1) Telenursing in the Intensive Care Unit (ICU) involves using telecommunication technologies to remotely monitor critically ill patients and support bedside healthcare teams.
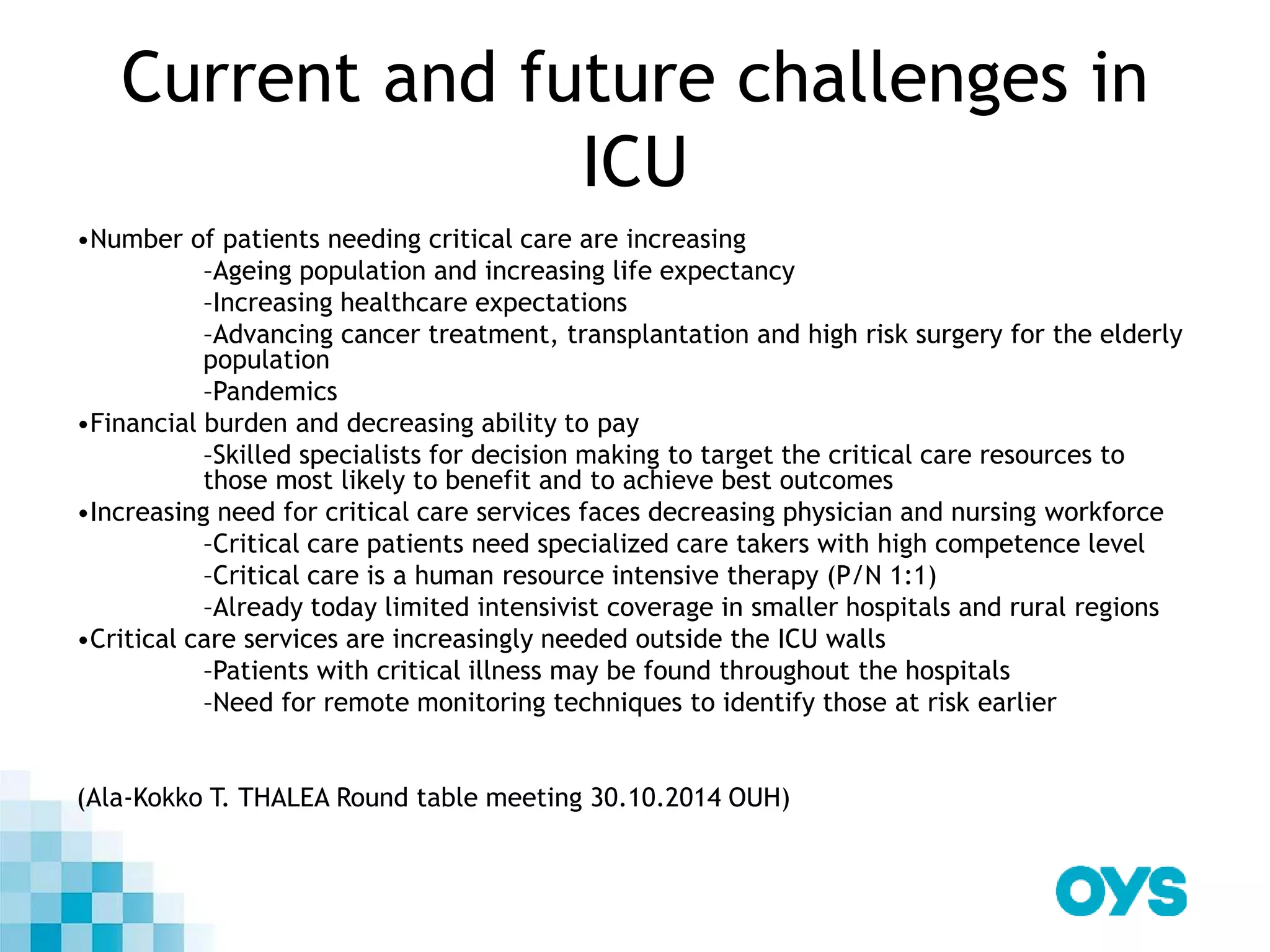
2) The number of patients requiring critical care is increasing due to an aging population and advanced treatments, yet resources are decreasing. Tele-ICU aims to address these challenges by providing remote monitoring and expertise from ICU specialists.
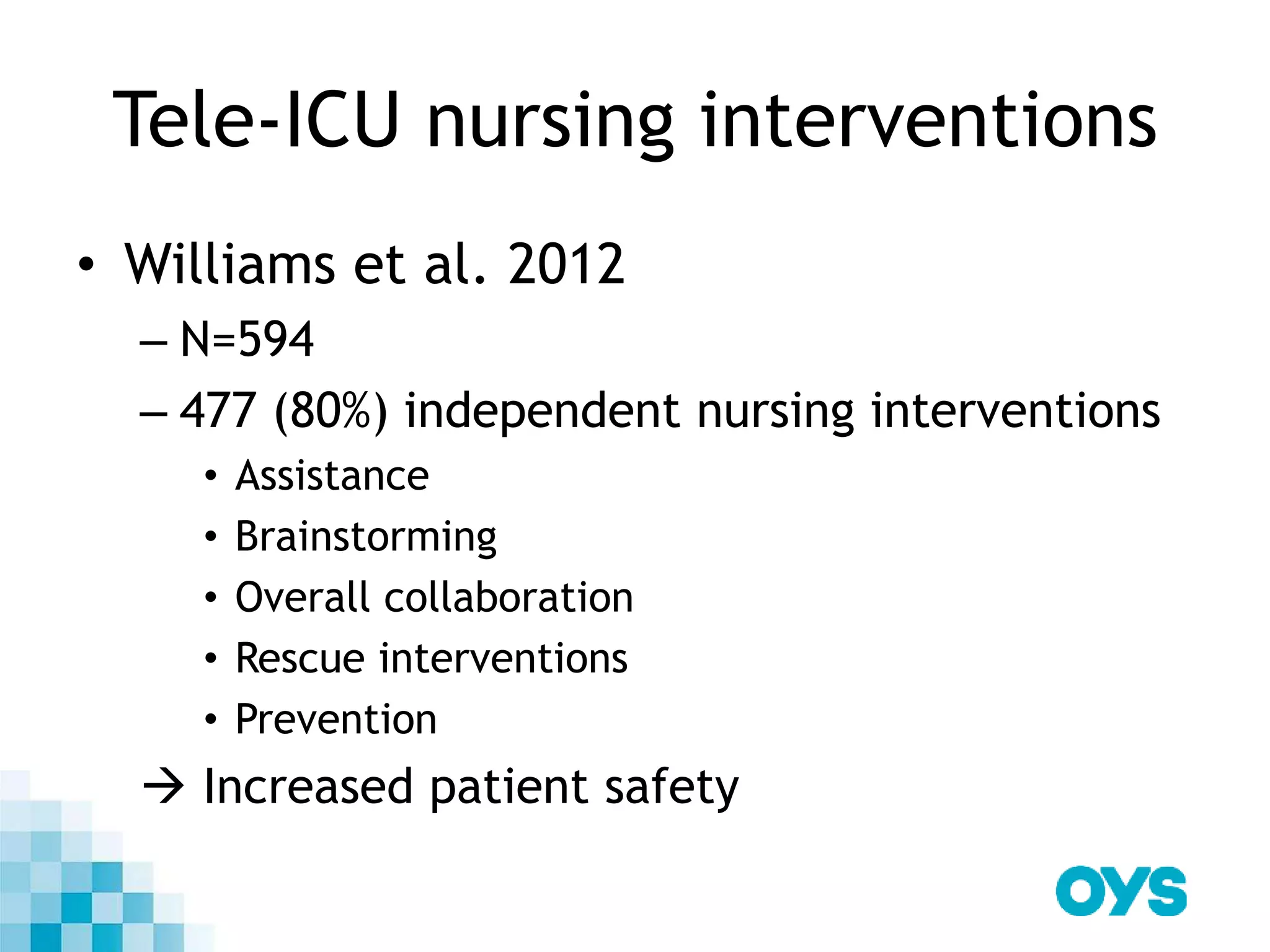
3) Studies have found tele-ICU can reduce ICU and hospital length of stays and mortality while increasing compliance with best practices. Tele-ICU nurses monitor patients, collaborate with bedside staff, and ensure best practices are followed to increase patient safety.