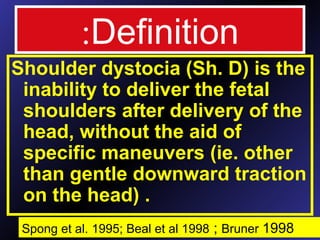
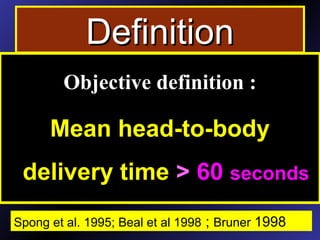
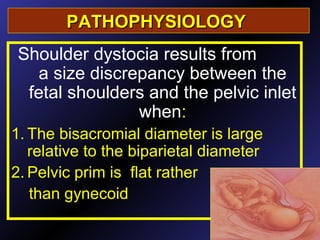
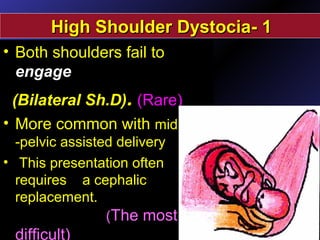
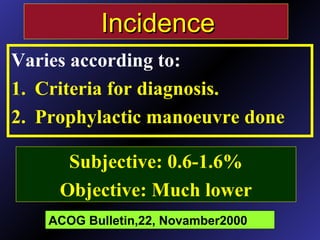
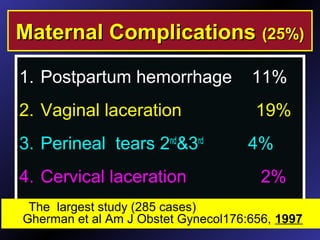
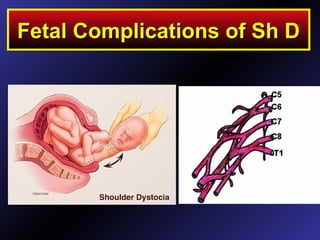
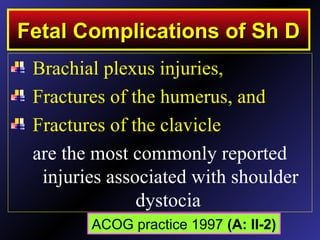
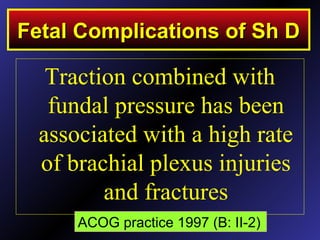
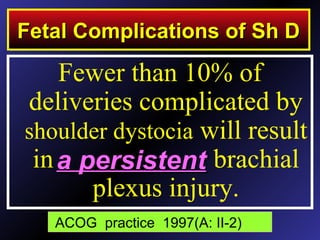
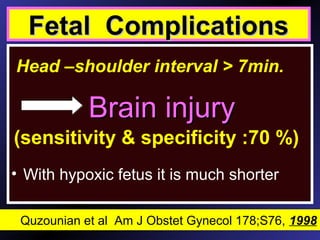
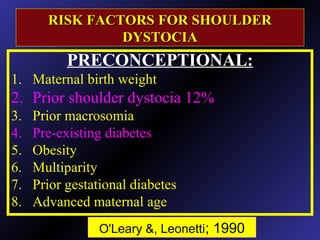
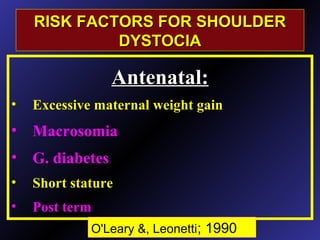
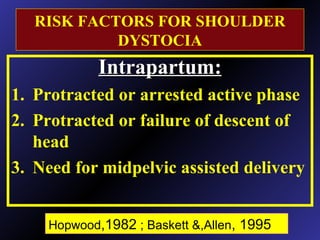
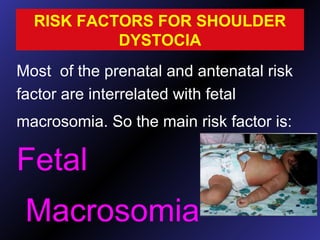
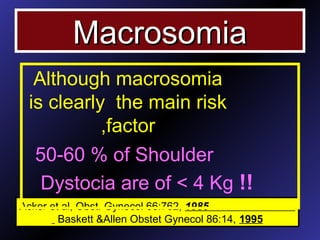
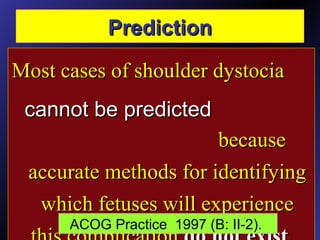
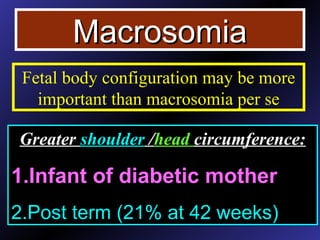
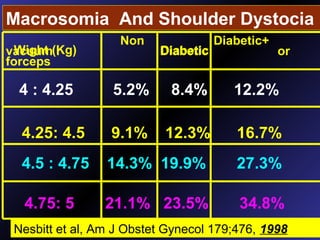
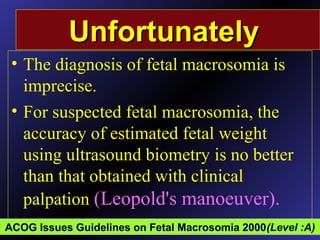
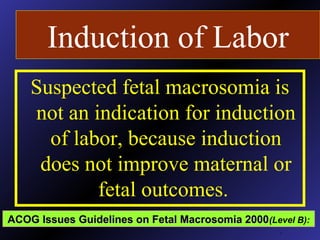
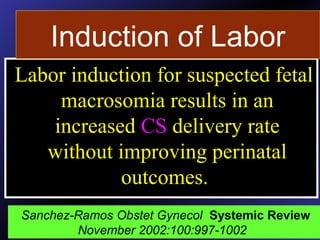
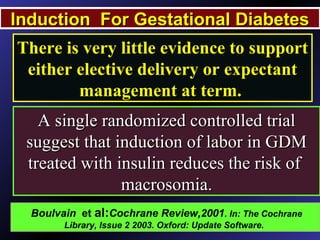
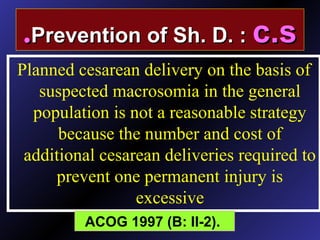
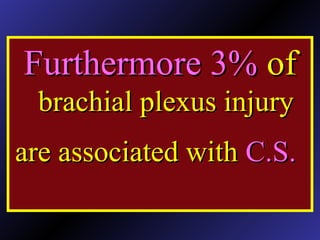
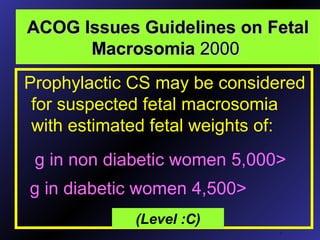
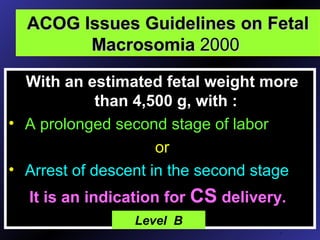
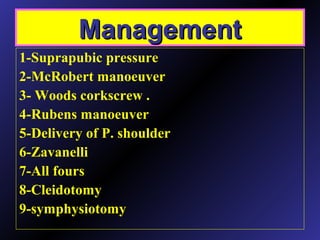
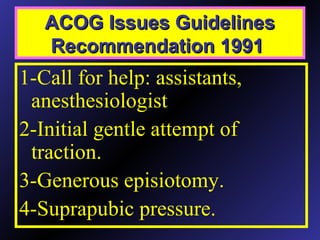
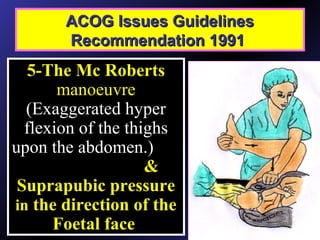
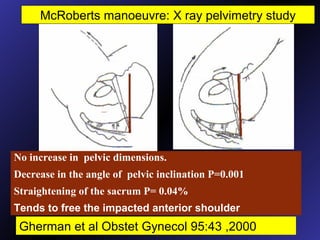
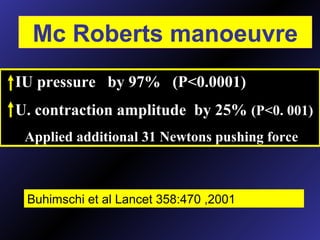
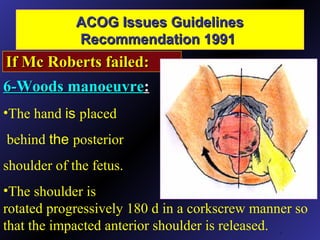
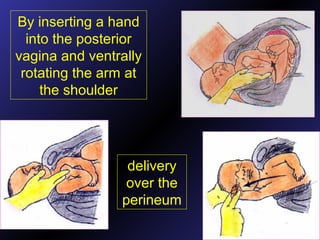
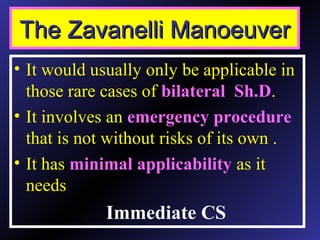
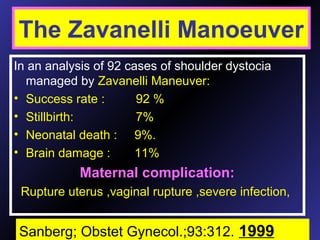
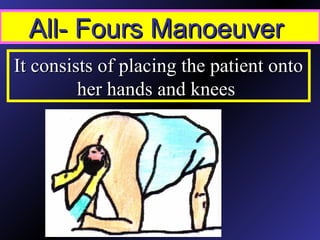
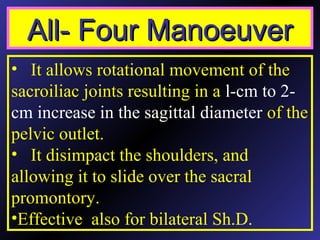
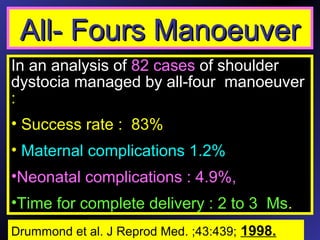
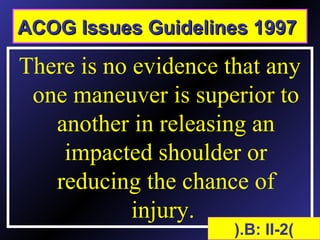
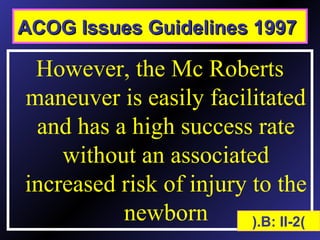
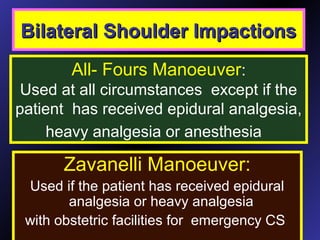
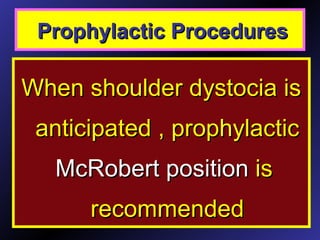
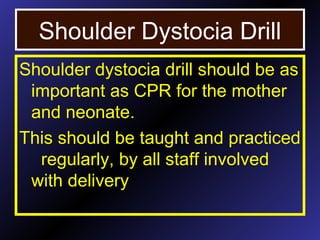
This document discusses shoulder dystocia, an obstetric emergency where the fetal shoulders do not deliver easily after the head is delivered. It defines shoulder dystocia and outlines risk factors such as macrosomia. It examines techniques to predict, prevent, and manage shoulder dystocia. While macrosomia is a main risk factor, shoulder dystocia is difficult to predict accurately. Prophylactic induction of labor or cesarean delivery for suspected macrosomia is not routinely recommended. Standard management techniques for shoulder dystocia include McRoberts maneuver, suprapubic pressure, and delivery of the posterior arm.