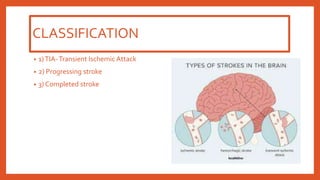
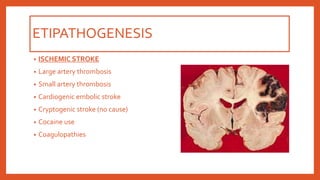
The document discusses types of strokes, defining transient ischemic attacks, progressing strokes, and completed strokes, alongside their respective symptoms and potential outcomes. It covers the pathophysiology of ischemic strokes, including various causes such as large artery thrombosis and cardiogenic embolism, as well as hemorrhagic strokes like intracerebral and subarachnoid hemorrhages. The document also addresses the gross and microscopic morphology of stroke-related tissue changes.