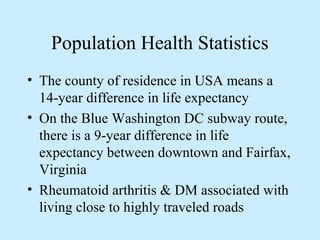
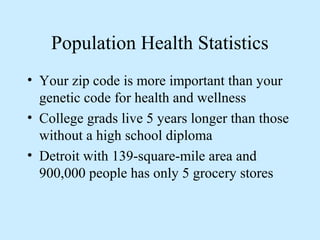
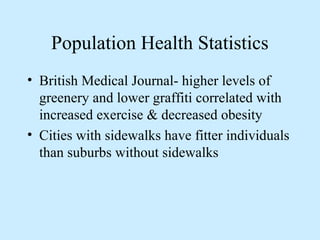
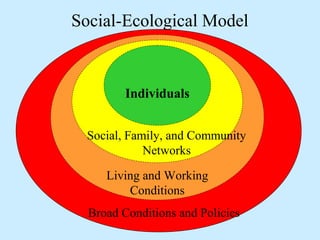
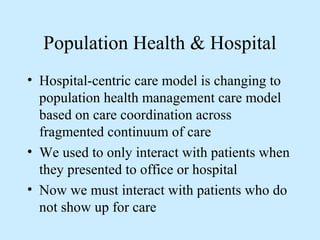
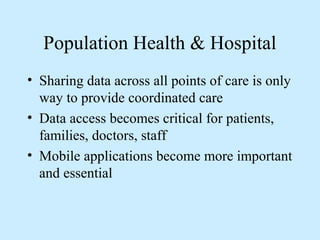
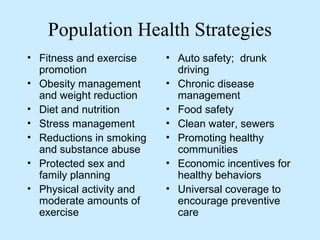
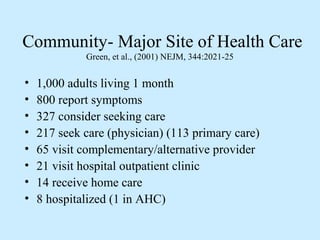
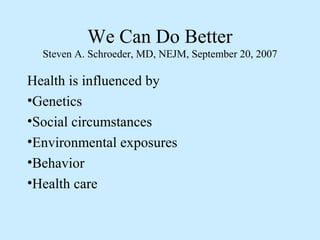
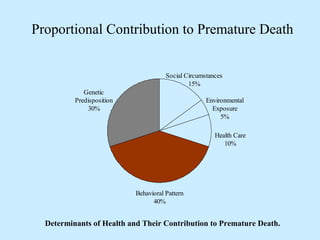
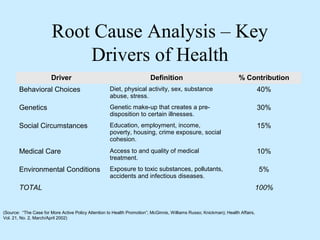
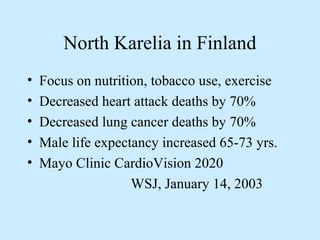
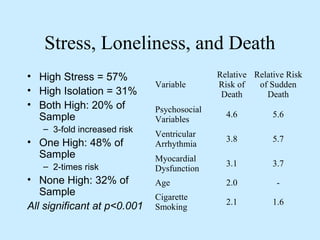
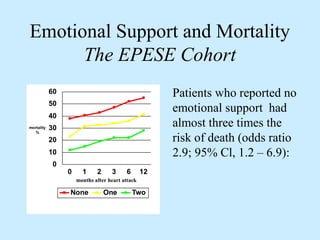
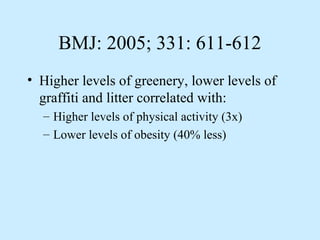
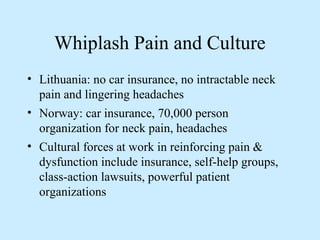
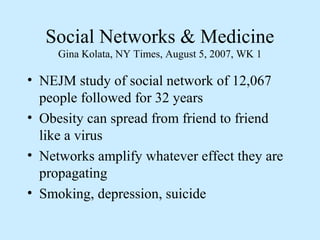
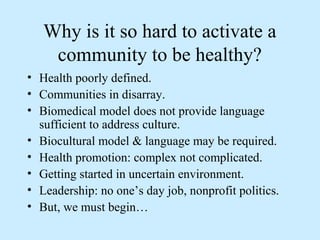
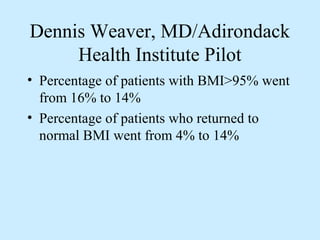
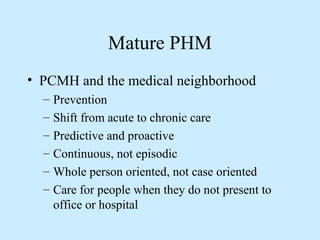
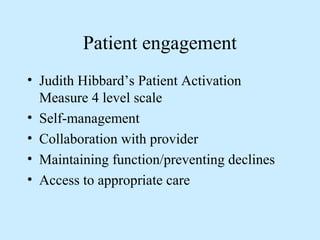
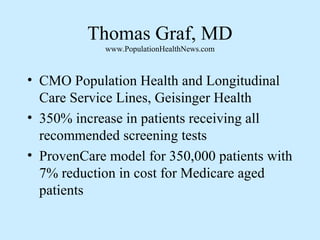
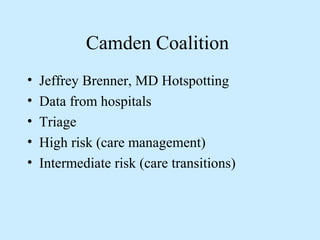
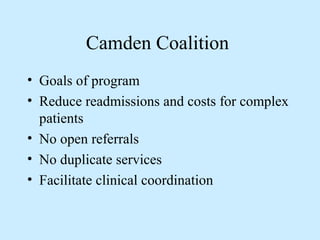
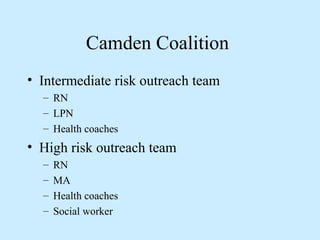
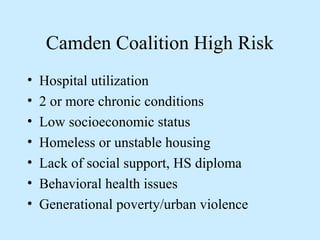
The document discusses the importance of population health management, emphasizing how social, environmental, and behavioral factors significantly influence health outcomes. It highlights various statistics illustrating disparities in health based on geography, education, and community resources, while advocating for a shift from hospital-centric care to coordinated population health strategies. Ultimately, it calls for collaboration among healthcare providers and non-medical organizations to address the multiple determinants of health.