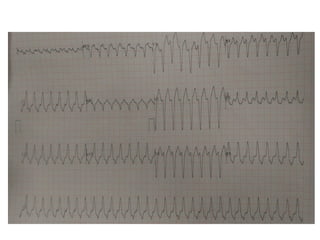
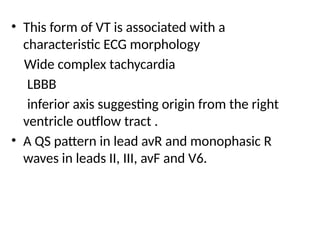
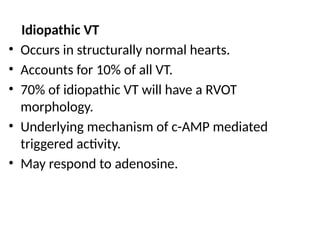
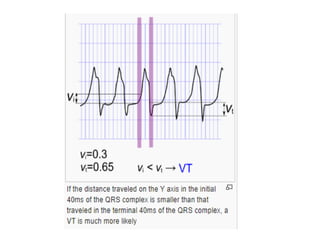
A 60-year-old female with a history of ventricular tachycardia (VT) presented with shortness of breath and palpitations after discontinuing her medication. The ECG showed right ventricular outflow tract (RVOT) VT identified by its characteristic morphology, and the patient was successfully treated with synchronized DC shock. RVOT tachycardia is typically benign and may respond to acute interventions or long-term therapies; it accounts for 10% of all VT cases.