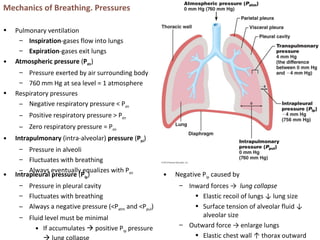
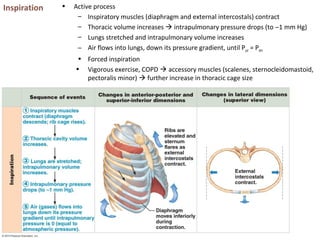
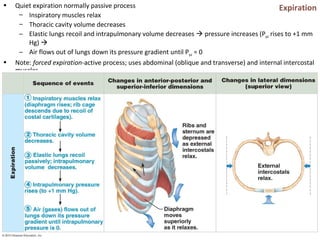
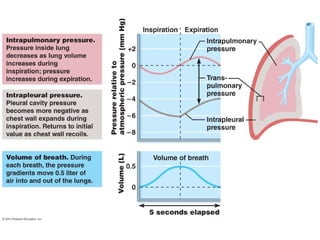
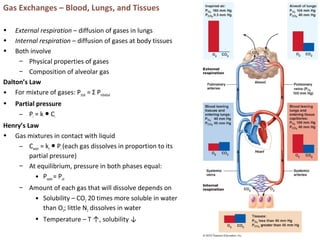
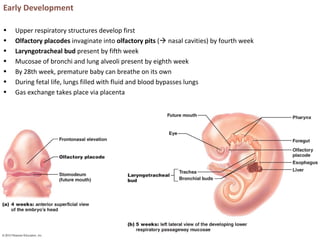
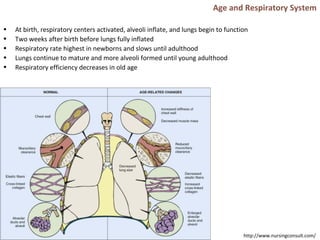
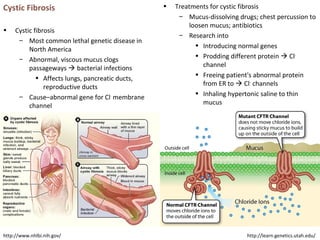
The respiratory system functions to oxygenate tissues and remove carbon dioxide. It includes the nose, pharynx, larynx, trachea, bronchi, lungs, and diaphragm. In the nose, nasal hairs and mucus filter air which is warmed and humidified. The pharynx connects the nasal cavity to the larynx and esophagus. The larynx contains vocal cords and cartilage that protect the airway and enable speech. The trachea branches into bronchi which further divide into bronchioles ending in alveoli in the lungs where gas exchange occurs. Breathing is driven by changes in intrapleural pressure caused by the diaphragm and chest wall expanding and contracting the