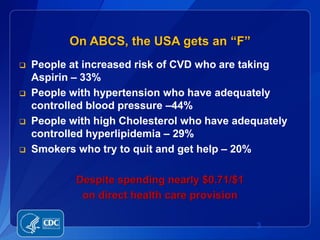
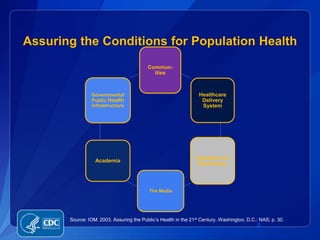
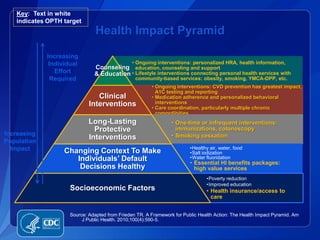
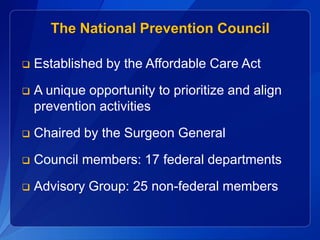
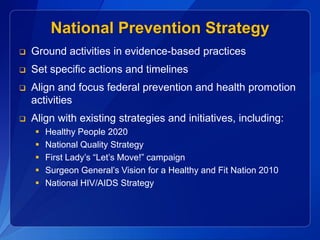
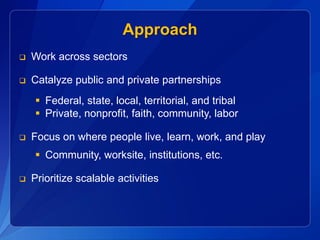
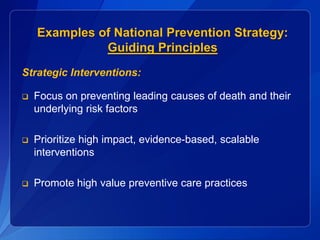
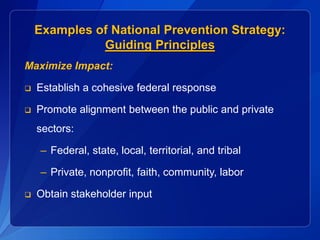
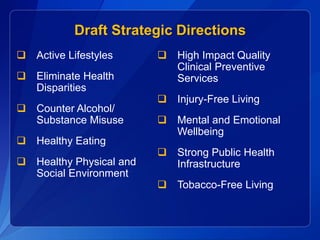
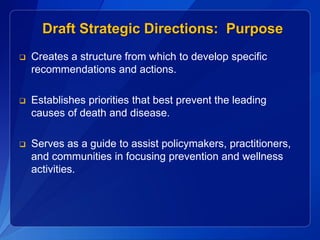
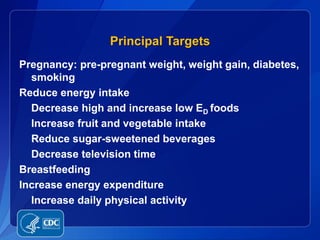
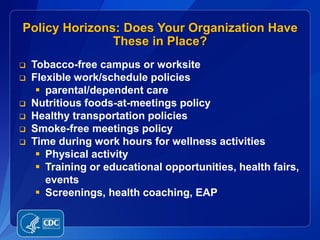
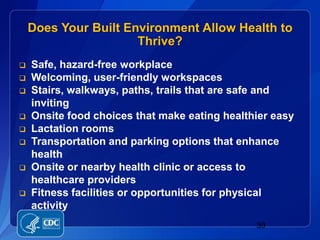
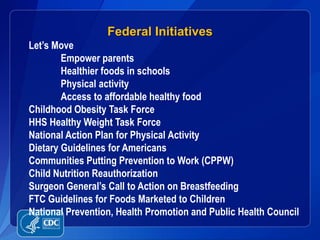
This document discusses strategies to promote population health in the United States. It provides data showing poor control of health conditions like high blood pressure and cholesterol. It also discusses how employers can play a key role in wellness since most Americans get health insurance through work. The document proposes several strategic directions for a National Prevention Strategy including promoting active lifestyles, healthy eating, strong public health infrastructure, and making clinical preventive services more accessible. It seeks input on draft strategic directions to guide federal prevention activities.