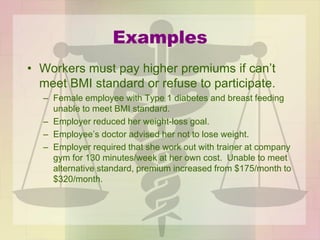
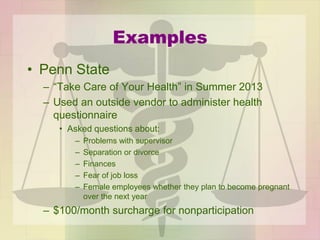
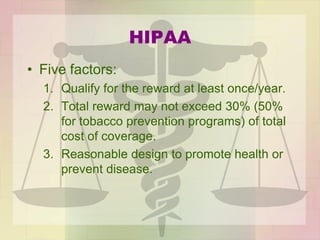
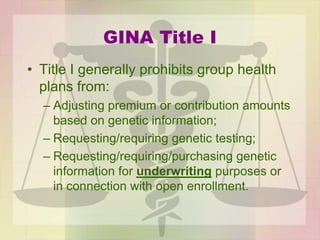
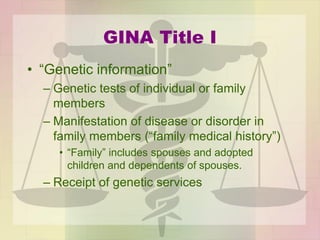
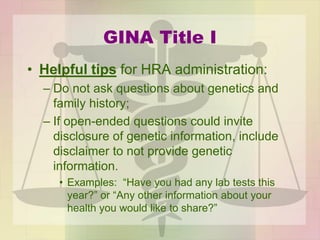
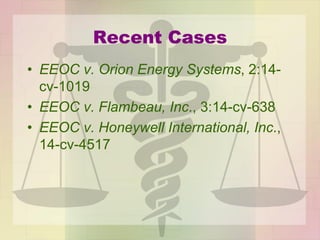
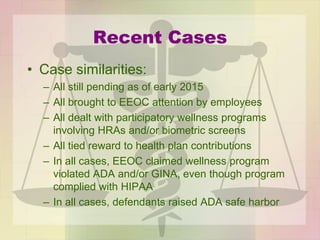
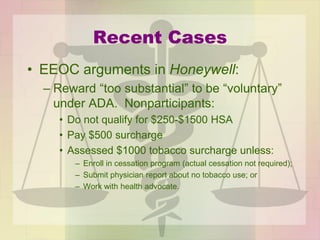
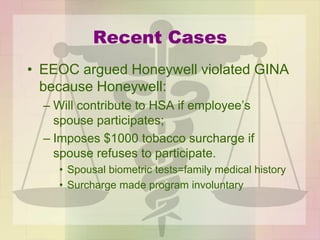
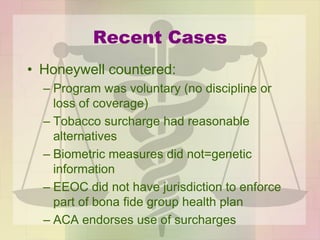
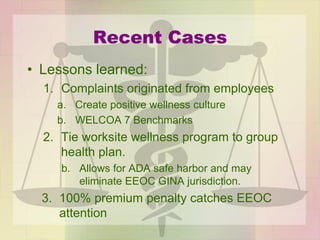
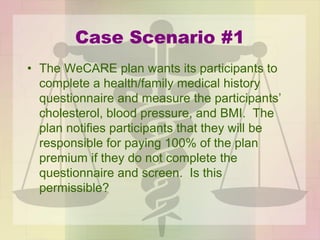
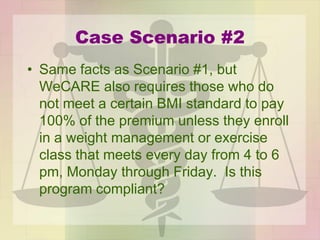
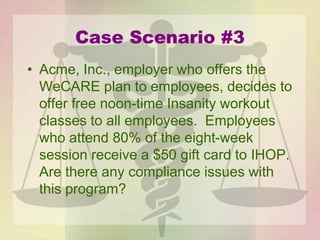
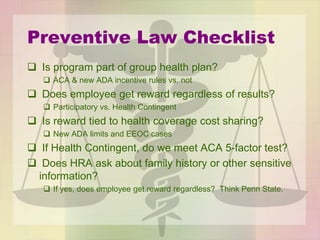
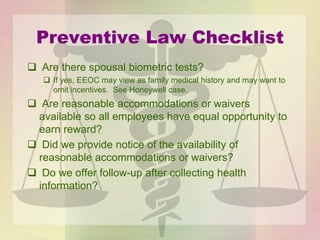
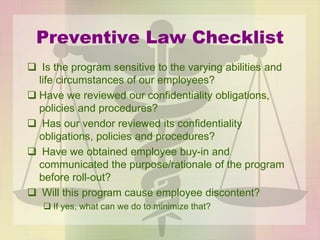
The document discusses the legal framework surrounding workplace wellness programs, focusing on compliance with laws such as HIPAA, ACA, ADA, EEOC, and GINA. It outlines the implications of these laws on program design and employee participation, emphasizing the need for inclusivity and non-discrimination while providing guidelines and case scenarios for compliance. A preventive law checklist is also included to assist employers in evaluating their wellness program policies.