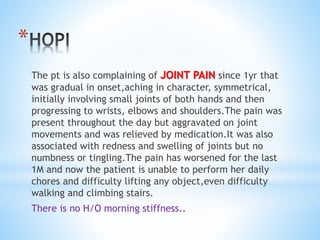
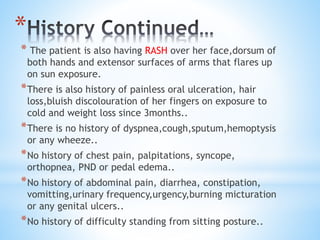
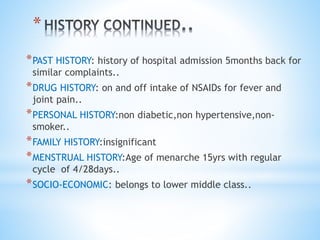
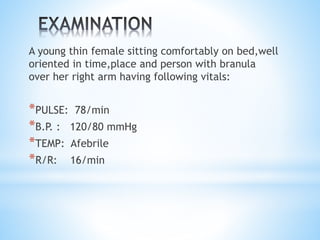
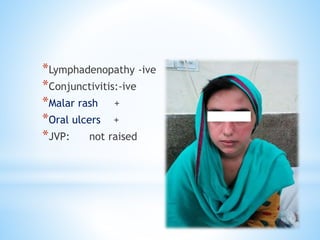
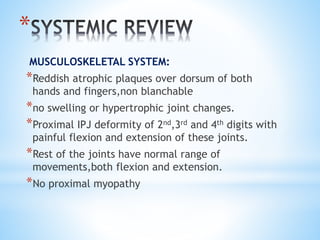
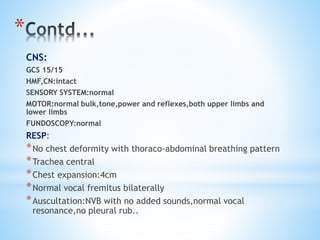
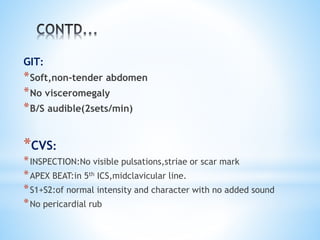
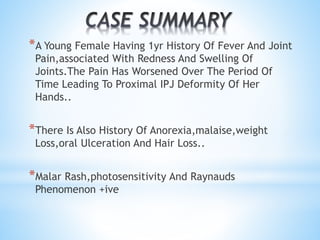
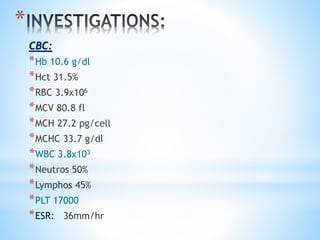
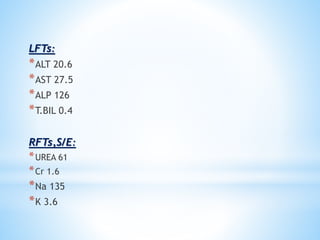
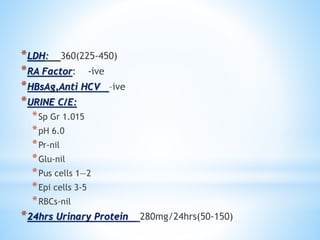
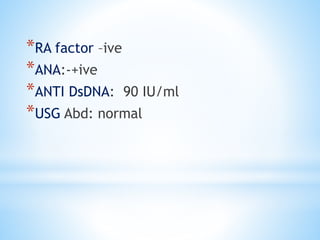
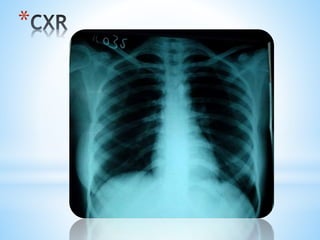
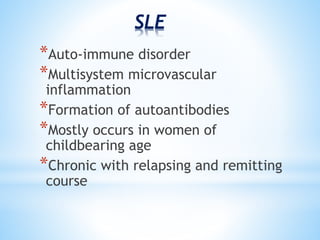
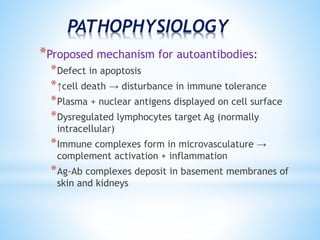
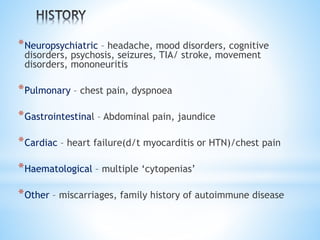
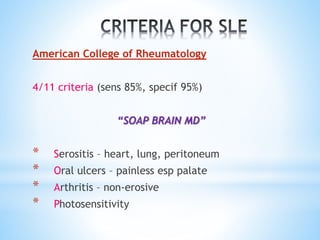
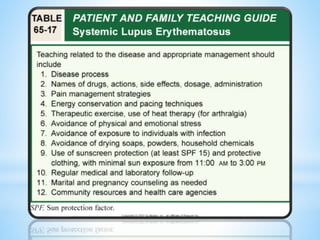
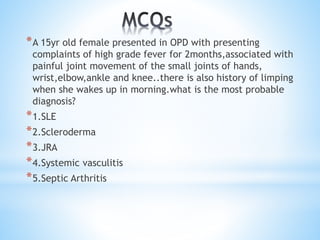
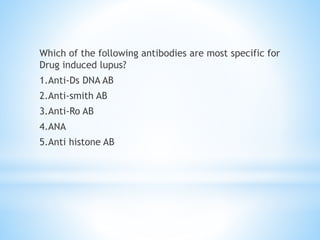
A 18-year-old female presented with 1 year history of fever, joint pain affecting small joints and progressing to larger joints, rash, oral ulcers, hair loss, and weight loss. Examination found malar rash, joint swelling and deformity, and positive photosensitivity and Raynaud's phenomenon. Tests showed positive ANA and anti-dsDNA antibodies. The presentation is most consistent with systemic lupus erythematosus.