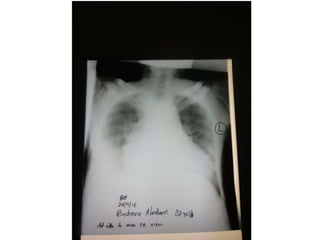
This case presentation is for an 82-year-old man with a history of chronic congestive heart failure (CCF) and chronic kidney disease (CKD) who presented with sharp left-sided chest pain, abdominal fullness, difficulty swallowing and breathing over the past 5 days. He has a history of lower limb swelling and blisters. Differential diagnoses include heart attack, myocardial infarction, pulmonary edema and pleural effusion. On examination, he appears sick and is lying in left lateral position. Vitals are stable. Lungs have wheezing and heart has murmurs. Lower limbs have edema and ulcer. Investigations include chest X-ray, ECG, urinalysis and CBC. He is started
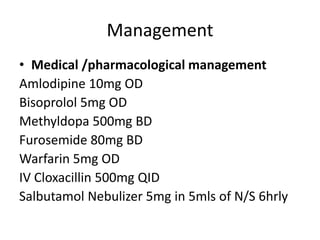
![General examination
• Head to toe
We examined a sick looking old man in bed lying in
left lateral position with the head slightly raised.
The hair is well distributed, eyes are symmetrical to
each other and no discharge from the ear, eyes and
nose. There is no yellowing of the sclera and the
skin, no pallor of the conjunctiva, palms and soles,
no bluishness of the mucous membranes and the
extremities, no finger clubbing, no lymph node
swelling, and no signs of dehydration but however
there is swelling of both lower limbs with some
blisters and an ulceration on the right lower leg.
[AVPU]-A](https://image.slidesharecdn.com/casepresentationaip1-230703063436-98f050be/85/CASE-PRESENTATION-AIP-1-pptx-14-320.jpg)
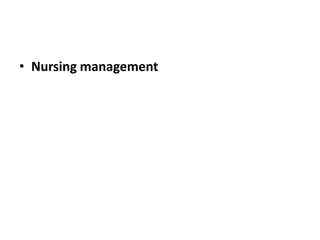
![• Vital observations during clerking
Bp=106/76mmHg [systolic(90-120),diastolic(60-90)]
Axillary temp=36.2oC [35.5-37.2oC]
Pulse= 74b/m[60-100]
SO2=95%[95-100]
RR=20c/m
• Anthropometric measurements
Weight= 63 kgs
Height= ???](https://image.slidesharecdn.com/casepresentationaip1-230703063436-98f050be/85/CASE-PRESENTATION-AIP-1-pptx-15-320.jpg)