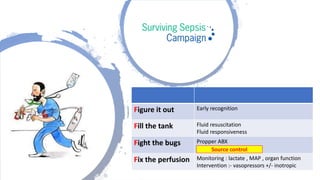
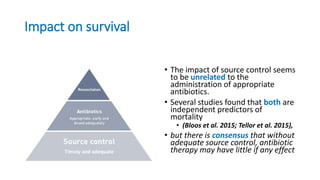
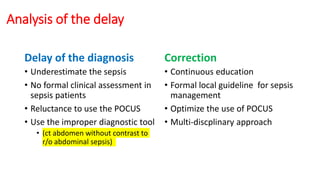
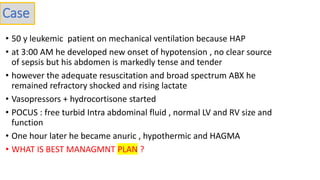
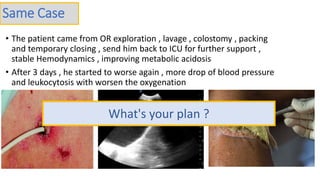
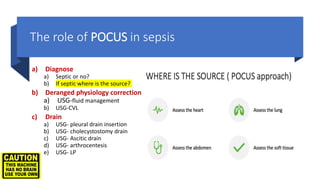
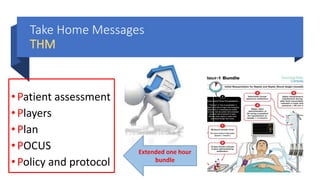
The document discusses optimizing source control for sepsis patients. It recommends:
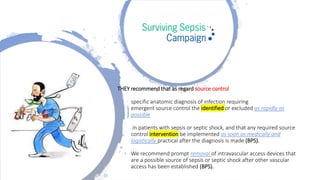
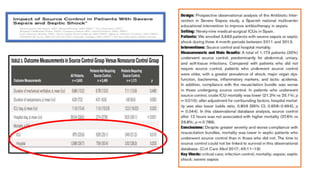
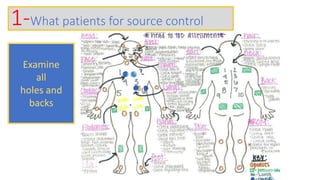
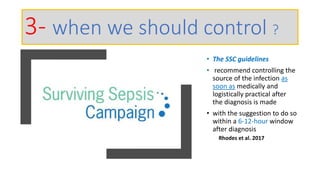
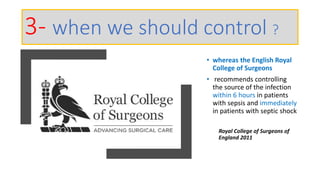
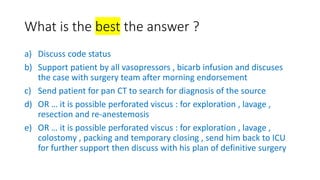
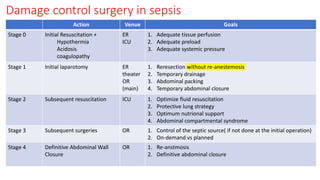
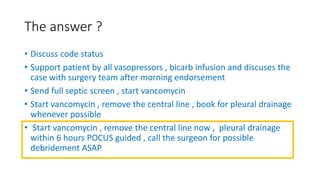
1) Identifying and controlling the source of infection as soon as possible after diagnosis, within 6-12 hours for sepsis patients and immediately for septic shock patients.
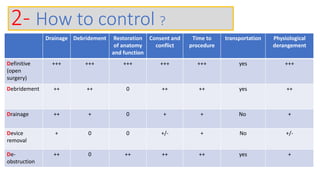
2) Drainage, debridement, restoration of anatomy and function are ideal source control methods when possible and as soon as medically and logistically practical.
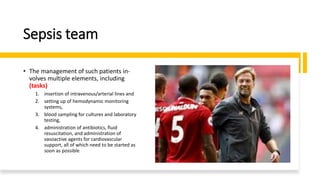
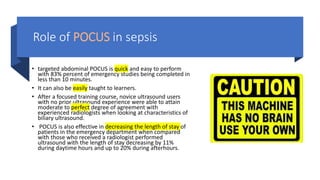
3) A sepsis team approach involving multiple specialties working together improves management and reduces delays in source control and other essential treatments.