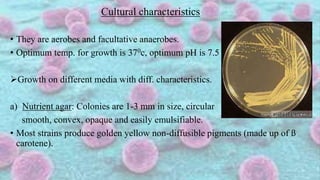
The document provides an overview of Staphylococcus, specifically Staphylococcus aureus, detailing its classification, morphology, cultural characteristics, biochemical reactions, pathogenesis, and associated infections. It highlights its pathogenic mechanisms, including colonization, invasion, evasion of host defenses, and the diseases it can cause such as cutaneous infections, food poisoning, and toxic shock syndrome. Laboratory diagnosis methods from sample collection to tests like coagulase for differentiation are also described.