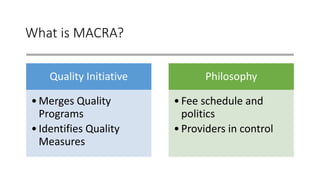
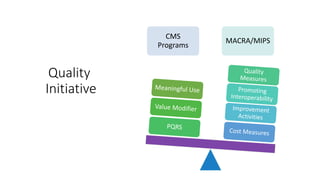
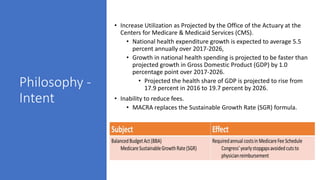
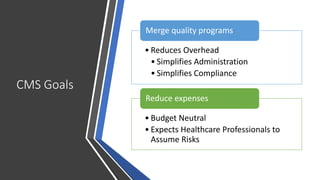
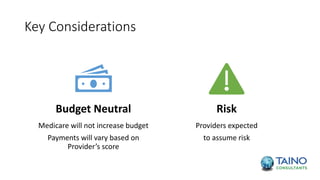
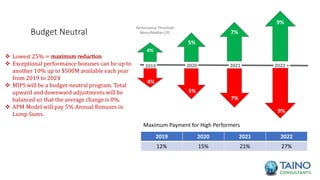
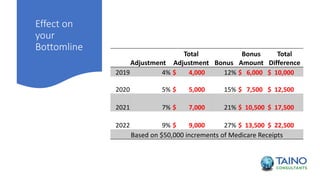
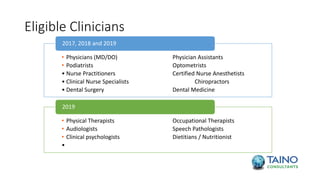
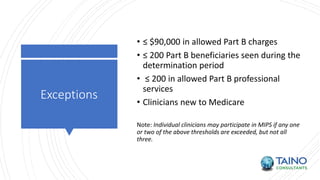
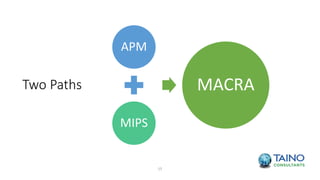
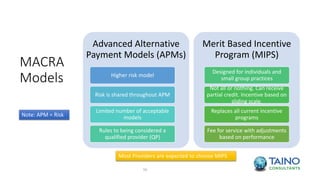
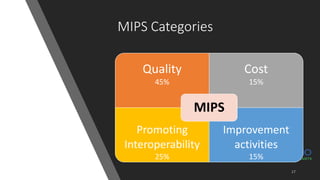
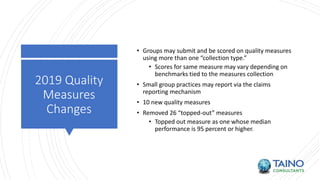
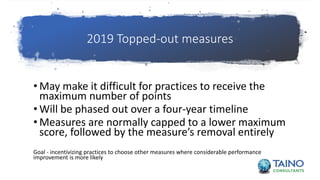
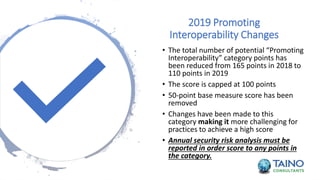
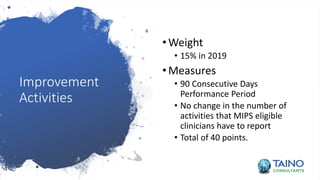
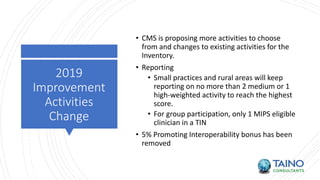
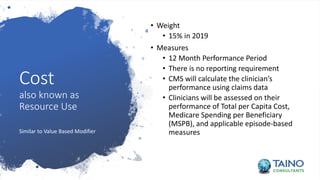
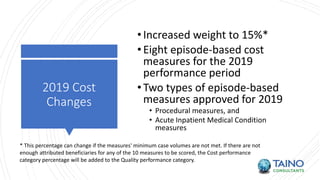
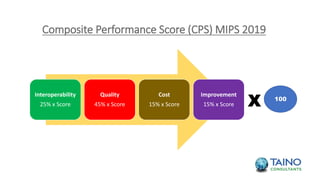
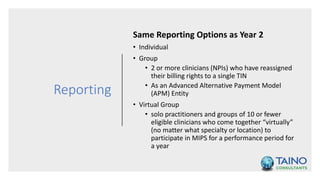
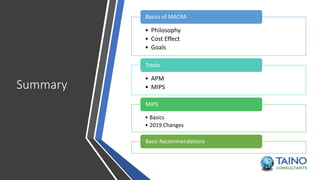
The document provides an overview of MACRA (Medicare Access and CHIP Reauthorization Act), focusing on its significance as a quality initiative that merges existing quality programs and emphasizes on shifting risk to healthcare providers. It outlines key components such as MIPS (Merit-based Incentive Payment System), its performance categories, and projected payment adjustments from 2019 to 2022. Additionally, it highlights the goals of reducing overhead and simplifying compliance while encouraging improved patient care through quality measures.